1 Policy summary
This policy informs colleagues, patients and visitors of the smoke free policy for Rotherham Doncaster and South Humber Trust (RDaSH). This policy was created to protect colleagues, visitors and patients from the harmful effects of smoking, whether that be first or second hand smoke. This policy outlines the support available to patients, colleagues and visitors.
2 Introduction
Smoking is a leading cause of preventable death in England. It is linked to diseases such as cancer, heart disease, and respiratory conditions. It also impacts mental health and can increase medication needs for those with mental health problems. In response, the government aims to reduce smoking prevalence to 5% by 2030.
Hospitals should be smoke-free both indoors and outdoors to protect everyone from the harmful effects of smoking. This includes offering treatment to smokers who wish to quit and supporting those who do not wish to quit in managing their smoking while on trust premises.
2.1 Legal position
The trust is required by law to provide a safe environment free from health risks such as second-hand smoke. The Health and Safety at Work Act (1974) and the Health Act (2006) mandate smoke-free regulations, which apply to all trust premises, including buildings, grounds, and vehicles.
3 Purpose
This policy aims to:
- promote a smoke-free environment for all trust premises
- protect all individuals from the health risks of second-hand smoke
- safeguard colleagues from smoke exposure at work
- support patients and colleagues in quitting smoking by offering nicotine replacement and behavioural support
- allow colleagues to conduct searches to maintain a smoke-free environment, including random or routine searches of patients with unescorted leave (refer to the searching of a person (patient and visitor) or their property policy)
- reduce fire risks associated with smoking
4 Scope
This policy applies to all colleagues, patients, visitors, and others on trust premises or during trust service delivery.
4.1 Exclusions
St John’s Hospice is exempt from the general smoke-free policy for patients, who may smoke in designated outdoor areas. Smoking is prohibited indoors. Patients at St John’s Hospice can access smoking cessation services. All other colleagues and visitors must comply with the smoke-free policy on hospice premises. All palliative community patients are requested to refrain from smoking indoors during home visits and for an hour before colleagues arrive.
5 Procedure
5.1 Quick guide
5.1.1 Key point 1
- RDaSH is a smoke free trust. Smoking is prohibited on all RDaSH sites (with an exemption for St John’s Hospice). This includes all indoor and outdoor areas. If colleague choose to smoke, they must do so off site and must not be identifiable as a health care worker. This means changing out of uniform and removing badges and lanyards.
5.1.2 Key point 2
- Vaping is permitted in outdoor areas for patients and visitors. Colleagues cannot vape on trust premises or in trust vehicles. Vaping is not permitted inside any trust buildings or buildings used for RDaSH appointments in the community.
5.1.3 Key point 3
- Patients are prohibited from smoking on escorted section 17 leave.
5.1.4 Key point 4
- Colleagues working in the community should request a smoke free environment when visiting a patient’s home. Arrangements should be made with patients prior to your visit to prevent the risk of second-hand smoke. Colleagues should request that patients and, or anyone else present refrain from smoking indoors during the visit and for an hour before colleagues arrive.
5.1.5 Key point 5
- All breaches of the smoke free policy should be reported via the incident reporting system (RADAR from 1 May 2025).
5.1.6 General approach
- Promote and maintain a smoke-free environment.
- Offer tobacco treatment service support to patients and colleagues who are smokers.
- An approach to discuss breaches of the smoke free policy should only be made once to avoid conflict. The trust will apply a no excuse for abuse approach to any individual who becomes abusive when reminded of the smoke free policy.
- Colleagues are expected to adhere to the principles taught in the trust’s conflict resolution and reducing restrictive interventions training courses.
5.2 Prohibited and permitted items
- Patients and visitors to trust premises will be made aware of the smoke free policy through signs, posters, leaflets and conversations with colleagues.
- Patients and visitors will be informed about prohibited items (tobacco, cigarettes, cigars, lighters, nicotine pouches, see appendix J) through signage and communication.
- Prohibited item issues should be addressed with visitors; visitors who provide prohibited items to patients will be asked to support the patient’s treatment plan in the first instance. Persistent offenders may be banned from future visits.
- Smoking paraphernalia should be stored securely in lockers; colleagues must not bring such items onto wards for themselves or patients.
- For guidance on specific products, contact the QUIT team at rdash.quit@nhs.net.
6 Community services
6.1 Assessment
- During the initial admission assessment, document patients’ smoking habits using the trust smoking template on SystmOne (see appendix C)
- Questions should cover:
- current use of tobacco or e-cigarettes
- past attempts to quit and methods used
- reasons for past or current smoking habits
- refer all smoking patients to the Healthy Hospitals team for in-house smoking cessation support unless they opt out
- important, screen all community patients 18 years or older on initial assessment or at least annually, including non-smokers
6.2 Referrals and treatment
- Review smoking status at least annually, or during dialog reviews.
- Where possible, carry health promotional materials about smoking cessation services Staff can be signposted to the intranet page too for relevant information.
- When a patient is likely to have contact with inpatient services, inform patients about the smoke-free policy and inform them that support to abstain from smoking will be offered during any inpatient stay.
- For referral pathways please see appendix D.
6.3 Visiting patients who smoke at home
- Request a smoke-free environment during home visits. include this request in appointment letters and verbal communications.
- Consider alternative arrangements if compliance is an issue:
- smoke in a separate room before visits
- use nicotine patches before or during appointments
- attend appointments at a clinic instead of home visits
- Include details of any alternative arrangements in the patient’s care plan.
- Review cases of persistent non-compliance and adjust the treatment plan as needed.
7 Inpatient services
7.1 Admission and assessment
- All trust inpatient wards and premises are smoke-free (this includes all mental health and physical health wards). St John’s Hospice is the only exception to this and provisions for this are stated in section 3.1 of this policy.
- Patients may vape outside while on site. This includes ward gardens or courtyards.
- Vaping in any indoor area is prohibited for all patients, colleagues and visitors.
- The above restrictions must be explained to patients and visitors before admission or soon as the patient arrives.
- Screen all patients within 24 hours of admission or readmission using the trust inpatient smoking screening questionnaire on SystmOne (see appendix E).
During admission:
- assess smoking status and past attempts to quit or reduce their consumption
- offer abstinence or harm reduction support and refer to the QUIT service
- all inpatients, including non-smokers and those transferred between different localities, must be screened on admission
- secure any smoking paraphernalia found on patients and store it in ward lockers, patients may access these items during unescorted leave but must surrender them upon return
- if patients refuse to hand over items, refer to the searching of a person or their property policy
- during the first 72 hours post admission, offer all smokers very brief advice (VBA) along with rechargeable vapes or nicotine replacement therapy, vapes cannot be given to anyone under the age of 18
- follow the QUIT approach:
- Q, ask and record smoking status
- U, understand addiction level
- I, inform about health benefits
- T, initiate treatment and refer to services
- if a patient declines cessation support, they must remain smoke-free on trust premises, a care plan should be developed for smokers detailing abstinence support during their stay
7.1.1 Trust supplied nicotine replacement therapy (NRT) and vapes
- All nicotine replacement therapy (NRT) is available to patients who smoke at any time during their admission, free of charge.
- Vapes are available to all patients who smoke, free of charge, for the first 72 hours of their admission. After 72 hours, patients who are engaging with a quit attempt or reduction with the view to quit will be eligible for trust supplied vapes for a 12-week period.
- If a patient does not want to make a quit attempt, they will be offered other forms of nicotine replacement therapy (NRT) (lozenges, patches, inhalators) to support abstinence during their admission.
- Vapes must be transcribed by colleagues for the first 72 hours following admission and subsequently for those patients who agree to engage with the QUIT programme,
- Vapes will only be administered to patients if transcribed. No vapes will be administered beyond the number transcribed on their drug card. Patients will need to provide their own supply once the transcribed number have been administered. These must be approved rechargeable products.
- After the 12-week supported QUIT period, free vapes will no longer be supplied by the trust. Patients will need to source their own trust approved products. Any patients who are unable to source their own products for any reason must be discussed by the multi-disciplinary team (including the involved tobacco treatment advisor (TobTa)) as an exception. Agreement to continue to supply beyond the 12-week cut-off point must be approved by the service manager or matron. If OOH this must be escalated to silver on call for approval. (Ideally a patient coming to the end of their 12 weeks will be prepared for this situation by the Healthy Hospitals team so it doesn’t become an urgent request).
- If at any point you are unsure about the appropriate nicotine replacement therapy or vape for a patient, please contact the nominated tobacco treatment advisor or the Healthy Hospitals team.
7.2 Risk management on inpatient wards
- Assessment: all smokers should have a smoking risk assessment (see appendix G) and a risk management care plan.
- Key risks:
- covert smoking, especially in bed
- prohibited items (for example, ignition sources, cigarettes) brought onto the ward by visitors or by the patient after a period of leave
- increased risk of absconding
- risk of ingestion of vape batteries as self-harm
- Reference, see appendix H for management of rechargeable vaping devices.
7.3 Medication management
- Impact of smoking: smoking affects drug metabolism, requiring dose adjustments when smoking status changes for some medications.
- Monitoring: closely monitor medication levels, especially for drugs with a narrow therapeutic index like clozapine. it is recommended that plasma levels of clozapine should be measured before smoking cessation commences, reducing the dose as needed and repeating plasma levels one week after cessation, to enable more accurate and timely monitoring and adjustment of medications.
- Resources: consult the specialist pharmacy service or the trust pharmacy team for advice.
7.4 Section 136 assessments
- Vaping or nicotine replacement therapy (NRT) provision: offer trust approved rechargeable vapes or 24-hour nicotine replacement therapy based on smoking habits:
- 21mg per 24 hours for greater than 10 cigarettes per day
- 14mg per 24 hours for less than 10 cigarettes per day
- Documentation: the use of these products is to be recorded in the patient record.
7.5 Seclusion
- Nicotine replacement: offer nicotine replacement therapy during seclusion, patches, lozenges, inhalators only; vapes are not permitted in seclusion.
- Risk assessment: provide the above detailed nicotine replacement therapy based on individual risk assessments.
7.6 Visitors
- Policy: all visitors must adhere to the trust’s smoke free policy.
- Information: provide information about smoke free status of the trust in carer’s information packs or on arrival. if this is not possible, visitors should be informed of this on arrival.
- Storage: visitors must store smoking paraphernalia in lockers.
- Vaping: allowed only in designated outdoor areas.
7.7 Environmental management
- Routine checks: designate a colleague each shift to monitor compliance and check the environment.
- Removal: patients and visitors breaching the smoke free policy are responsible for clearing up any smoking related rubbish such as cigarette butts, packaging or ash that they have created. Any that is not removed by those using it will be removed by facilities and domestic teams as part of routine cleaning duties.
7.8 Access to information
- Display: wards must display health promotion materials on the harms of smoking and the cessation support available.
7.9 Non-compliance
- Action: for persistent non-compliance, conduct a multi-disciplinary team (MDT) review to determine actions and update the care plan. The trusts supportive observation of inpatients who are identified as posing a significant risk to themselves or others policy should be used for patients who are identified as posing a fire risk due to covert smoking.
- Support: discuss in the Patient Safety Oversight Group (PSOG) and report non-compliance via the incident reporting system (see section 8.1).
7.10 Violence and aggression
- Handling: if a patient becomes violent or aggressive in relation to the smoke free policy, de-escalation is the preferred option. There is no expectation that colleagues should put themselves at risk.
- Protocol: follow the reducing restrictive interventions policy and ensure the patient make arrangements to avoid future breaches, which should be recorded in a care plan.
7.11 Section 17 leave
- Purpose: section 17 leave should not be used to facilitate smoking.
- Rationale: smoking or “smoking leave” has been found to add no therapeutic value to a patients care. Smoking is known to increase symptoms of poor mental and physical health.
7.12 Discharge
- Discharge plan: patients should be asked if they wish to continue with support to stop smoking when they are discharged. If they would like support, it should be included in their discharge plan and the following steps should be followed:
- nicotine replacement therapy and vapes: provide 2 weeks’ worth of nicotine replacement therapy products or 1 weeks’ worth of vapes. Post-discharge, the Healthy Hospitals team will provide rechargeable vapes and follow up the patients in the community (Doncaster and Rotherham residents)
- North Lincolnshire residents can be referred to the community smoking cessation services on discharge and follow-up telephone support will also be provided from the Healthy Hospitals Team if required.
- referral, all patients will be given a follow-up call once they leave hospital from the Healthy Hospitals team to offer to continue support post discharge
- documentation, where a patient has stopped smoking, ensure that discharge notes make clear that blood plasma levels may be affected, and certain medication dosages may need to be adjusted
8 Breaches and reporting
8.1 Reporting smoking-related incidents
- Reporting: all breaches must be logged on the trust incident reportingir1 system as per the trust incident management policy. This helps monitor trends and manage risks.
- Reporting categories:
- type of incident: security, loss, or damage
- cause group: security, loss, theft, or damage
- cause: smoking policy breach or concern
- Violence and aggression: if violence or aggression is involved, log the incident under violence and aggression with smoking as a secondary cause.
- Responsibility: ward colleagues must report incidents or ask a manager to do so if they lack access to the incident reporting system.
- Issues:
- report any issues with completing incident reports due to staffing capacity to the ward manager, service manager or modern matron
- persistent non-compliance with the smoke free policy should be reported to the modern matron and service manager
- complaints should first be handled by the ward and team manager; unresolved issues can be escalated to pals or through the formal complaint’s procedure
8.2 Sale of tobacco products
- Prohibition: no tobacco sales are allowed on trust premises. Selling, transporting, or possessing illegal tobacco products is a criminal offence.
- Disposable vapes: from 1 June 2025 it will become illegal to supply, sell or purchase disposable vapes. Only rechargeable vapes will be available for use to support patients in their QUIT journey. Any vapes brought onto site for use by visitors or patients must be rechargeable. Disposable vapes will be confiscated and disposed of accordingly.
- Enforcement: colleagues who suspect illegal tobacco products are being used on trust premises should search for and remove it. The trust will cooperate with law enforcement. Any illegal activity by colleagues will result in disciplinary action.
9 Colleague support
9.1 Smoking cessation support
- Support: the trust offers up to 12 weeks of smoking cessation support per year for employees in Rotherham, Doncaster or North Lincolnshire. Colleagues are able to access free nicotine replacement therapy (NRT) and vapes during this 12-week period.
- Incentives: Colleagues who successfully quit can receive gift vouchers (£10 at 4 weeks, £30 at 12 weeks). To sign up, email either:
- Email: rdash.quit@nhs.net
- Email: healthandwellbeing@nhs.net
9.2 Workplace responsibilities
- Restrictions:
- colleagues must not smoke, chew tobacco, or vape anywhere on trust grounds. This includes inside trust premises or inside trust vehicles. Colleagues who struggle with this can be referred to the colleague service at any time for support
- colleagues are not entitled to smoking or vaping breaks, if colleagues wish to vape or smoke this must be done during their allotted breaks and in accordance with the smoke free policy
- Uniform: no smoking or vaping whilst wearing uniform or if identifiable as a health worker, irrespective of whether they are on duty or on trust premises. Identity badges should be removed and clothes should be changed. Staff in breach of this will be managed in accordance with the trust disciplinary procedure.
- Vehicles: smoking and vaping are prohibited in trust vehicles and while traveling with trust colleagues.
- Disciplinary: continued non-compliance may lead to disciplinary action.
9.3 Colleague breaches
- Expectations:
- colleagues should promote a smoke free environment and avoid condoning, facilitating or advocating tobacco smoking
- all trust colleagues are prohibited from purchasing or providing tobacco products for patients, colleagues must not use tobacco as a reward for patients
- breaches should be reported to line managers, repeated breaches may result in action through the trust disciplinary policy and personal responsibility framework
10 Training implications
10.1 Very brief advice training, all colleagues
- How often should this be undertaken: Every 3 years.
- Length of training: 30 minutes.
- Delivery method: Face-to-face or Microsoft Teams.
- Training delivered by whom: Healthy Hospitals team.
- Where are the records of attendance held: Electronic staff record (ESR).
10.2 Transcribing nicotine replacement therapy (NRT), all colleagues issuing pharmacotherapy
- How often should this be undertaken: Every 3 years.
- Length of training: 30 minutes.
- Delivery method: Face-to-face or Microsoft Teams.
- Training delivered by whom: Healthy Hospitals team.
- Where are the records of attendance held: Electronic staff record (ESR).
As a trust policy, all colleagues need to be aware of the key points that the policy covers. Colleagues can be made aware through:
A variety of means such as:
- all user emails for urgent messages
- one to one meetings or supervision
- continuous professional development sessions
- posters
- group supervision
- special meetings
- intranet
- team meetings
- local induction
- chief executive’s video log
- trust induction
11 Equality impact assessment screening
To access the equality impact assessment for this policy, please email rdash.equalityanddiversity@nhs.net to request the document.
11.1 Privacy, dignity and respect
The NHS Constitution states that all patients should feel that their privacy and dignity are respected while they are in hospital. High Quality Care for All (2008), Lord Darzi’s review of the NHS, identifies the need to organise care around the individual, “not just clinically but in terms of dignity and respect”.
Consequently, the trust is required to articulate its intent to deliver care with privacy and dignity that treats all patients with respect. Therefore, all procedural documents will be considered, if relevant, to reflect the requirement to treat everyone with privacy, dignity, and respect, (when appropriate this should also include how same sex accommodation is provided).
11.1.1 How this will be met
There are no additional requirements in relation to privacy, dignity and respect.
11.2 Mental Capacity Act (2005)
Central to any aspect of care delivered to adults and young people aged 16 years or over will be the consideration of the individuals’ capacity to participate in the decision-making process. Consequently, no intervention should be carried out without either the individual’s informed consent, or the powers included in a legal framework, or by order of the court.
Therefore, the trust is required to make sure that all employees working with individuals who use our service are familiar with the provisions within the Mental Capacity Act (2005). For this reason, all procedural documents will be considered, if relevant to reflect the provisions of the Mental Capacity Act (2005) to ensure that the rights of individual are protected, and they are supported to make their own decisions where possible and that any decisions made on their behalf when they lack capacity are made in their best interests and least restrictive of their rights and freedoms.
11.2.1 How this will be met
All individuals involved in the implementation of this policy should do so in accordance with the guiding principles of the Mental Capacity Act (2005) (section 1).
12 Links to any associated documents
- Physical health policy
- Supportive therapeutic observation policy
- Reducing restrictive interventions (RRI) policy (formerly prevention and management of violence and aggression (PMVA) policy)
- Searching of a person or their property policy
- Personal responsibility framework procedure
- Disciplinary policy
- Incident management policy
- Guidelines for nicotine management therapy and attached units (staff access only)
13 References
- Department of Health and Social Care (2011) No Health Without Mental Health: a cross-government outcomes strategy
- Department of Health and Social Care (2017) Smoke-free generation: tobacco control plan for England
- Department of Health and Social Care (2017) Tobacco control plan: delivery plan 2017 to 2022
- Harker and Cheeseman (2016) The Stolen Years: Mental Health and Smoking Action Report, Action on Smoking and Health (ASH)
- Health and Safety Executive (2020) Health and Safety at Work Act (1974)
- Health and Safety Executive (2020) Health Act (2006)
- NHS Digital (2018) Statistics on Smoking, England
- NICE (2021) Tobacco: preventing uptake, promoting quitting and treating dependence
- NICE (2013) smoking: acute, maternity and mental health services, public health guideline (ph48)
- NICE (2013) smoking: harm reduction
- PHE (2020) health matters: smoking and mental health Public Health England guidance
14 Appendices
14.1 Appendix A responsibilities, accountabilities and duties
14.1.1 The trust
The trust has a duty of care and a duty of confidentiality to ensure that all aspects of healthcare record keeping are properly managed. The trust must adhere to the legislative, statutory, and good practice guidance requirements relating to healthcare records management.
14.1.2 The chief executive
- Is responsible for overall health, safety, and welfare of the trust.
- Has delegated this function is delegated to the chief operating officer and senior responsible officer who are accountable for policy implementation.
- Is responsible for ensuring the trust has effective policies and procedures for a smoke-free environment.
- Is responsible for oversee compliance with relevant legislation.
14.1.3 Executive director of nursing and allied health professionals, deputy director of nursing
- The deputy director of nursing, delegated by the executive director of nursing and AHP’s, oversees the QUIT program and ensures adherence to the policy.
14.1.4 Senior managers of the trust
The Health Act (2006) section 8 and sub section 1 states that ‘it is the duty of any person who controls or is concerned in the management of smoke free premises to cause a person smoking there to stop smoking’ and therefore directors, care group directors and managers are responsible for:
- raising awareness and ensuring effective communication of the policy
- ensuring screening of every patient within 24 hours of admission or registration and recording the status on SystmOne
- maintaining a safe, healthy environment by applying the policy
- addressing concerns and take action regarding non-compliance
- completing risk assessments for passive smoking exposure
- ensure patients are informed and supported in managing or quitting smoking
14.1.5 All employees
- Comply with and support the smoke-free policy.
- Report non-compliance incidents to line managers and via the trust ir1 incident reporting system.
- Notify managers of passive smoking incidents and request patients to smoke outside or to refrain from smoking inside for an hour before visits.
- Request that patients extinguish cigarettes and move away from trust premises.
- Prevent and manage ignition sources and smoking paraphernalia on trust premises.
- Be aware that persistent non-compliance may lead to disciplinary action in accordance with the trusts’ disciplinary policy.
14.2 Appendix B monitoring arrangements
14.2.1 Policy implementation
- Who by: All managers.
- Reported to: Care group quality meetings.
- Frequency: As incidents arise.
14.2.2 Smoking related fire incidents
- Who by: Health and Safety team.
- Reported to: Health, safety and security forum.
- Frequency: Bi-monthly.
14.2.3 Non-fire smoking related incidents
- Who by: All managers.
- Reported to: Care Group Quality meetings.
- Frequency: Bi-monthly.
14.3 Appendix C location of the trust smoking template for screening of mental health community services patients
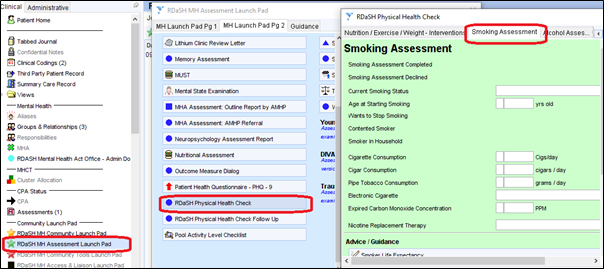
Located under “RDaSH MH Assessment Launch Pad”, “RDaSH Physical Health Check”, then “Smoking Assessment”.
14.4 Appendix D Referral routes for trust community patients who opt into receiving smoking cessation support
14.4.1 Doncaster
14.4.1.1 Option 1 (preferred)
In-house healthy hospitals service by either:
- using a referral form on SystmOne (see appendix H)
- Email: rdash.quit@nhs.net
14.4.1.2 Option 2
If option 1 is not available or patient explicitly states, they would like to be supported by an external service.
External Yorkshire smoke free service by contacting:
- Phone: 0800 612 0011
- Phone: 0330 660 1166
- Email: swy-tr.y-smokefree@nhs.net
14.4.2 Rotherham
14.4.2.1 Option 1 (preferred)
In-house healthy hospitals service by either:
- using a referral form on SystmOne (see appendix H)
- Email: rdash.quit@nhs.net
14.4.2.2 Option 2
If option 1 is not available or patient explicitly states, they would like to be supported by an external service.
External get healthy Rotherham service by contacting:
- Phone: 01709 718 720
- Email: gethealthyrotherham@nhs.net
14.4.3 North Lincolnshire
14.4.3.1 Option 1 (preferred)
In-house healthy hospitals service by either:
- using a referral form on SystmOne (see appendix H)
- Email: rdash.quit@nhs.net
14.4.3.2 Option 2
If option 1 is not available or patient explicitly states, they would like to be supported by an external service.
North Lincolnshire healthy lifestyles service contact:
- Phone: 01724 298 212
- Email: healthylifestyles@nhs.net
14.5 Appendix E referral form for trust patients to the smoking cessation team
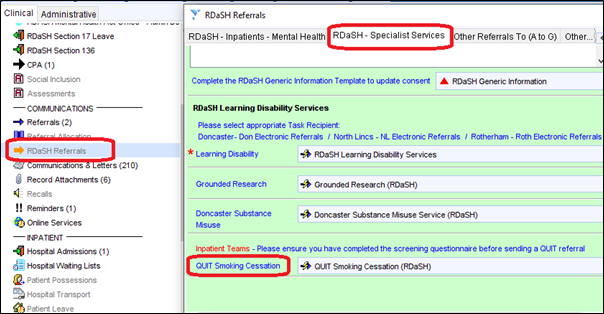
Located under “RDaSH Referrals”, “RDaSH Specialist Services”, then “QUIT Smoking Cessation”.
14.6 Appendix F flowchart for the transcription of vapes

- New patient admitted onto the ward.
- Smoking status template completed on SystmOne by admitting clinician.
- If non smoker no further action needed.
- If smoker, admitting clinician discusses the smoke free policy, nicotine replacement therapy options and will transcribe accordingly.
- Admitting clinician provides very brief advice (VBA) on smoking cessation.
- Healthy Hospitals team triage all new admissions and visit all inpatient smokers within 72 hours to discuss QUIT programme.
- Vapes are transcribed for the first 72 hours until patients decide if they wish to engage with QUIT Programme.
- If patient is engaged with QUIT programme:
- vapes will be transcribed for a maximum of 12 weeks
- after 12 weeks, patients on the QUIT programme must provide their own vape products
- nicotine patches and lozenges can still be transcribed if required
- If after 72 hours, patients not engaged with QUIT programme:
- need to provide their own vape products
- nicotine patches and lozenges can still be transcribed if required
14.6.1 Vapes will only be provided if transcribed
- Vapes will not be provided by the ward to any patient, regardless of whether they are on the QUIT programme or not, unless transcribed.
14.6.1.1 Once discharged
- Patients can access the “swap to stop” vapes available to help support the transition period from hospital to home.
- Support will be provided by the Healthy Hospitals team during this transition period (Rotherham and Doncaster residents only)
14.6.1.2 Exceptions
- The smoke free policy is not applicable to patients at the Hospice who are smokers at their end of life or admitted for symptom control.
- Patients who reach the 12-week timeline for vape provision but have no means of suppling their own vapes (maybe a formal patient with no visiting family or friends to fetch the products into the ward for them or may not have the financial means to buy their own vape products), will be discussed at multi-disciplinary team and a plan agreed to meet this need (the plan will need care group approval if vapes are to be transcribed beyond the 12-week window).
14.7 Appendix G smoking risk assessment for inpatient services
Refer to appendix G: smoking risk assessment for inpatient services (staff access only).
14.8 Appendix H electronic cigarettes guidance
14.8.1 National guidance
- Overview: e-cigarettes (vapes) are battery-powered devices delivering nicotine via inhaled vapor. they can be nicotine-containing or nicotine-free and are widely used as a smoking cessation aid. Public Health England (PHE) supports their use for smokers, as they are less harmful than smoking.
- Support: the NHS long term plan (2019) and care quality commission (CQC, 2018) endorse the use of e-cigarettes in mental health and learning disability services as a smoking cessation tool.
14.8.2 Health and safety of e-cigarettes
- Health impact: e-cigarettes are considered at least 95% less harmful than smoking but are not risk-free. PHE advises reporting any adverse reactions to e-cigarettes via the yellow card scheme.
- Exposure risk: the risk to bystanders from e-cigarette vapor is low, though those with respiratory conditions may be sensitive. Adjustments should be made as needed for comfort.
- The replaceable vape pods and nicotine replacement therapy patches must be disposed of appropriately to reduce littering and the negative impacts on the environment.
14.8.3 Types of e-cigarettes
- Pod vapes: small, rechargeable with replaceable pods containing e-liquid.
- Vape pens: pen-shaped, refillable with e-liquid; often have adjustable settings.
- Box kits or mods: box-shaped devices with larger batteries and adjustable power settings.
- Heat not burn products (see appendix J).
14.8.4 E-cigarettes permitted on trust premises
14.8.4.1 Inpatients
- Offer nicotine replacement products, including rechargeable e-cigarettes, on admission. Authentic personal devices should be inspected and can be restricted if counterfeit
- Vaping is permitted outdoors but not indoors. Patients who are in isolation for a health reason (such as COVID-19) may not vape in their rooms and should be offered alternative nicotine replacement therapy (patches, inhalators and lozenges).
14.8.4.2 Community patients, visitors, and colleagues
- Community patients can use personal vapes outdoors and should be referred to the healthy hospitals service. Contact rdash.quit@nhs.net for referrals.
- Visitors may use personal vapes outdoors but cannot charge them on-site.
- Colleagues may vape off-site, not in uniform or trust vehicles, they can access QUIT support at rdash.quit@nhs.net.
- Smoking paraphernalia must be stored in lockers, not on wards.
14.8.4.3 E-cigarettes and fire safety
- Risks: fires from e-cigarettes are rare but can occur due to malfunctioning lithium batteries. Lithium batteries can short circuit leading them to heat up uncontrollably (thermal runaway).
- Safety measures:
- use only the designated charger
- do not leave charging devices unattended or overnight
- store batteries and chargers in a cool, dry place
- avoid charging near flammable or combustible materials or medical oxygen
- report any safety concerns to the estates team
14.8.4.4 Self-harm and ligature risks
- Risk assessment: conduct individual risk assessments for e-cigarettes to ensure safe use and storage.
- Storage: store devices centrally if there are safety concerns and supervise their use. E-liquids should be managed carefully to prevent ingestion risks.
- Charging cables: charging cables may present a ligature risk. A risk assessment should be completed for any patient who has a charging cable.
14.8.4.5 Risk assessment and general management
Checklist:
- Verify CE mark, check for damage or tampering, and ensure proper condition of devices and accessories.
- Only use equipment and chargers supplied by approved supplier or manufacturer.
- Faulty devices should be disposed of according to trust waste management policy.
- Charging should be done in designated areas, not in patient bedrooms.
Report any issues or incidents involving e-cigarettes on the IR1 system under:
- type of incident: security, loss or damage
- cause group: security, theft, loss or damage
- cause: smoking policy breach or concern
14.8.4.6 Risks associated with lithium batteries
- Swallowing: swallowing lithium batteries requires immediate medical attention. risk assessments should be undertaken for any patient who may be at risk of swallowing the battery or vape.
- Malfunction: if a battery overheats, place the device on a dry surface to discharge and contact the manufacturer.
14.9 Appendix I smoking or tobacco use dependency calculator (Fagerstrom test)
Refer to appendix I: smoking or tobacco use dependency calculator (Fagerstrom test) (staff access only).
14.10 Appendix J prohibited products
14.10.1 Heat not burn products
- Heat not burn products use compressed tobacco in a mini-cigarette form in a vaporiser.
- Unlike electronic cigarettes which vaporise nicotine suspended in a liquid, a heat not burn device heats and vaporises actual tobacco, meaning they must be considered as tobacco products.
- Tobacco companies are heavily promoting heat not burn products and see is as their main focus for future growth. The companies are claiming these products are safer than other forms of tobacco and have begun lobbying the UK government that ‘heat not burn’ products should be exempt from the indoor smoking ban and advertising regulations.
- Below are examples of what they look like. If you do get asked by ward staff or patients, they are tobacco products and aren’t allowed on inpatient areas.
14.10.2 Nicotine pouches
- Nicotine pouches are similar to snus pouches as they are made to be placed between the lip and gum, and do not require spitting. Nicotine pouches do not contain fresh tobacco leaf but a form of dehydrated nicotine that does not need to be kept cold. The pouches usually contain plant fibres, flavourings and sweeteners. Nicotine is absorbed into the bloodstream via the mucous membranes in the mouth. Nicotine strengths can range between 4mg and 18mg.
- The UK Independent Scientific Committee on Toxicity (COT) raised concerns around the lack of specific regulations for nicotine pouches in the UK, and the absence of data other than that produced by the tobacco industry. The COT have not yet finalised their recommendations, however their draft report expresses concerns over the current regulatory framework for oral nicotine pouch products, as they did not fall under specific regulations, and have concerns regarding the high levels of nicotine in many commercially available pouches.
- Nicotine Pouches are not currently recommended for use by either National Institute for Health and Care Excellence (NICE) or the National Centre for Smoking Cessation and Training (NCSCT) and are not currently covered in the AWP smoke free and the associated stop smoking medicines guidance.
- For these reasons these products should be stored off ward as a tobacco product.
- Below are examples of nicotine pouches.
Document control
- Version: 8.
- Unique reference number: 32.
- Ratified by: Risk management clinical leadership executive group.
- Date ratified: 6 May 2025.
- Name of originator or author: Interim operations manager for healthy hospitals service.
- Name of responsible individual: Chief nursing officer.
- Date issued: 13 May 2025.
- Review date: 31 May 2028.
- Target audience: All trust colleagues, patients and visitors.
Page last reviewed: June 20, 2025
Next review due: June 20, 2026
Problem with this page?
Please tell us about any problems you have found with this web page.
Report a problem