Contents
1 Introduction
Advance care planning involves offering people opportunities to consider and discuss their future care and support needs and make plans while they have capacity to make decisions. It may involve appointing an advocate, which can increase the chances of the person’s wishes being known and respected.
Opportunities to discuss advance care plans should be offered to people at risk of losing capacity (for example through progressive illness), as well as those who have fluctuating capacity (for example through mental illness). If people do not want to speak about their future needs and care arrangements, this should be respected and clearly recorded. However, people should know that they can discuss these whenever they wish. Reviewing and updating existing advance care plans regularly ensures that the recorded wishes stay valid, applicable and true to the person.
Usually a person is able to discuss care and treatment options when they are unwell, and a joint decision can be made about future care and treatment options. When an adult has capacity, they can refuse treatment and it cannot be given without a person`s valid consent except for some circumstances under the Mental Health Act 1983.
Communication is the key to the provision of safe and effective care and is essential whether this is before capacity is lost and a person is considering their future, when capacity is diminished or fluctuating, and with relatives, carers, advocates and the care team when capacity is lost.
There are occasions when a person is unable on a temporary or permanent basis to communicate their wishes and consent to or refuse treatment.
The Mental Capacity Act 2005 (MCA) provides the legal framework for acting and making decisions on behalf of individuals who lack capacity to make particular decisions for themselves.
It includes many provisions to protect the rights of those who lose capacity to make decisions and provides several ways that people can influence what happens to them if they are unable to make a particular decision in the future including:
- advance statements: expressions of wishes and feelings
- advance decision to refuse medical treatment (ADRT)
Rotherham Doncaster and South Humber NHS Foundation Trust (the Trust) acknowledge that it is the right of every competent adult patient to influence their care and treatment and that advance statements and advance decisions to refuse treatment (ADRT) provide an opportunity to support autonomy, shared decision making and the recovery process.
In striving to achieve a more balanced partnership between patients and health and social care professionals the trust has developed this policy. Its aim is to assist and guide those patients who wish to plan for their future care and provide clear guidance to those health professionals responsible for delivering such care.
Making decisions in advance with patients might help to ensure that the care a person receives is the care that he or she would want in certain circumstances. This policy provides a framework for the effective support of this process and the trust actively encourages all patients to plan ahead.
This policy should be read in conjunction with the MCA 2005 and the MCA Code of Practice (2007). It is not a substitute for the MCA and the Code of Practice, to which all professionals must adhere.
This policy assumes a knowledge and understanding of the trust’s MCA Mental Capacity Act 2005 policy and should be read in conjunction with it.
Other trust policies to be read in conjunction with this policy are:
- Consent to care and treatment policy
- Mental Health Act 1983
Professionals must act with due care and attention and may be legally liable if they disregard a valid and applicable ADRT.
2 Purpose
The purpose of this policy is to ensure that wherever possible, patients in receipt of care from Rotherham Doncaster and South Humber NHS Foundation Trust (the trust) will have their expressed wishes in an advance statement and legal rights that are contained in an advance decision to refuse treatment (ADRT) respected and upheld where they are valid and applicable.
The trust is committed to ensuring that all patients within the trust who are using our services are treated with dignity and respect and individuals and their families or carers receive appropriate care and support. This includes encouraging patients aged 16 and over to set out their wishes in advance and encouraging collaboration to discuss advance care planning at each review.
2.1 Definitions
The definitions set out here are to ensure clarity, as there are a number of terms to describe advance statements that are often used interchangeably, sometimes misleadingly.
Note: the term professional within the context of this policy relates to all health, allied, social care professionals.
2.1.1 Advance statements
Section 4(6) (a) of the MCA places special emphasis on written statements the person may have made before losing capacity, which could provide relevant information when best interests decision have to be made on their behalf.
An advance statement is an expression of a person`s wishes, feelings, beliefs and values about how they would prefer to be cared for and treated if they lose capacity to make decisions for themselves. Such expressions of wishes and preferences must be taken into account when considering an incapacitated patient’s best interests but are not legally binding.
An advance statement can reflect their religious beliefs or other beliefs that they have and allows the patient to state how they would like to be treated should they not be able to communicate their wishes in the future.
Advance statements can be used to nominate a person to be consulted (if practicable and appropriate) with at a time a decision has to be made, although at present their view is not legally binding. However, if the nominated person has also been granted lasting power of attorney to make personal welfare decisions, the decision of the person with lasting power of attorney will be binding.
Advance statements can also be used to inform health professionals of how the person would prefer to be treated medically.
2.1.2 Advance decisions to refuse treatment (ADRT)
An ADRT is a refusal to accept certain medical treatments in the future if specified circumstances arise once the person has lost capacity.
ADRTs are sometimes also known as ‘advance directive’, ‘advance refusal’ or ‘living will’. However, the statutory term is “advance decision” and to make it clear to staff the term advance decision to refuse treatment (ADRT) will therefore be used in the remainder of this policy. A valid ADRT which is applicable to the circumstances which arise is legally binding in the same way as a contemporaneous refusal by a person with capacity. Professionals may be legally liable if they treat a patient in the face of a valid and applicable ADRT.
An ADRT does not give an individual the right to demand specific treatment at the time of making it or in advance.
Advance statements and ADRTs cannot be used when the person has the capacity to consent to, or refuse, the proposed treatment
3 Scope
Rotherham Doncaster and South Humber NHS Foundation Trust (the trust), supports the use of Advance statements and ADRT to enhance communication between patients, carers and staff. This policy applies to all patients who have made an advance statement or ADRT. All staff have the responsibility to make themselves aware of the presence of an advance statement or ADRT when a patient attends for care, and to consider the statement as stated within this policy below.
This policy applies to everyone in a paid, professional or voluntary capacity who is involved in the care, treatment or support of patients over the age of 16 under the umbrella of Rotherham Doncaster and South Humber NHS Foundation Trust (the trust). This includes staff employed by the trust, social care and health staff who are either seconded to the trust or work in partnership with the trust.
4 Responsibilities, accountabilities and duties
4.1 Chief executive
The chief executive is responsible for there being a structured approach to policy development and management.
Responsibility for this policy is delegated to:
4.2 Care group directors
The care group directors for each locality are the directors accountable for this policy.
4.3 Clinical managers
- Make a copy of this policy available to staff and to check staff have read it and are in a position to incorporate this policy into their practice.
- Make sure staff receive sufficient training and support to undertake their role.
4.4 Clinical staff
It is each individual’s responsibility to ensure they make themselves aware of this policy and receive sufficient training and information about advance statements and ADRT to undertake their role.
5 Procedure and implementation
5.1 Advance statement
A person aged 16 and over may make a general advance statement reflecting their wishes and feelings, about how they would like to be treated in the future if they lose capacity. For some patients it is aimed towards planning for a crisis, relapse, acute episode when the individual is unable to make their preferences unknown. It can also be used as part of end of life care planning.
An advance statement does not bind doctors and professional staff to a particular course of action if it conflicts with their professional judgement or if the treatment preferences described are not considered appropriate or necessary (for example, taking into account available resources). Patients should be made aware of this.
However whilst an Advance Statement does not have any basis in law, if a patient or their family has made staff aware that they have a written advance statement, staff must be able to demonstrate that the patient’s wishes and feelings have been taken into account as part of considering what is in their best interests if they lose capacity. If a patient`s wishes are not followed clear reasons for this must be documented in the patient’s records as part of the best interest`s process.
It is important to consider an advance statement when planning care and treatment and at each review
5.1.1 Examples of what may be included in an advance statement
An appointment of representative: a person may name another person to be consulted about health care decisions when he or she is or are incapable of deciding for him or herself. That named person should then be consulted as part of consideration of what is in the patient`s best interest once they lose capacity. However, the views of the named person will not be legally binding unless that person has been formally given lasting power of attorney to make personal welfare decisions on a patient’s behalf or is a court appointed deputy under the provisions of the MCA 2005.
A statement about wishes in relation to a particular treatment: the patient would like to receive should they become unwell. Although not legally binding on doctors and other staff, this should be taken into account when deciding treatment.
A statement in relation to how and where they should be cared for: at a time when their condition may deteriorate, and they are no longer able to care for themselves.
A statement of general beliefs: on various aspects of life, which an individual values. This statement contains no specific request or refusal but attempts to paint a picture of the individual as an aid to healthcare professionals in deciding what the patient would want.
5.1.2 What to consider when making an advance statement
- The patient must have capacity at the time it is written. If there any doubts about the persons capacity to consider an advance statement, then an assessment of capacity should be undertaken and recorded on MCA1.
- The advance statement should preferably be in writing, although a patient`s verbally expressed wishes should also be taken into account when considering what is in their best interests.
- There is no set format for an advance statement. The patient may wish to use the trust’s template (see appendix A) or it could be written in another form such as the wellness recovery action plan (WRAP). This has been adopted by many patients and carers across RDaSH as the preferred model to support self-management and recovery, which includes a section on crisis planning which is to all intents and purposes the same as an advance statement.
- Assistance in writing an advance statement should always be offered to those individuals who have sensory impairment or who lack confidence in completing written forms. The provision of an interpreter should also be provided as required.
- If the patient has the capacity but is unable to write staff should facilitate the recording of a patient’s advance statement in writing.
- The content of an advance statement should be the patients’ own views and wishes and should not be unduly influenced by any other person.
- The advance statement must be clear in meaning. If the statement is unclear or ambiguous it must be discussed and clarified with the patient while they still have capacity.
- An advance statement can be made in conjunction with the care coordination process under care programme approach, and a copy should be kept within the care record. It is important to ensure that all patients are given information about advance statements during their assessment and, or CPA review.
- Patients can withdraw or alter their advance statement at any time while they have capacity to do so. It is the patient’s responsibility to notify the trust of any changes made to their advance statements.
If a patient wishes to refuse a particular treatment in the future the process of making an advance decision to refuse treatment (ADRT) should be explained to them.
Any advance statement needs to be signed by the patient and witnessed by an appropriate person to validate the signature.
5.1.3 Where to store an advance statement
A copy of the advance statement should be scanned and stored on the patient record and an appropriate entry made on the MCA advance statements and advance decisions to refuse treatment questionnaire. This will alert staff of its existence.
5.1.4 Sharing an advance statement
With the agreement of the individual, a copy of the advance statement should be circulated to all members of the care team. Staff should ensure that the patient wishes are considered in situations where they are relevant in the future.
5.1.5 Reviewing an advance statement
An advance statement should be reviewed with the patients every 6 months through the process of care coordination review. If the review results in changes to the advance statement, the updated document should be circulated as above, and copies of the original document made inactive.
5.2. Advance decision to refuse treatment (ADRT)
5.2.1 Who can make an ADRT
An ADRT can only be made by an individual aged 18 and over with capacity to make advance care and treatment decisions. In the event of them losing capacity in the future, a properly made ADRT is as valid as a contemporaneous decision (for example, one that is made at the time).
Patients can only make an advance decision to refuse treatment. Nobody has the legal right to demand specific treatment, either at the time or in advance.
5.2.2 What is an ADRT?
An ADRT is preferably a written document where the content has been agreed through discussion and negotiation between the person making it and the people involved in their care and treatment, including where appropriate, family members and carers. A verbal ADRT can be made, unless it is about refusal of life sustaining treatment, in which case specific criteria need to be met.
A written ADRT is a document owned by the patient and shared with the trust. It is not the property of the trust or a document that requires staff to ensure is completed.
5.3 Valid and applicable
Before healthcare professionals can apply an ADRT, there must be proof that:
- it exists
- is valid
- is applicable in the current circumstances
A valid ADRT refusing treatment, applicable to the arising circumstances, is legally binding and therefore must be followed. The ADRT may be written in medical language or in lay terms but must be clear and unambiguous in order to be legally enforceable. The health professional treating the patient must be assured of the following to ensure that the ADRT is valid and applicable.
5.3.1 When is an ADRT valid and applicable?
In order for the ADRT to be valid and applicable the following conditions must apply:
- the person had capacity to make the decision at the time the decision was made. For most people there will be no doubt about their capacity to make an ADRT. In line with principle 1 of the act, ‘that a person must be assumed to have capacity unless it is established that he or she lacks capacity’. Professionals should always start on the assumption that the patient had capacity at the time they made it unless there was reasonable grounds to doubt the person had capacity at the time they made it. However although it is not a requirement of the act, in some particular cases if the decision is about life-sustaining treatment or may be challenged in the future it may be useful to get evidence of a person`s capacity at the time they make the decision
- professionals must be satisfied that the ADRT was made whilst the person had capacity and was not affected by (for example) illness or medication. To make a valid ADRT the person must be judged to be ‘competent’ or to ‘have necessary mental capacity to make the decision at the time it was made
- the person is free from the undue influence of others. Professionals must be satisfied that the ADRT was not based on false information or pressure from other people
- the person is sufficiently informed. Professionals must assure themselves that the person understood the implications of the decision they made at the time and also that the person has acted in a way consistent with the ADRT
- the person intends the refusal to apply to the circumstances that subsequently arise. The person must have envisaged the type of situation the decision applies to. To be applicable, an advance decision must apply to the situation in question and in the current circumstances. For example, a new anti-psychotic medication becoming available after an ADRT is made. If it is not specified, the ADRT could be taken to mean that a refusal of medication might not apply to newly available medication
5.3.2 When an ADRT is NOT valid
- The patient has withdrawn the ADRT, at a time when he or she has capacity to do so (note, withdrawal of an ADRT does not have to be in writing).
- The patient after making the ADRT has made a lasting power of attorney (LPA) for health and welfare, giving the attorney authority to make treatment decisions that are the same as those covered by the ADRT.
- The patient has done something that clearly goes against the ADRT which suggests they have changed their mind.
- An advanced decision refusing life sustaining treatment will not be valid unless the ADRT is in writing, signed by the patient in the presence of a witness and includes a clear, specific statement by the patient to the effect that the decision is to apply to the specific life sustaining treatment even if his or her life is at risk.
- An ADRT refusing ‘basic care’ (see definition appendix A) is also invalid. An ADRT may not refuse, for example, warmth, shelter and hygiene measures to maintain body cleanliness. This includes the offer of oral food and hydration, but not artificial nutrition and hydration. Such care may be provided in the best interests of a person lacking capacity to consent to it.
5.3.3 When an ADRT will NOT be applicable
- The proposed treatment is not the treatment specified in the ADRT
- The patient has the capacity to accept or refuse the treatment at the relevant time
- There are reasonable grounds for believing that circumstances now exist which the patient did not anticipate at the time of writing the ADRT, which would have affected the decision, such as advances in treatment or changes in patient’s religious beliefs. So, when deciding whether an ADRT applies to the proposed treatment, professionals must consider:
- how long ago the ADRT was made
- whether there have been changes in the patients’ personal life that might affect the validity of the ADRT (for example the person is pregnant, and this was not anticipated when they made the ADRT)
- whether there have been developments in the medical treatment that the person did not for see (for example new medication, treatment or therapies)
5.4 Patients detained under the Mental Health Act (MHA) 1983
The MHA 1983 takes precedence and prevails over an ADRT when it comes to treatment for mental disorder. This means that where a patient is subject to compulsory detention and treatment under part IV of the MHA 1983 an ADRT is not legally binding on decisions relating to the patient’s mental disorder. However, the responsible clinician should take an ADRT into consideration when deciding upon a treatment plan and where it is decided to go against the patients preferred wishes the reason is to be recorded in the patient’s clinical records.
Decisions made by detained patients will still be legally binding insofar as they relate to treatment which is not connected with their mental disorder. For example, a decision refusing treatment for a patient’s physical health, which is not covered by the MHA 1983, must be adhered to if, it is valid and applicable to the circumstances.
Treatment for a patient’s mental disorder under the MHA 1983 can include treating the symptoms or consequences of the mental disorder, as well as the treatments which are a necessary pre-requisite to treatment for the patient`s mental disorder. For example, feeding a detained patient with anorexia nervosa by nasogastric tube would be likely to come under compulsory treatment under the MHA 1983 because the treatment (feeding) is aimed at treating a symptom of the mental disorder.
5.4.1 Electroconvulsive therapy (ECT)
If a patient lacking capacity has made a valid and applicable ADRT to refuse ECT or an attorney under a lasting power of attorney, or a court appointed deputy, or a court has refused ECT on the patient`s behalf, then the ECT should not be given, even if detained under the MHA, unless treatment is needed in an emergency, when it can be given under section 62 of the MHA if certain circumstances apply.
Although the MHA allows ECT to be given in an emergency to a person who has made an advance decision to refuse it, this would only happen in exceptional cases.
5.5 Making an advance decision to refuse treatment (ADRT)
5.5.1 What is an ADRT?
An advance decision to refuse treatment (ADRT) is a statement of your wishes to refuse a certain treatment in a specific situation. It is a way of making sure everyone knows what treatments you do not want to have, if you lose capacity to make your own decisions
5.5.2 Who can make an ADRT
It is up to individuals with mental capacity to decide whether they want to refuse treatment in advance. If they are over 18 they are entitled to do so if they wish, but there is no obligation to do so.
5.5.3 When can and ADRT be made?
It is important that the ADRT is completed when an individual feels best able to represent their wishes clearly and to record them or have them recorded formally.
Patients must have capacity to make an ADRT. The Mental Capacity Act 2005 (MCA) presumes capacity, however if there is any doubt about their capacity at the time of making the ADRT an assessment should be undertaken and recorded on MCA1 on the patient’s electronic record. This will ensure there are no doubts over their capacity at the time, if concerns are raised later.
5.5.4 How should an ADRT be recorded
There is no nationally agreed or set format for an ADRT the patient may use whatever format for an ADRT they wish, including a verbal statement. Some patients may prefer not to make what they consider to be a legalistic document but instead talk to professionals about their wishes to refuse treatment and have these recorded in their medical notes or CPA documentation. In such cases, patients should be encouraged to check the notes made about them to ensure that they agree with what is written and sign and date them.
Alternatively, patients can use the trust pro-forma (appendix B) if they wish. Staff can help patients who need assistance to record their wishes on the pro forma. Once completed the patient should be asked to check the content to ensure they agree with what is written.
5.5.5 Who should be consulted?
It is useful for the patient to consult with carers and other health professionals when making an ADRT to ensure that their decisions are based on realistic views.
Decisions may evolve in stages over time and with discussion. It is not advisable to make complicated decisions at one time without further review.
Written ADRTs should use clear and unambiguous language. Therefore, professionals consulted must consider the following if asked for assistance with an ADRT:
- does the patient have sufficient knowledge of the condition?
- does the patient have sufficient knowledge of possible treatment options if there is a known illness?
- is it clear that the patient is reflecting their own view and is not being pressured by other people?
- professionals need to ensure that patients are aware of the risks of ADRT as well as the benefits
- professionals need to be aware that any doubt or ambiguity about intention or capacity at the time of drafting the decision could lead to it becoming invalid
Information should be provided in an accessible format to assist in making informed choices.
ADRT should be understood as an aid to, rather than a substitute for, open dialogue between patients and health professionals. An open attitude and a willingness to discuss the advantages and disadvantages of certain options can do much to establish trust and mutual understanding. Professionals must document in the clinical records all involvement and discussions about ADRT.
5.5.6 Duress and undue influence
Professionals consulted at the drafting stage must take reasonable steps to ensure that patient’s decisions are not made under duress. If professionals, when consulted, suspect there may be duress or undue influence from others, they must take steps to bring this to the attention of the appropriate manager.
5.5.7 What should be included in an ADRT
In drawing up an ADRT it is recommended that where the trust pro-forma is not used the written document contains the following information:
- patients full name
- address
- name and address of general practitioner or consultant
- whether advice was sought from health professionals
- a statement that the ADRT is intended to have effect if the maker lacks capacity to make treatment decisions
- a clear statement of the decision, specifying the treatment to be refused and the circumstances in which the decision will apply, or which will trigger a particular course of action
- signature of the person the ADRT refers to
- date drafted and date reviewed
- witness signature, date and relationship with individual
The advance decision must:
- set out clearly the treatment which is not to be carried out or continued
- set out any circumstances which are applicable to the decision
5.5.8 Witnessing an ADRT
The individual and a witness should sign and date a written ADRT, (although signing and witnessing the ADRT is not necessary to make the refusal legally binding unless it is intended to apply to life sustaining treatment (see point 5.6 on life sustaining treatment below).
In some situations, a professional such as a doctor may be asked to act as witness, however, an ADRT does not have to be signed by a doctor to make it valid.
The witness should only witness the patient’s signature and confirm that it appears that the maker intends the signature to give effect to the ADRT. The role of the witness does not involve certifying the capacity of the person making the ADRT.
5.5.9 What to do when told a verbal ADRT
Where an ADRT is received by a professional in the form of an oral statement, this be should recorded on the trust pro-forma and the patient should be asked to sign this document in the presence of a witness (the witness should not be the staff member who records the ADRT).
5.5.10 Where to record and store a written ADRT
A copy of the completed ADRT pro forma should be scanned and recorded on the MCA advance statements and advance decisions to refuse treatment questionnaire. This will alert staff of its existence.
With the agreement of the individual, a copy of the completed ADRT should be circulated to all members of the care team. Staff should ensure that the patient wishes are considered in situations where they are relevant in the future.
It is worth noting that some forms of treatment contained in ADRT should also be reflected in CPA documentation such as the CPA crisis plan. Care must be taken to ensure these are not contradictory
5.5.11 Storage of an ADRT made independently
When a patient is admitted to an inpatient setting they should be asked if they have an ADRT. If they have made an ADRT a copy of the ADRT should be obtained, scanned and recorded on the ADRT questionnaire on the patient’s electronic record.
If a patient who is receiving treatment in the community makes an ADRT then they should arrange for their care co-ordinator to receive a copy. This should ensure that the existence of the ADRT is brought to the attention of trust staff. The care co-ordinator should arrange for a copy of the ADRT to be recorded on the electronic patient record on the ADRT questionnaire.
5.6 Life sustaining treatment
5.6.1 What is considered to be life-sustaining treatment?
Life-sustaining treatment is defined as treatment which a person providing health care regards as necessary to sustain life. Whether a treatment is ‘life sustaining’ depends not only on the type of treatment, but also on the particular circumstances in which it may be prescribed. For example, in some situations giving antibiotics may be life sustaining, whereas in other circumstances antibiotics are used to treat non-life-threatening conditions. The important factor here is that the treatment is necessary to sustain life at that time. It is for the doctor to assess whether a treatment is life-sustaining in each particular situation.
Artificial nutrition and hydration (ANH) has been recognised as a form of medical treatment. ANH involves using tubes to provide nutrition and fluids to someone who cannot take them by mouth. It bypasses the natural mechanisms that control hunger and thirst and requires clinical monitoring. An advance decision can refuse ANH. Refusing ANH in an advance decision is likely to result in the person’s death, if the advance decision is followed.
If the ADRT includes an advance refusal of life- sustaining treatment, a requirement within the MCA 2005 is that it must be in writing and should state that the ADRT is to apply ‘even if life is at risk’. It must be signed and dated by the patient (or by another, on behalf of the patient and in the patient’s presence) and when the ADRT is signed it must be witnessed and then countersigned and dated by the witness.
5.7 Responding to an existing ADRT
Professionals will be protected from liability for failing to provide treatment if they ‘reasonably believe’ that a valid and applicable ADRT exists.
Therefore, staff should try to ascertain if a new patient has an ADRT as soon as possible. Where the existence of an ADRT is or becomes known then the following steps must be taken:
- consider any evidence that at the time of making the ADRT the person lacked capacity, and immediately advise the patient’s GP or consultant of concerns and of the available evidence
- ensure all staff, in particular medical staff, are made aware of the ADRTs existence and that an appropriate note is made and retained in a prominent position in the patient’s clinical file
- check the validity of the ADRT with the patient or where this is not possible consult the individuals identified in the statement, for example, named persons, witnesses. However, a statement or ADRT is not invalid just because it has not been possible to check with the individuals identified
- declare any conscientious objections to carrying out the instructions of the ADRT and arrange for an alternative worker as necessary
5.8 Emergency treatment
Emergency treatment must not be delayed in order to look for the ADRT, if there is no clear indication that one exists. If doubt arises as to the existence of an ADRT the matter may be referred to the courts for a decision. Professionals may be legally liable if they disregard the terms of an ADRT, or if it is known that the ADRT exists and is valid and applicable to the proposed treatment. However, under the MCA, if there are any significant doubts about the validity of an ADRT then the professional will be obliged to treat the person under best interests until clarification is obtained. This would need to be clearly recorded.
5.9 Withdrawal of ADRT
An ADRT may be withdrawn by the patient at any time providing they have capacity to do so. The withdrawal of an ADRT does not need to be in writing, including in the case of advance refusals of life sustaining treatment, for example, a verbal withdrawal will be sufficient, but should be recorded in the patients case notes where the ADRT was originally recorded. The person who has made the ADRT should tell anyone who knew about the ADRT that it has
been cancelled.
5.10 Reviewing and updating ADRT
Patients can make changes to an ADRT verbally or in writing. Patients who make an ADRT should be advised to regularly review their decisions. Any changes should be recorded in the patients’ health care notes or a copy of the updated ADRT obtained. ADRT made a long time ago before the proposed treatments are not automatically invalid. However, if a long period of time has elapsed since the ADRT was made, this may raise doubts about the extent to which it remains valid and applicable.
5.11 Invalid or inapplicable ADRT
If an ADRT is not valid or applicable to the current circumstances, professionals must nevertheless consider the ADRT as part of their assessment of the patient’s best interests if they are unable to make the decision themselves.
5.12 ADRT: Doubt or disagreement
In the event that there is doubt or disagreement about the validity or applicability of and ADRT all staff have a responsibility to discuss with their professional lead (for example, nurse consultant, clinical director, and Mental Capacity Act lead) who will if appropriate refer to the relevant medical director or care group director. However, if the matter remains unclear, legal advice should be sought with a possible view to seeking clarification as to the validity or applicability of the ADRT from the court of protection.
6 Training implications
6.1 Selection
As a trust policy, all staff must be aware that advance statements and advance decisions to refuse treatment form part of the Mental Capacity Act training which is mandatory for all clinical new starters to the trust. Following this all qualified clinical staff are require to undertake specific enhanced MCA training as identified by their manager.
The training needs analysis (TNA) for this policy can be found in the training needs analysis document which is part of the trust’s mandatory risk management training policy located under policy section of the trust website.
7 Monitoring arrangements
7.1 Training
- How: Training records.
- Who by: Mental health and MCA training coordinator.
- Frequency: Annual as part of report on MCA training.
- Reported to: Mental health legislation committee
7.2 Policy implementation
- How: Clinical audit.
- Who by: Mental Capacity Act lead.
- Frequency: Annual as part of audit of MCA policy.
- Reported to: Mental health legislation committee
8 Equality impact assessment screening
To download the equality impact assessment for this policy, please follow this link: Equality impact assessment.
8.1 Privacy, dignity and respect
The NHS Constitution states that all patients should feel that their privacy and dignity are respected while they are in hospital. High Quality Care for All (2008), Lord Darzi’s review of the NHS, identifies the need to organise care around the individual, ‘not just clinically but in terms of dignity and respect’. Consequently, the trust is required to articulate its intent to deliver care with privacy and dignity that treats all service users with respect. Therefore, all procedural documents will be considered, if relevant, to reflect the requirement to treat everyone with privacy, dignity, and respect, (when appropriate this should also include how same sex accommodation is provided).
8.1.1 Indicate how this will be met
No issues have been identified in relation to privacy, dignity, and respect.
8.2 Mental capacity act
Central to any aspect of care delivered to adults and young people aged 16 years or over will be the consideration of the individual’s capacity to participate in the decision-making process. Consequently, no intervention should be carried out without either the individual’s informed consent, or the powers included in a legal framework, or by order of the court.
Therefore, the trust is required to make sure that all colleagues working with individuals who use our service are familiar with the provisions within the Mental Capacity Act (2005). For this reason, all procedural documents will be considered, if relevant to reflect the provisions of the Mental Capacity Act (2005)to ensure that the rights of individual are protected, and they are supported to make their own decisions where possible and that any decisions made on their behalf when they lack capacity are made in their best interests and least restrictive of their rights and freedoms.
8.2.1 Indicate how this will be achieved
All individuals involved in the implementation of this policy should do so in accordance with the guiding principles of the Mental Capacity Act 2005. (Section 1)
9 Associated documents
- Consent to care and treatment policy
- Electro-convulsive therapy (ECT) clinical guidelines policy
- Care programme approach (CPA) policy
- MCA Mental Capacity Act 2005 policy
- Mental Health Act policies
10 References
- Mental Capacity Act 2005
- Mental Capacity Act Code of Practice
- Mental Health Act 1983 (as amended by the Mental Health Act 2007)
- The Children’s Act 1989
- Human Rights Act 1998
- Care Standards Act 2000
- Data Protection Act 1998
- National Health Service and Community Care Act 1990
- NICE quality standards: Decision making and mental capacity 2020
11 Appendices
11.1 Appendix A Basic and essential care
Basic and essential care means those procedures which are solely or primarily designed to keep an individual comfortable. This includes warmth, shelter, pain relief, management of distressing symptoms (such as breathlessness and vomiting) and hygienic measures such as management of incontinence. The administration of medication or the performance of any procedure which is solely or primarily designed to provide comfort to the patient or alleviate that patient’s pain, symptoms or distress are facets of basic care.
In the face of a valid ADRT refusing all physical care interventions only those measures essential for a patient’s comfort should be given. Therefore, appropriate food or drink should be made available for (but not forced upon) all patients. Artificial nutrition and hydration should not be given to a patient who has made a valid and applicable advance refusal of this treatment.
If the physical condition of the patient is starting to deteriorate, then legal advice should be sought as a matter of urgency. Authorisation to obtain legal services should be obtained through the medical director. If there is doubt about the validity of an apparent refusal, life-sustaining treatment and treatment to prevent a serious deterioration in the patient’s health can be provided while a decision is being sought from the court.
11.2 Appendix B Advance statement pro-forma
11.3 Appendix C Advance decision to refuse treatment pro-forma
11.4 Appendix D Flow chart
11.4.1 Advance decision to refuse treatment decision making flowchart
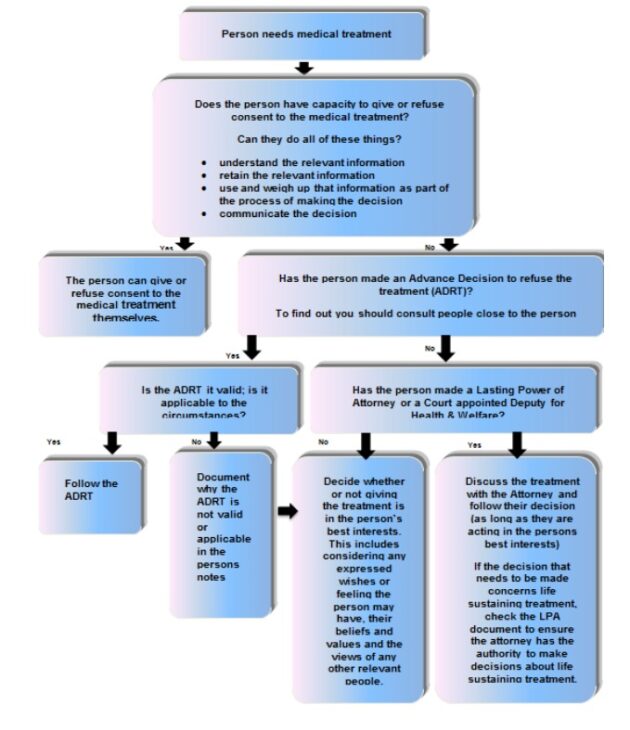
- Person needs medical treatment.
- Does the person have capacity to give or refuse consent to the medical treatment? can they do all these things?
- understand the relevant information
- retain the relevant information
- use and weigh up that information as part of the process of making the decision
- communicate the decision
- If yes, the person can give or refuse consent to the medical treatment themselves.
- If no, has the person made an advance decision of refuse the treatment (ADRT)? to find out you should consult people close to the person:
- if yes, is the ADRT it valid, is it applicable to the circumstances?
- if yes, follow the ADRT
- if no, document why the ADRT is not valid or applicable in the person’s note
- if no, has the person made a lasting power of attorney or a court appointed deputy for health and welfare:
- if no, decide whether or not giving the treatment is in the person’s best interests. This includes considering any expressed wishes or feeling the person may have, their beliefs and values and the views of any other relevant people
- if yes, discuss the treatment with the attorney and follow their decision (as long as they are acting in the person’s best interests). If the decision that needs to be made concerns life sustaining treatment, check the LPA document to ensure the attorney has the authority to make decisions about life sustaining treatment
- if yes, is the ADRT it valid, is it applicable to the circumstances?
Document control
- Version: 5.
- Ratified by: Mental health legislation operational group.
- Date ratified: 14 January 2021.
- Name of originator or author: Mental Capacity Act lead.
- Name of responsible individual: Mental health legislation operational group.
- Date Issued: 29 January 2021.
- Review date: January 2024.
- Target audience: All clinical staff.
Page last reviewed: March 20, 2024
Next review due: March 20, 2025