Contents
1 Introduction
The MHA 1983 provides the legislative framework within which hospital managers are expected to operate in order to ensure that any actions they take fulfil legal requirements. The Mental Health Act Code of Practice 2015 provides guidance to hospital managers on how they should proceed when undertaking duties under the MHA 1983 (chapter 38 the hospital managers discharge power).
These procedures contain a summary of the relevant rules applicable to this part of the MHA 1983. It is by no means exhaustive and is not intended to replace the hospital managers need to be aware of the relevant provisions of the code of practice and reference guide and the MHA 1983 together with relevant case law.
2 Objectives
Section 23 of the MHA 1983 gives the hospital managers the power to discharge an unrestricted patient from detention and patients subject to supervised community treatment orders (SCTO).
The trust has appointed a number of hospital managers to undertake the functions of the Hospital Managers to discharge patients under section 23 of the MHA 1983. The appointees are known collectively as the “trust associate hospital managers” and those who chair the panel hearing are known as “senior trust associate hospital managers”.
The legislation does not define the procedure for reviewing a patient’s detention or CTO; however, the trust associate hospital managers’ conduct of reviews must satisfy the fundamental legal requirements of fairness, reasonableness and lawfulness:
- they must adopt and apply a procedure which is fair and reasonable
- they must not make irrational decisions, that is, decisions which nobody of trust associate hospital managers properly directing themselves as the law, and on the available information, could have made
- they must not act unlawfully, that is, contrary to the provisions of the MHA 1983, any other legislation (including the Human Rights Act 1998 and relevant equality and anti-discrimination legislation)
The guidance set out below on the conduct of meetings and procedures should be followed. In exceptional circumstances, however, it may be necessary to deviate from the suggested conduct or procedure. In such circumstances, advice must be taken from the Mental Health Act office.
3 When to hold a review
Hospital managers:
- may undertake a review at any time at their discretion
- must undertake a review if the patient’s responsible clinician (RC) submits to them a report under section 20 of the MHA 1983 renewing detention or under section 20A extending CTO
- should consider holding a review when they receive a request from (or on behalf of) a patient
- should consider holding a review when the RC makes a report to them under section 25 barring an order by the nearest relative to discharge a patient
In the last two cases, when deciding whether to consider the case, trust associate hospital managers are entitled to take into account whether a tribunal has recently considered the patient’s case or is due to do so in the near future.
Whilst it is desirable for trust associate hospital managers to consider a report renewing a detention or extending an CTO before the current detention period or CTO ends, the RC’s report made under section 20 or 20A provides authority for the patient’s continued detention or CTO until the trust associate hospital managers can consider the case and reach a decision.
4 Principles underpinning review
The trust will ensure that all relevant patients are aware that they may ask to be discharged by the trust associate hospital managers and of the distinction between this and their right to apply for a tribunal hearing.
The exercise of trust associate hospital managers’ functions under section 23 MHA 1983 is also subject to the general law in that the conduct of the review must conform to the legal requirements of fairness, reasonableness and lawfulness (see 2 above). The procedure adopted must conform to the principles of natural justice and the trust associate hospital managers must not make decisions that are irrational or outside their powers.
Where a review is to take place, trust associate hospital managers must consider whether the grounds for continued detention of the patient under the MHA are satisfied.
Generally the trust associate hospital managers must consider the questions below, in the order stated:
For section 2:
- is the patient is still suffering from a mental disorder?
- if so, is the disorder of a nature or degree which warrants the continued detention of the patient in hospital for assessment or for assessment followed by medical treatment?
- ought the detention to continue in the interests of the patient’s health or safety or for the protection of other people?
For other detained patients:
- is the patient still suffering from a mental disorder?
- If so, is the disorder of a nature or degree which makes treatment in a hospital appropriate?
- Is continued detention for medical treatment necessary for the patient’s health or safety or for the protection of other people?
- Is appropriate medical treatment available for the patient?
For patients on CTO:
- is the patient is still suffering from a mental disorder?
- if so, is the disorder of a nature or degree which makes it appropriate for the patient to receive medical treatment?
- if so, is it necessary in the interests of the patient’s health or safety or the protection of other people that the patient should receive such treatment?
- is appropriate medical treatment available for the patient?
- is it still necessary for the RC to be able to exercise the power to recall the patient to hospital, if that is needed?
- is appropriate medical treatment available for the patient?
If the RC has made a report under section 25 barring a nearest relative’s attempt to discharge the patient, the hospital managers should also consider the following question:
Would the patient, if discharged, be likely to act in a manner that is dangerous to other people or themselves?
This last question provides a more stringent test for continuing detention or CTO.
If the panel unanimously disagree with the RC and decide that the answer to this question is “no”, the panel should usually discharge the patient. However, the trust associate hospital managers retain a residual discretion not to discharge in these cases, so panels should always consider whether there are exceptional reasons why the patient should not be discharged.
In all cases, trust associate hospital managers have discretion to discharge patients even if the criteria for continued detention or CTO are met. Hospital managers’ panels must therefore always consider whether there are other reasons why the patient should be discharged despite the answers to the questions set out above.
5 Procedure for renewal of authority
The MHA office will advise the RC eight weeks prior to the date of renewal.
The RC will complete the appropriate paperwork (form H5 or Form CTO7).
The named nurse (for inpatients) will ensure that the patient is advised of his or her rights and will complete the form 14c (appendix A). The care co-ordinator (for community patients) will ensure that the patient is advised of his or her rights and will complete the Form 14c.
The form 14c together with the Form H5 or CTO7 will be forwarded to the MHA office.
The trust associate hospital managers must hold a renewal review hearing, for example, a full managers hearing with all the Care team present, for each renewal of detention or extension of CTO.
The MHA Office will arrange the renewal review hearing.
6 Procedure for renewal review hearing
The MHA administrator will write to the patient advising them of the recommendation for the renewal and subject to the patient’s wishes, the nearest relative will be informed in writing.
The MHA Office will invite the patient and professionals involved in the patients care to attend a renewal review hearing.
Follow 7.2 to 7.18 for the process to be undertaken.
7 Procedure for an appeal to hospital managers
The relevant MHA office will acknowledge receipt of the appeal application from the patient in writing.
A report, addressing all the issues will be requested, from the responsible clinician (appendix B or C), AMHP or care co-ordinator (appendix D), named nurse (appendix E).
These reports should be timely and up-to-date, or, a written addendum submitted or verbal update given, at the hearing. One week prior to the hearing the MHA office will contact the report writers to ascertain if an addendum is required.
The relevant MHA office will convene a panel of 3 trust associate hospital managers including a senior trust associate hospital manager who will act as chair, ensuring all the professionals, and or nearest relative are available to attend the managers hearing.
The panel of trust associate hospital managers must consist of at least three members, one of whom will be a senior trust associate hospital manager. The panel will not be able to sit unless there are 3 members present. In the event of only two being present the hearing should be adjourned and re-convened.
The relevant MHA office will confirm in writing the arrangements for the managers hearing to all participants. The time of the hearing will be arranged to enable all participants to attend directly from the ward or offices. Every effort will be made to put the patient and the nearest relative or supporter at ease.
The relevant MHA office will, one week in advance of the hearing, scrutinise all the relevant documentation to be put before the panel hearing and will complete the administration checklists (appendix F to H).
The reports from the RC, AMHP or care co-ordinator, named nurse and professionals involved, will be given to the panel members on the day of the hearing.
The panel will be supported by the relevant MHA administrator who will provide them with copies of:
- form H5 renewal of authority for detention
Or:
- form CTO7 report extending the community treatment period
- form 14c section 132 advice to a detained patient of their rights under the MHA 1983
- copies of all the professional reports
- copy of an up-to-date care plan
And:
- hospital managers decision form
The panel will meet in private, at least 1 hour prior to the start of the hearing, to read the reports and to identify any matters contained in the reports that require further explanation or clarification. In the event of there being reports with items for non-disclosure, the panel must discuss the relevance of this prior to the start of the hearing, if necessary, with the professionals concerned and decide if it is appropriate to withhold this information.
The trust associate hospital managers will, prior to the start of the hearing, establish via the patient, if they wish to speak to them privately.
All participants will attend the managers hearing as a group.
In reviewing the patient’s continued detention the trust associate hospital managers will ensure that the responsible clinician, AMHP or care co-ordinator, named nurse and other professionals involved are actively and positively questioned.
In the event of the patient not wishing to be accompanied to the managers hearing but subject to consent, the views of the nearest relative will be sought and represented by the appropriate professional, for example, AMHP or care co-ordinator.
At the conclusion of the managers hearing the chair of the panel will ensure the decision and reasons for it are communicated orally to the patient, to the accompanying nearest relative or supporter, to the other professionals involved and documented in the patient’s case notes via the appropriate decision form (appendix I to N).
If the patient does not wish to return to the room to hear the decision then the communication of the decision may be delegated to the care co-ordinator or named nurse.
A decision to discharge the patient can only be made if 3 or more members of the panel (who between them make up a majority) are satisfied from the evidence presented to them that the answer to any of the criteria is ‘no’, the patient should be discharged, unless there is an exercise by the panel of its discretionary power referred to in 4 above.
Should the hospital managers discharge from detention, this is effective immediately although the patient may have expressed willingness to remain in hospital informally.
The relevant MHA office will confirm the decision in writing to the patient and will communicate that information to any non-attending relative who has expressed views, with the consent of the patient.
In the event of the panel making recommendations, the relevant MHA office will ensure that the recommendation is passed onto the relevant professional or undertake the action as necessary. The MHA office will then record this action and report on this via the local mental health legislation monitoring groups and then quarterly to the mental health legislation operational group. The MHA office will report the outcome of any recommendation to the panel members in a safe and secure manner.
Copies of the record of the managers hearing together with the hospital managers confirmation letter will be placed in the patient’s mental health act file.
8 Appendices
8.1 Appendix A Form 14c
8.2 Appendix B Report requirement for the responsible clinician
This report must describe the patient’s relevant medical history, to include:
- full details of the patient’s mental state, behaviour and treatment for mental disorder
- in so far as it is within the knowledge of the person writing the report, a statement whether the patient has ever neglected or harmed himself, or has ever harmed other persons or threatened them with harm, at a time when he was mentally disordered, together with details of any neglect, harm or threats of harm
- an assessment of the extent to which the patient or other persons would be likely to be at risk if the patient is discharged by the managers and how any such risks could best be managed
- an assessment of the patient’s strengths and any other positive factors that the managers should be aware of in coming to a view on whether he should be discharged
- if appropriate, the reasons why the patient might be treated in the community without continued detention in hospital, but should remain subject to recall on supervised community treatment
I am asked to remind you that a copy of the authority’s statement, including medical reports, will be sent to the patient unless submitted as a separate document and endorsed: “not to be disclosed to the applicant”. However, it should be noted that unless this is going to cause “serious harm to the patient” the managers will normally ask for disclosure.
The managers draw attention to the fact that all documents must be disclosed to the patient’s representative if he or she is a solicitor, doctor or in the managers’ opinion is otherwise suitably qualified.
8.3 Appendix C Report requirements for the supervised community treatment order
CTO reports must include the following information:
- details of the original authority for the patient’s supervised community treatment under the Mental Health Act 1983.
- the name of the patient’s responsible clinician and the length of time the patient has been under their care
- full details of the patient’s mental state, behaviour and treatment for mental disorder, and relevant medical history
- in so far as it is within the knowledge of the person writing the report, a statement whether the patient has ever neglected or harmed himself, or has ever harmed other persons or threatened them with harm, at a time when he was mentally disordered, together with details of any neglect, harm or threats of harm
- an assessment of the extent to which the patient or other persons would be likely to be at risk if the patient is discharged by the Managers and how any such risks could best be managed
- an assessment of the patient’s strengths and any other positive factors that the Managers should be aware of in coming to the view on whether he should be discharged
- the reasons why the patient can be treated as a community patient without continued detention in hospital, and why it is necessary that the responsible clinician should be able to exercise the power under section 17E(1) of the Mental Health Act 1983 to recall the patient to hospital
- details of any specific conditions in force regarding the patient under section 17B of the Mental Health Act 1983
I am asked to remind you that a copy of the authority’s statement, including medical reports, will be sent to the patient unless submitted as a separate document and endorsed: “not to be disclosed to the applicant”. However, it should be noted that unless this is going to cause “serious harm to the patient” the managers will normally ask for disclosure.
The managers draw attention to the fact that all documents must be disclosed to the patient’s representative if he or she is a solicitor, doctor or in the managers’ opinion is otherwise suitably qualified.
8.4 Appendix D Social circumstances report for hospital managers template
8.5 Appendix E Nursing report template
8.6 Appendix F Renewal review admin checklist
8.7 Appendix G Attendance sheet
8.8 Appendix H Background information
8.9 Appendix I Decision forms section 2
8.10 Appendix J Decision forms treatment sections
8.11 Appendix K Decision forms supervised community treatment order
8.12 Appendix L Decision forms section 25 barring section 2 by nearest relative
8.13 Appendix M Section 25 barring section 3 by nearest relative
8.14 Appendix N Section 25 barring supervised community treatment order by nearest relative
8.15 Appendix O Hearing flowchart
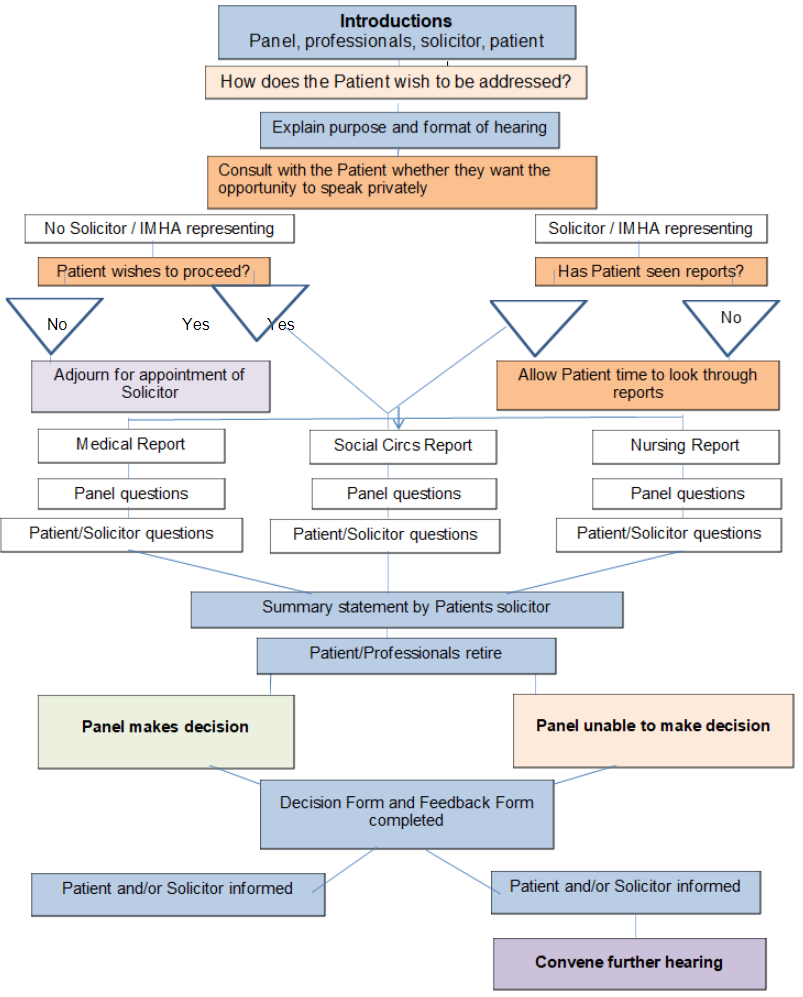
- Introductions, panel, professionals, solicitor, patient.
- How does the patient wish to be addressed?
- Explain purpose and format of hearing.
- Consult with the patient whether they want the opportunity to speak privately.
8.15.1 No solicitor or independent mental health advocate (IMHA) representing
Patient wishes to proceed?
- No, adjourn for appointment of solicitor.
- Yes, proceed to 8.15.3 Reports.
8.15.2 Solicitor or independent mental health advocate (IMHA) representing
Patient wishes to proceed?
- No, allow patient time to look through reports
- Yes, proceed to 8.15.3 Reports.
8.15.3 Reports
8.15.2.1 Medical report
- Panel questions.
- Patient or solicitor questions.
- Proceed to 8.15.4 summary statement by patient solicitor.
8.15.2.2 Social Circs report
- Panel questions.
- Patient or solicitor questions.
- Proceed to 8.15.4 summary statement by patient solicitor.
8.15.2.3 Nursing report
- Panel questions.
- Patient or solicitor questions.
- Proceed to 8.15.4 summary statement by patient solicitor.
8.15.4 Summary statement by patient solicitor
- Patient or professionals retire:
- panel makes decision
- panel unable to make decision
- Decision form and feedback form completed.
- Patient and, or solicitor informed.
- Convene further hearing.
Document control
- Version: 8.
- Approved by: Mental health legislation operational group.
- Date approved: 14 July 2022.
- Name of originator or author: MHA manager.
- Name of responsible individual: Mental health legislation operational group.
- Date issued: 28 July 2022.
- Review date: May 2025.
- Target audience: Trust associate hospital managers or all trust staff.
Page last reviewed: June 04, 2025
Next review due: June 04, 2026
Problem with this page?
Please tell us about any problems you have found with this web page.