Contents
1 Aim
This standard operating procedure (SOP) is to ensure that all medical staff and clinicians within the children, adolescent mental health service (CAMHS) have a full understanding of the expectations placed on them whilst a child or young person is placed in a tier 4 establishment. This includes face to face visits, communication with the Tier 4 unit and communication with the patient and carer’s family.
2 Scope
The SOP is for use by all CAMHS clinicians and medical staff within the children’s care group
3 Link to overarching policy
This SOP should be read in conjunction with the following trust policy:
4 Procedure
Any child and young person that has been admitted to a tier 4 unit via a planned or unplanned route needs to have the stability and security of knowing the frequency of visits from their care coordinator or lead worker and their consultant psychiatrist.
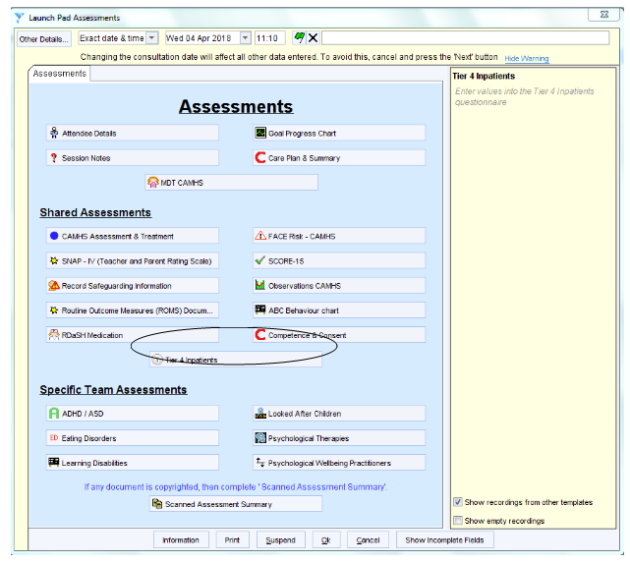
Once a child has been admitted it is the responsibility of the care coordinator or lead worker to alert their manager to the admission. The care coordinator needs to complete the details of the admission on SystmOne (appendix A), complete the commissioner tier 4 document (appendix B) and the root cause analysis (appendix C), so this can be passed on to the local commissioners.
Once an admission has occurred the relevant pathway lead, upon being informed of the admission, will allocate another worker to co-work the case to ensure that the tier 4 units always have access to a CAMHS clinician. It is the responsibility of both clinicians to ascertain who will attend and liaise with the tier 4 unit.
At the child and young person’s admission, first care programme approach (CPA) review, the care coordinator or co-worker will attend the meeting to ensure collaboration with the Tier 4 unit on the patient’s care plan, risk assessment, crisis plan, contingency plan and discharge planning. If both workers are unable to attend this meeting, then either the consultant psychiatrist or a representative from CAMHS will attend (this meeting may be set up for face to face or over virtual media).
It is expected that either the care coordinator or co-worker will actively engage in each CPA review, or where there are significant changes in the patient’s presentation, they would be expected to attend to review the situation. If the care coordinator is unable to attend in person, then consideration needs to be made for alternative forms of communication such as Skype and conference calls. The care coordinator or co-worker when visiting the patient should also view the patient’s electronic care records to ensure that both the tier 4 care plan and the local CAMHS care plan are working in collaboration; and update the local record accordingly.
The patients’ leave needs to be managed by the tier 4 unit and local CAMHS service, where a local CAMHS service has not been made aware of home leave; this would need to be reported directly to their manager and the NHS England case worker so they can take appropriate action.
The consultant psychiatrist will need to liaise with the consultant at the Tier 4 unit around the patient’s treatment and medication plan, to ensure on discharge they are both in agreement with the plan. The consultant where possible should at least try and attend as many CPA reviews (which may be face to face or virtual meetings)
There is also an expectation that the consultant will attend the discharge planning meeting, to ensure that the community team can manage the patient. If in unexpected circumstances the consultant cannot attend, then a telephone conference call should be expedited.
Outside of these meetings, the care coordinator or co-worker should make fortnightly contact with the tier 4 unit by telephone to ascertain the patient’s progress or deterioration and adapt the local care plan or crisis plan to replicate work that is being done at the unit. Requests should be made to the unit for weekly progress reports to be sent to both CAMHS clinicians and the local CAMHS consultant psychiatrists for updates.
If the local CAMHS consultant psychiatrist disagrees with specific treatments then a conversation needs to occur, consultant to consultant. This may result in a visit to the unit by the local CAMHS consultant psychiatrist to gather further information. If the care coordinator or co-worker has any concerns surrounding certain treatments this information will need to be passed to the local CAMHS consultant psychiatrist for advice.
During the patient’s admission the care coordinator or co-worker needs to have regular contact with the patient or carers family to make sure they are updated with their child’s care, and if any concerns are raised these are reported to the team manager. The family should be made aware of any changes to local care planning; this may include transferring patients closer to their local community. Any changes to the family’s position may need to be included in the patient’s care plan, for example where a family cannot have the patient back home. Any discharge plans and future care plans for those people detained under section 3 of the Mental Health Act should consider the requirements of Section 117 the aftercare needs of the patient and liaise with local authorities to support. (Refer to the trust’s section 117 policy for further information).
4.1 Long term placements, extending beyond 6 months
Where a child and young person is likely to be placed in a tier 4 or specialist placement, for a period extending beyond 6 months, then liaison with the unit and frequency of contacts do not need to be as often as stated above. However, there is an expectation that telephone contact should occur monthly to the unit and the young person (as appropriate).
The frequency and level of contact needs to be documented in the child and young person’s care plan, ensuring all relevant parties are in agreement with these contact arrangements. It is still expected that active representation by the care coordinator is provided to each CPA review or occurs though delegation of who attends may be flexible, especially in smaller specialist teams such as learning disability. Where face to face representation cannot occur then other forms of communication need to be explored such as Skype or conference calls.
4.2 Section 85 Children Act 1989
Where a child and young person has been placed in a tier 4 unit for more than 3 months the local children services need to be made aware to undertake section 85 duties. It is the responsibility of the care coordinator to ensure that the relevant local authority is aware of the admission (see appendix D).
4.3 Care, education and treatment review (CETR) process
For children and young people with a diagnosis of learning disability or autism, a care, education and treatment review (CETR) must be completed prior to any admission. The relevant local commissioners need to ensure that they invite all appropriate agencies and distribute all related information. It is the responsibility of the local commissioners to ensure CETR are arranged and managed accordingly.
For children that have been through the CETR process, the CETR is reviewed upon a tier 4 admission, this is the responsibility of the NHS England case manager and in-patient unit.
4.4 Conflict resolution of tier 4 issues
As already highlighted, should any issues arise, the relevant documentation must be completed. However, these issues need to be managed locally where possible.
All initial problems should be passed to the team manager to liaise with the appropriate tier 4 unit and the NHS England case worker if appropriate. If at this point it cannot be resolved, then the manager will pass the information on to the service manager of CAMHS. If problems still persist and a resolution has not been sought, then this will continue up to the children’s care group director or associate nurse director.
4.4.1 Conflict resolution process
- Care coordinator.
- Team manager.
- Service manager.
- Children care group director or care group nurse director.
5 Appendices
5.1 Appendix A SystmOne tier 4 form
CAMHS launchpad assessment window.
5.2 Appendix B Information for commissioners
5.3 Appendix c Root cause analysis
5.4 Appendix D Section 85 and 86 Children Act 1989 notifications to children’s social care
Sections 85 and 86 of the Children Act 1989 were introduced to ensure that children who are accommodated by a health agency, local education authority, care home or independent hospital for a consecutive period of at least three months are brought to the attention of children’s social care. Such children are potentially vulnerable by virtue of their being accommodated outside of the family.
Upon notification that a child from their area is living in such arrangements, Children’s social care can assess whether the child’s welfare is being adequately safeguarded and promoted and whether any additional services or interventions should be offered to the child and their family.
As sections 85 and 86 only apply to those children who are accommodated for a consecutive period of at least three months, the provisions do not apply to children placed on a term-to-term basis in boarding school where they return home during the school holidays.
It is a requirement of the accommodating authority to notify children’s social care for a child who would normally be resident within that local authority area if they are providing accommodation for a consecutive period of at least three months or if they have the intention of providing accommodation for such a period.
5.4.1 Legal requirements
5.4.1.1 Section 85 Children Act 1989
- Where a child is provided with accommodation by any Local Health Board, Special Health Authority, Primary Care Trust, National Health Service Trust, NHS Foundation Trust or local education authority (“the accommodating authority”):
- for a consecutive period of at least three months
- with the intention, on the part of that authority, of accommodating him for such a period, the accommodating authority shall notify the responsible authority.
- Where subsection (1) applies with respect to a child, the accommodating authority shall also notify the responsible authority when they cease to accommodate the child.
- In this section “the responsible authority” means:
- the local authority appearing to the accommodating authority to be the authority within whose area the child was ordinarily resident immediately before being accommodated
- where it appears to the accommodating authority that a child was not ordinarily resident within the area of any local authority, to local authority within whose area the accommodation is situated.
- Where a local authority has been notified under this section, they shall:
- take such steps as are reasonably practicable to enable them to determine whether the child’s welfare is adequately safeguarded and promoted while he is accommodated by the accommodating authority
- consider the extent to which (if at all) they should exercise any of their functions under this Act with respect to the child.
5.4.1.2 Section 86 Children Act 1989
- Where a child is provided with accommodation in any care home or independent hospital:
-
- for a consecutive period of at least three months
- with the intention, on the part of the person taking the decision to accommodate him, of accommodating him for such period
the person carrying on the home shall notify the local authority within whose area the home is carried on.
-
- Where subsection (1) applies with respect to a child, the person carrying on the home shall also notify that authority when he ceases to accommodate the child in the home
- Where a local authority has been notified under this section, they shall:
- take such steps as are reasonably practicable to enable them to determine whether the child’s welfare is adequately safeguarded and promoted while he is accommodated in the home
- consider the extent to which (if at all) they should exercise any of their functions under this Act with respect to the child
- If the person carrying on any home fails, without reasonable excuse, to comply with this section he shall be guilty of an offence.
- A person authorised by a local authority may enter any care home or independent hospital within the authority’s area for the purpose of establishing whether the requirements of this section have been complied with.
- Any person who intentionally obstructs another in the exercise of the power of entry shall be guilty of an offence.
- Any person exercising the power of entry shall, if so required, produce some duly authenticated document showing his authority to do so.
- Any person committing an offence under this section shall be liable on summary conviction to a fine not exceeding level 3 on the standard scale.
Document control
- Version: 3.1.
- Unique reference number: 11.
- Date ratified: 20 February 2024.
- Ratified by: Clinical policies review and approval group.
- Name of originator: Pathway lead for the mental health cluster.
- Name of responsible individual: Children’s care group director.
- Date issued: 22 February 2024.
- Review date: December 2024.
- Target audience: All clinical staff in children and young people’s mental health service across the trust.
Page last reviewed: April 05, 2024
Next review due: April 05, 2025