Contents
1 Introduction
Disengagement can be defined as a patient who avoids contact with services, either intentionally or unintentionally over a period of time. The period of time will be determined by the risks that the patient poses and the clinical judgement of the care team.
Reasons for disengagement are varied and may include poor insight, deterioration or acuity of mental health difficulties, concerns about the person capacity to make decisions about their care and treatment, forgetfulness, transport difficulties, substance misuse and safeguarding concerns. For others it may simply be that they have reached a stage in their recovery where they no longer feel that they need to engage with services. However in some cases, disengagement with services will raise significant concerns relating to the health, safety and wellbeing of an individual or others. In a small number of cases failures to attend and disengaging with services raises serious concerns relating to safeguarding children. In order to promote safety and wellbeing of all children it is vital that failure to attend is considered and the impact that compliance or lack of engagement will have on an adult’s ability to provide good enough consistent care to a child.
The overriding principles of the Children Act 1989 and 2004 place a clear and absolute requirement for all organisations and their services to have a clear emphasis on ‘the importance of keeping the focus on the child and his or her safety and welfare, understanding the daily life experience of the child, seeing the child alone where appropriate and using information about the family’s history and functioning to inform decision making’.
This awareness of the child’s needs can help those services working with adults to recognise the potential impact of non-attendance or disengagement from services by adults and the impact this could have on the safety and wellbeing of a child or children whether they live with the child or children, or have contact with a child or children. The clinical decision tree is a key tool in this process and provides a tool where risk and impact can be considered.
In order to promote the health, safety and wellbeing of all patients and others, it is vital that disengagement from services is considered seriously and that responses from the service are proportionate to any measured or perceived risk.
The trust has a responsibility to ensure that it deliver safe and effective services and attempts to engage patients in treatment and care. It must also consider the complex mental health needs of its patient and the impact that disengagement from services may have on them and their families.
Patients referred to Adult Community Mental Health Services attend, in the main, on a voluntary basis. Exceptions to this are those that are subject to Mental Health Act 1983 (MHA) Community Treatment Orders, other sections of the Mental Health Act, those who need to be treated under the Mental Capacity Act 2005 (MCA) and treatment orders directed by the courts.
2 Purpose
The purpose of this policy is to set out the arrangements for, and approach to, the management of patients who are at risk of disengaging, or who have disengaged, with mental health services and those where there may be safeguarding children’s concerns.
3 Scope
This guidance applies to all clinical staff working within community mental health services and arrangements to safeguard children
4 Responsibilities, accountabilities and duties
4.1 Service managers and team managers
Service managers and team managers are responsible for:
- making their staff aware of the contents of this policy
- monitoring the compliance of their staff with the contents of this policy
- facilitating multidisciplinary team discussions to assist decision making and communication of assessments and plans
4.2 Care coordinators and lead professionals
- Following the appropriate steps in this policy and informing the team manager, or nominated deputy, where necessary.
4.3 All other clinical staff
It is the responsibility of every member of the care team to alert the care coordinator and lead professional if they are concerned that a patient is at risk of disengaging from services
5 Procedure and implementation
For the purpose of this policy the trust has separated patients who disengaged into two groups:
- patients referred to, but not yet assessed by services
- patients in receipt of services and subsequently disengage
- relates to those adults who are in receipt of services, subsequently disengage and have parental, caring responsibility and access to children
Each category is separated into high and low risk.
Staff should follow the guidance below that most appropriately describes their patient. Where there is uncertainty staff should discuss the case with their team manager and agree which pathway to follow.
For patients accessing home treatment and who are deemed to be high risk, please refer to appendix A.
When a patient disengages the steps below must be followed and all actions appropriately recorded in the electronic patient record (EPR).
5.1 Patients referred to, but not yet assessed by services
5.1.1 Urgent and emergency referral
If the patient misses an initial appointment following referral, then the allocated assessor must:
- attempt to contact the patient that day to identify reasons for non-attendance
- agree an alternative appointment if possible
- attempt to contact any identified family members and carers where appropriate
- consider undertaking a cold call. If there is no answer, a calling card must be left asking the patient to contact the service
- where there are concerns regarding a real and immediate risk to life, or of significant harm to others, the assessor must inform the police. Where possible this should be discussed with a team manager and senior clinician
- if, after 24 hours, no contact has been made, the assessor must notify the referrer and all other agencies involved with the patient including their general practitioner (GP). A joint plan of action must be agreed and recorded. Where appropriate, family members or carers may be involved and be informed of any plans
If the receiving service has been informed by the referrer that there are concerns regarding the impact on any child or children:
- discussions must be held with the team manager, line manager or the safeguarding supervisor and a member of the safeguarding children team to consider what action if any is required to safeguard any child or children as a result of the adult failing to engage with services
- the care coordinator, key worker, allocated worker, clinical staff must contact the referrer and inform them that the adult has failed to engage with the service. This should be confirmed in writing
5.1.2 Routine referral
If there are no known or suspected significant risks then the allocated assessor must:
- attempt to contact by the patient by telephone
- if contact by telephone is unsuccessful the assessor must write to the patient using first class mail requesting that they contact the service within 1 week
- if there is still no contact then the assessor must notify the referrer and all other agencies involved with the patient including their GP. A joint plan of action must be agreed and recorded. Where appropriate, family members or carers may be involved and be informed of any plans
- consider referral on to another service
5.2 Patients who are in receipt of services and those who have contact with children, parent and care for children and risks are identified
It must be made clear at the commencement of any intervention or offer of a service, that all staff have a responsibility to safeguarded children and this may include sharing information and beaching confidentiality with other agencies. This will include a professional’s assessment of the impact that failing to attend or engage may have on the ability of an adult to parent or provide care to a child or children.
Where it is suspected that a patient has disengaged and attempt to make contact by phone and in writing have failed, the team should:
- assertively attempt to make contact with the patient using all reasonable methods available to them that may include but not limited to:
- contacting the patient direct through a variety of electronic devices
- contacting family or knows associates
- contacting other providers involved in the patients care
- Unannounced home visits (if unsuccessful staff must leave a calling card asking the patient to make contact)
- if the team is able to reengage the patient then a full assessment of their needs and risk must be undertaken within 7 days
- if it is not possible to make contact then the case must be escalated for discussion with the team manager
- consideration should be given to contacting the police to request their support in establishing the safety of the patient
- consider support from home treatment or assertive outreach who may be able to offer a more flexible or intensive approach to engagement. A full transfer of care to assertive outreach should not be considered until the patient has reengaged
- determine whether the disengagement could affect the parenting capacity and therefore place any child or children at risk. The clinical member of staff must discuss the case with the team manager, line manager, safeguarding supervisor or the Safeguarding team as to what action should be taken
- inform the referrer by telephone and in writing if the service user does not respond to reengagement requests and the assessed impact disengagement may have on their ability to parent or provide care to children
- inform those services known to be engaged with the children as part of any ongoing intervention (for example, health visitors, school nurses, GP’s, and education) including the impact of the disengagement from the service
- act in accordance with RDaSH safeguarding children policy
- ll staff have a personal and professional responsibility to assess, determine and act if they believe a child’s welfare will be impacted by an adult’s unwillingness to engage with services
- act in accordance with RDaSH care programme approach (CPA) policy and procedure where applicable
- act in accordance with RDaSH safeguarding adults policy
- act in accordance with local safeguarding children board policies and procedures for the locality
5.3 Patients who are in receipt of services where there is no identified risk
There are some patients who will receive low levels of mental health support, for example, through nurse led clinics. If the patient does not attend two consecutive appointments, the lead professional must:
- attempt to contact the patient by phone, or another appropriate method, to identify the reasons for non-attendance and to offer a further appointment
- if contact is unsuccessful then the lead professional should attempt to contact significant family members or carers or associates in an attempt to gain information as to the patient’s current situation.
- if contact is successful and there is a suspected or confirmed deterioration in the patient’s mental health then the patient should be “stepped up” to the appropriate Community Treatment team
- if the patient is well and wishes to be discharged this should be managed in line with the discharge process detailed in the CPA and None CPA policy
- if contact continues to be unsuccessful then the lead professional should write to the patient, inviting them to contact the service if a further appointment is required. The option of an alternative venue and time most suited to the needs of the patient concerned should be offered. The letter should state that if no contact is made within three weeks, then the individual will be discharged from the service
5.4 Mental Health Act
Where appropriate consideration should be given to convening a Mental Health Act assessment.
For patients who are subject to community treatment orders or conditional discharge the responsible clinician must consider whether there are grounds to recall the patient to hospital.
5.5 Safeguarding
Any safeguarding concerns (adult or child) must be discussed with the team manager, named safeguarding nurse and addressed in line with local safeguarding policies.
5.6 Multi disciplinary team meeting (MDTM) and discharge
If the team are unable to make meaningful contact with the patient then they must arrange a multi disciplinary team meeting (MDTM) to discuss and plan future care.
The urgency of the MDTM will be determined by the information available to the practitioner at the time. The MDTM must include as a minimum a senior clinician and team manager, however may include a number of professionals across agencies.
The plan agreed by the MDTM must be shared with the GP, other relevant agencies and family or carers where appropriate.
Any decision to discharge should be informed by the MDTM and must be discussed and agreed with the team manager. The GP, other relevant agencies and family or carers where appropriate must also be informed of discharge.
Notification of discharge must be sent to the patient in writing and must include a crisis contingency plan, which, as a minimum supports the patient to access services should they experience any future deterioration in their mental health.
5.7 Patients who are known or assessed to be at risk of dis-engagement and reengagement with the service
It is known that some patients disengage and re-engage with services a number of times before reaching a stage where they are ready to complete the treatment pathway. In view of this any risk of disengagement should be discussed and planed for jointly with the patient before they enter into an episode of treatment.
With such patients a decision to discharge for failing to keep their appointment may not be deemed clinically appropriate, and therefore the MDTM should consider the appropriate course of action keeping the patients general practitioner informed of any changes in care.
6 Training implications
6.1 All clinical staff groups receive safeguarding training as part of the safeguarding
training offer
- How often should this be undertaken: The policy links to safeguarding children training requirements.
- Length of training: half day training.
- Delivery method: Face to face and e-learning.
- Training delivered by whom: Named nurses, safeguarding children.
- Where are the records of attendance held: Electronic staff record system (ESR).
As a trust procedure, all staff need to be aware of the key points that the procedure covers. Staff can be made aware through a variety of means such as:
- all user emails for urgent messages
- continuous professional development sessions
- daily email (sent Monday to Friday)
- group supervision
- intranet
- one to one meetings or supervision
- posters
- team meetings
- local induction
- special meetings
7 Monitoring arrangements
7.1 Compliance with the policy
- How: Through discussion on a case by case basis during supervision and at team meetings.
- Who by: Team managers.
- Reported to: Care group quality meeting.
- Frequency: Quarterly.
8 Equality impact assessment screening
8.1 Privacy, dignity and respect
The NHS Constitution states that all patients should feel that their privacy and dignity are respected while they are in hospital. High Quality Care for All (2008), Lord Darzi’s review of the NHS, identifies the need to organise care around the individual, ‘not just clinically but in terms of dignity and respect’. Consequently, the trust is required to articulate its intent to deliver care with privacy and dignity that treats all service users with respect. Therefore, all procedural documents will be considered, if relevant, to reflect the requirement to treat everyone with privacy, dignity, and respect, (when appropriate this should also include how same sex accommodation is provided).
8.1.1 Indicate how this will be met
No issues have been identified in relation to this policy.
8.2 Mental capacity act
Central to any aspect of care delivered to adults and young people aged 16 years or over will be the consideration of the individual’s capacity to participate in the decision-making process. Consequently, no intervention should be carried out without either the individual’s informed consent, or the powers included in a legal framework, or by order of the Court. Therefore, the trust is required to make sure that all colleagues working with individuals who use our service are familiar with the provisions within the Mental Capacity Act (2005). For this reason, all procedural documents will be considered, if relevant to reflect the provisions of the Mental Capacity Act (2005)to ensure that the rights of individual are protected, and they are supported to make their own decisions where possible and that any decisions made on their behalf when they lack capacity are made in their best interests and least restrictive of their rights and freedoms.
8.2.1 Indicate how this will be achieved
This policy will be implemented in accordance with the Guiding Principles of the Mental Capacity Act 2005. (Section 1).
9 Associated documents
- RDaSH safeguarding children manual
- RDaSH care programme approach (CPA) policy
- RDaSH safeguarding adult manual
10 Appendices
10.1 Appendix A Access team protocol for patients who disengage from home treatment
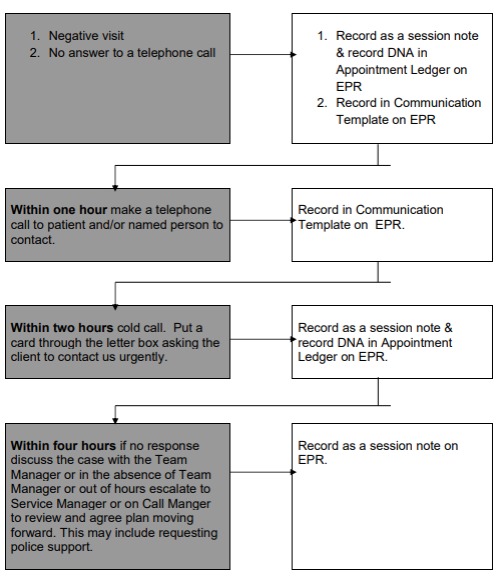
- Negative visit or no answer to a telephone call.
- Record as a session note and record DNA in appointment ledger on EPR and record in communication template on EPR.
- Within one hour make a telephone call to patient or named person to contact.
- Record in communication template on EPR.
- Within two hours cold call. Put a card through the letter box asking the client to contact us urgently.
- Record as a session note and record DNA in appointment ledger on EPR.
- Within four hours if no response discuss the case with the team manager or in the absence of team manager or out of hours escalate to service manager or on call manager to review and agree plan moving forward. This may include requesting police support.
- Record as a session note on EPR.
Document control
- Version: 1.
- Unique reference number: 562.
- Ratified by: Clinical policies review and approval group.
- Date ratified: 3 November 2020.
- Name of originator or author: Head of patient safety.
- Name of responsible individual: Executive director of nursing and allied health professionals.
- Date Issued: 20 November 2020.
- Review date: November 2023.
- Target audience: Clinical staff working on the trust’s patients and carers.
- Description of change: New policy.
Page last reviewed: April 05, 2024
Next review due: April 05, 2025