Contents
- Welcome
- My team
- Cardiac conditions
- Coronary artery disease
- Heart failure
- Valve disease
- Arrhythmia
- Risk factor management
- Smoking
- Weight
- Cholesterol
- High blood pressure
- Stress
- Healthy eating and drinking
- Sexual activity and relationships
- Sleep
- Medication
- Cardiac rehabilitation physiotherapy sessions
- My future
- Further information
Welcome
Cardiac Rehabilitation is a programme designed for people following a cardiac event, operation or diagnosis. Our team aim to support you to return to as full and active a life as possible and give you the confidence to manage your condition long-term. Through integrated working with our specialist cardiac team we provide education, lifestyle advice, counselling and structured physical activity and exercise to aid recovery and reduce the risk of further cardiac episodes.
This booklet provides you with information to support the advice and treatment you will receive from the cardiac rehabilitation team. There are also sections for you to complete and update to help set goals and log your progress. It is important to remember that your condition and recovery are individual to you and therefore your treatment will be tailored to suit your needs. Our team will assess and work alongside you to ensure you get the most out of your programme and achieve your goals.
We look forward to working with you!
My team
Our team is made up of cardiac nurses and specialist physiotherapy staff. Due to a variation in our working hours we may not be able to answer your call immediately however if you leave us a message we will get back to you as soon as possible.
We are based at Cantley Health Centre and can be reached by calling 03000 211518. Please note we do not work weekends or bank holidays so calls of an urgent nature should be directed to your GP, NHS 111 or 999 in emergencies.
You nurse or physiotherapist will provide you with their name and more specific contact details.
Cardiac conditions
If you have been referred to our service you will have a diagnosis of ‘cardiac related illness or disease’. This can relate to different mechanisms within your heart. Common cardiac conditions may affect:
- the coronary arteries, coronary artery disease
- the heart muscle or pumping action, heart failure or valve disease
- the rhythm or pace of the heart, arrhythmia
It may be that you are affected by more than one of these conditions. We will discuss your specific condition and management with you and answer any questions you may have.
Coronary artery disease
Heart attack
The heart is a hollow organ which fills with blood when its thick muscular walls relax. When the muscular walls contract it pumps blood around the body through a network of arteries.
The heart itself requires a plentiful supply of blood. This supply is delivered by the coronary arteries which run over its surface. If one of these arteries or a branch of one of these arteries becomes blocked, part of the heart muscle is starved of blood and is damaged. This is known medically as a myocardial infarction or a heart attack.
Over time, the walls of your coronary arteries may have become narrowed by a gradual build up in the artery wall of fatty material, known as atheroma. The area of artery that is narrowed by atheroma may get damaged or inflamed and a small crack appears. When this happens the body fights back by covering the damage with a small clot made up of blood cells called platelets. This clot can block the artery and stop blood flowing through to the muscle and causing a heart attack.
Angina
Angina is a feeling of tightness, discomfort or heaviness in the chest, which may radiate into the neck, jaw, arms and between the shoulder blades. It typically comes on during activity or high emotion. It happens when the coronary arteries cannot supply enough blood to a part of the heart muscle and this is usually due to narrowing of the arteries. It is eased by rest or Glyceryl Trinitrate (GTN) spray or GTN tablets. If you experience angina after a cardiac event, you should know what to do.
Use of GTN for angina
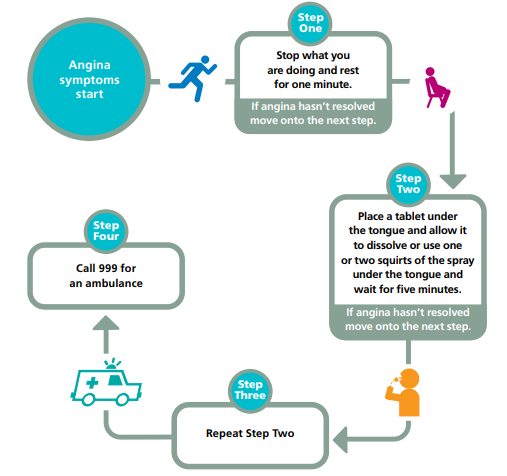
- Angina symptoms start.
- Stop what you are doing and rest for one minute. If angina hasn’t resolved move onto the next step.
- Place a tablet under the tongue and allow it to dissolve or use one or two squirts of the spray under the tongue and wait for five minutes. If angina hasn’t resolved move onto the next step.
- Repeat step 3.
- If repeated step 3 and the symptoms last, call 999 for an ambulance.
Medication, you will be prescribed medication to protect your heart.
Angioplasty, this is when a special catheter is inserted through an artery in your arm or leg and passed up to the blocked vessel in the heart. The tip of the catheter is a small balloon, which is inflated with enough pressure to clear the blocked artery. A stent may also be put into the artery to hold the artery open. Eventually the stent becomes embedded in the lining of the artery, helping to prevent it from becoming narrowed again in the future.
Thrombolysis, a dose of ‘clot busting’ medication that attempts to dissolve the clot within the artery. Coronary artery bypass graft, you may need an operation where a blood vessel is taken from your leg, arm or chest and used to bypass a narrowed section of coronary artery.
Heart failure
Heart failure means that your heart is not pumping blood around your body as effectively as it should. Having heart failure doesn’t mean that your heart has stopped working, but that your heart needs some support to help it work better. Heart failure can have many causes such as a heart attack, high blood pressure, inherited conditions, viral illness and damaged heart valves.
Symptoms occur due to a build up of fluid in the body which may affect the lungs and cause breathlessness. Fluid retention may also cause swelling from you waist downwards. You may feel tired as your heart struggles to deliver enough blood and oxygen to your muscles.
Heart failure treatment helps to control symptoms and protect the heart muscle leading many people to live full and active lives. Your doctor or cardiac nurse is likely to recommend drugs that will help to improve your symptoms, keep you as well as possible, help prevent your condition from getting worse and help to improve your life expectancy.
Some people with heart failure will benefit from an implantable device which helps to improve the pumping action of your heart. Your doctor will talk to you about these treatments if they are the right option for you.
Valve disease
There are four chambers in your heart and the valves make sure that the blood flows through them in one direction. The two large blood vessels that leave the heart also have valves to make sure that the blood does not go back into the heart once it has been pumped out. A diseased or damaged valve can affect the flow of blood in two ways.
If the valve does not open fully, it will obstruct or restrict the flow of blood. This is called valve stenosis or narrowing. This can put extra strain on your heart, making it pump harder to force the blood past the narrowing.
If the valve does not close properly, it will allow blood to leak backwards. This is called regurgitation or a leaky valve. This can put extra strain on your heart and may mean that your heart has to do extra work to pump the required volume of blood.
Some people will not experience any symptoms with valve disease but typical symptoms include shortness of breath, fatigue and swelling of the feet and ankles.
Certain medications or heart valve surgery can treat the symptoms of valve disease. Your treatment will depend on the cause of your problem and the effect that it is having on your heart.
Arrhythmia
An abnormal heart rhythm or arrhythmia means your heart is beating too fast, too slow, or with in an irregular pattern. Your heart has an electrical system that tells it when to beat and pump blood around your body. If there is a problem with this system you may experience an abnormal heart rhythm.
The symptoms of an abnormal heart rhythm depend on what type of arrhythmia you have. The most common symptoms of an abnormal heart rhythm include palpitations (a thumping or fluttering sensation in your chest), dizziness, breathlessness, feeling tired, and losing consciousness.
There are many different types of abnormal heart rhythm. What type you have depends on where in your heart the electrical impulse starts, and if it causes your heart to beat too fast, or too slowly. The most common abnormal rhythm is atrial fibrillation (an irregular or fast heart rhythm).
Depending on the type of abnormal heart rhythm you may have been started on medication to stop, prevent or control it. If appropriate, they might suggest a procedure such as cardioversion or catheter ablation, or surgery to insert an implantable cardioverter defibrillator (ICD) or pacemaker.
If you have been diagnosed with an arrhythmia and want further advice or information then speak to your Cardiac Rehabilitation team.
Risk factor management
There are many factors which can influence somebody’s chance of developing heart disease or having a heart attack. Some of the risk factors such as family history, gender, age and cultural background cannot be changed. There are however some risk factors that can be modified to reduce a person’s risk. This section highlights some of the modifiable risk factors associated with heart disease and how you can try and manage them.
Smoking
Stopping smoking is the single best thing you can do for your heart health as it is one of the main risk factors causing heart disease. Smokers are almost twice as likely to have a heart attack compared with people who have never smoked. Stopping smoking has huge benefits and it’s never too late to give up.
- Smoking damages the lining of your arteries, leading to a build-up of fatty material which narrows the artery. This can cause angina, a heart attack or a stroke.
- The carbon monoxide in tobacco smoke reduces the amount of oxygen in your blood. This means your heart has to pump harder to supply the body with the oxygen it needs.
- The nicotine in cigarettes stimulates your body to produce adrenaline, which makes your heart beat faster and raises your blood pressure, making your heart work harder.
- Your blood is more likely to clot, which increases your risk of having a heart attack or stroke.
It can be difficult to quit smoking and it is vital that you get the right support to help you make the right changes and stick to them. If you want to quit smoking but don’t know where to start you can speak to your Cardiac Rehabilitation team or your GP who can give advice on practical tips, support groups, nicotine replacement products or medication.
By quitting you’ll be improving your own health by dramatically reducing your risk of coronary heart disease, stroke and a variety of cancers. You’ll feel better, and have more money to spend on other things that you enjoy.
You can contact the Yorkshire SmokeFree service for FREE expert advice (face to face, telephone or online) and FREE stop smoking medication to help you quit! Call 0800 612 0011 (free from landlines), 0330 660 1166 (free from most mobiles) or visit the Yorkshire Smoke free service website (opens in new window) to get the right support for you.
Weight
If you are overweight you are more at risk of developing heart disease, high blood pressure and diabetes. It is therefore important to maintain a healthy body weight. Your diet and physical activity levels will impact upon your weight and will be discussed later on in the booklet. If you are planning on losing weight then speak to your GP or Cardiac Rehabilitation team to support and advise you.
Cholesterol
Cholesterol is a fatty substance found in everyone’s blood. Too much cholesterol leads to fatty deposits in the blood vessels, which then become narrowed or blocked. Most cholesterol is made from fat in the food we eat and so a low fat diet can reduce blood cholesterol levels. Triglycerides are another type of fat found in the blood. Raised triglyceride levels can increase your risk of heart disease. Being overweight or inactive, drinking too much alcohol and eating too many sugary foods can all raise your levels of triglycerides and is discussed in the ‘Healthy Eating’ section of the booklet. You may be on medication to reduce your cholesterol levels
High blood pressure
Hypertension, or high blood pressure, develops when the pressure of the blood running through the vessels is too high. It can occur when the larger blood vessels become more rigid (and less expandable), while the smaller vessels constrict. This puts a strain on the blood vessels, and the heart has to work much harder to keep the blood circulation going. High blood pressure is very often a silent condition which shows no symptoms. Because of the increased strain on your heart and blood vessels, untreated hypertension puts you at risk of angina or a heart attack.
Your GP and Cardiac Rehabilitation team will monitor your blood pressure and start or alter blood pressure medication accordingly. You may find that this medication has some unpleasant side effects and you should discuss this at your appointments to see if there may be an alternative.
Simple lifestyle changes like quitting smoking, exercise, weight loss and diet will have an impact on your blood pressure and improve your overall health.
Stress
Stress is a word people often use to describe how you may feel when everything seems too much. Suffering a cardiac event or being diagnosed with a cardiac condition can cause stress and anxiety to build up.
You might start feeling stressed when you feel you have too much to do, or too much on your mind. You may have been feeling overwhelmed for a long time. You may also feel that other people are asking too much from you or that you have to deal with situations that you can’t control or change.
Over a long time, stress can be hard to deal with and bad for your health. If you’ve felt under stress for a while, it may lead to depression or anxiety or more severe mental and physical health problems. If you struggle to cope with stress, you can develop some unhealthy habits. For example, you may eat unhealthy food as a form of comfort or smoke or drink alcohol to help you deal with how you feel. Some of these habits can increase your chance of developing heart disease.
If you feel that you are experiencing stress that is affecting your health and wellbeing then speak to your GP or Cardiac Rehabilitation Team who can look at ways to help you. Try to work out the triggers for stress and if there are any simple changes you can make to reduce your stress levels. As part of our physiotherapy programme we deliver relaxation sessions which are a good way of taking some time out and reducing stress levels.
We can provide relaxation CDs for you to use at home and encourage regular use of relaxation. We also run Tai Chi Style sessions which again encourage relaxation. If you wish to discuss this further then please talk to your Cardiac Rehabilitation Team.
The Improving Access to Psychological Therapy team are a service set up to support people with long-term conditions with their mental health and wellbeing. The service is free and you can self-refer to access a range of talking therapies, information and self-help literature. To self-refer into the service telephone 0800 8048999 or for all other enquiries call 03000 211563.
Healthy eating and drinking
Your diet can strongly affect the health of your heart. Eating healthily is one way in which you can reduce the risk of further heart disease and help you control your weight, blood pressure and blood cholesterol.
For most people, the move towards a healthy, balanced diet means eating more fruit, vegetables and fish. The most important thing is to aim to have a varied diet. Here are some simple changes you can make to your diet:
Eat more fibre and starchy foods
- Soluble fibre is found in oats, pulse and vegetables and can help to lower cholesterol levels. Insoluble fibre found in wholemeal bread, pasta, rice and wholegrain cereal help fill you up and prevent constipation
- Try and opt for wholegrain or multigrain foods
- Aim for at least 5 portions of fruit and vegetables daily
- Leave the skins on potatoes
- Choose high fibre cereal for breakfast such as bran flakes, porridge, Weetabix or shredded wheat
- Add peas, beans and lentils to soups, stews and casseroles.
Eat less fat
- As fat is high in calories you should try to limit all types of fat in your diet.
- Avoid frying food in favour of grilling, baking, steaming or poaching.
- Remove skin from poultry and cut off any visible fat on meat, choose leaner cuts of meat or swap for fish.
- Have low fat dairy products, for example skimmed milk, semi skimmed milk, half-fat cheese.
- Choose an olive oil based spread and olive products or rapeseed oil for cooking.
- Reduce intake of crisps, pastries, pies, cakes etc.
It is important to remember that all fat is high in calories so you should try and limit total fat content within your diet. You may have heard of ‘good fats’ and ‘bad fats’ which can be confusing. The type of fat you eat can affect the level of cholesterol in the blood. Saturated fat increases your blood cholesterol whereas unsaturated fats have a role in lowering your risk of heart disease so should be used in its place. Try to cook with rapeseed or olive oil but still use as little as possible to lower your calorie intake.
- Saturated fat is found in animal products such as butter, cream, lard, cheese, meat, pies and pastry.
- Unsaturated fats include polyunsaturated fats found in sunflower oil, corn oil, soya oil and oily fish and monounsaturated fat found in olive oil and rapeseed oil.
Reduce sugar intake
- Reducing your sugar intake is one of the easiest ways to lose weight but sugar can be hiding in seemingly ‘healthy’ products so ensure you check the nutritional information.
- Avoid adding sugar to tea and coffee (use artificial sweeteners if needed).
- Choose sugar free drinks and squashes.
- Cut down on puddings, cakes, pastries, sweets, chocolate and jams.
- Avoid sugar coated cereals and check the label for sugar content.
Reduce salt intake
- Too much salt can increase blood pressure so should be limited. Many foods contain salt and therefore try to avoid adding salt to meals when cooking or at the table. Use herbs, pepper and spices to flavour your food.
- Cut down on salty snacks like crisps and salted nuts.
- Reduce your intake of processed food such as ready meals and takeaways which are high in salt.
- Tinned or processed meat such as bacon, sausages or tinned ham contain medium salt levels so should be reduced where possible.
Reduce alcohol intake
- All alcoholic drinks are high in calories. A small amount of alcohol is not harmful but too much can lead to weight gain, overeating ad raised blood pressure.
- The recommended amount of alcohol consumption is no more than 2 units per day.
- Try to have at least a couple of days a week without any alcohol.
- 1 unit of alcohol equals half a pint of beer (normal strength), a single pub measure of spirits (25ml). A small glass of wine (125mls) is around 1.5 units of alcohol depending on strength.
Healthy eating does not necessarily mean changing your diet all at once. Try changing one thing at a time and make sustainable changes. It is important to enjoy your food
Sexual activity and relationships
Whether you have angina or are recovering from a heart attack or heart surgery you can usually resume sexual activity when you are feeling better. After a heart attack or surgery, this is normally within four to six weeks. There are lots of things that you can do to reduce your anxiety about sex, such as choosing a relaxing atmosphere , caressing and touching may be a helpful start to increase your confidence and keeping the room and bed at a comfortable temperature.
When you are ready to start having sex again, think about the following:
- avoid having sex after a heavy meal or too much alcohol.
- find a comfortable position
- ask your partner to take a more active role
- if you have a GTN spray or tablets, keep them where you can reach them just in case you need them.
A loss of sex drive or impotence is a common problem and usually temporary so try not to worry. The emotional stress of your condition or the medicines you have been prescribed could be the cause of your problems. Having diabetes can also affect your sex drive.
You should not feel embarrassed to talk to your GP, practice nurse or Cardiac Rehabilitation team nurse will be understanding and can offer you advice and support.
Sleep
Sleep is important for your health and wellbeing. After a stressful life event such as a cardiac diagnosis, the introduction of new medication and changes to your routine, you may find that you experience difficulty sleeping. Here are some tips to encourage a good night’s sleep;
Try to go to bed at a regular time and have a bedtime routine that helps you relax such as reading, listening to music or having a bath. Ensure your bedroom is comfortable environment which is not too hot, cold or noisy.
Try to be active in the day and exercise regularly as advised by your cardiac rehabilitation team.
If you are worrying or have been awake for over 30 minutes, get up and do a relaxing activity until you feel tired again. Try not to worry.
Consider whether your medication may be affecting your sleep and speak to your nurse or doctor if you believe they are. Medication can be used to aid sleep although can have side effects so it is worth trying other methods before talking to you doctor about this.
Try not to nap in the day or sleep in late as this may affect your routine.
Avoid caffeine, heavy meals, alcohol or excessive amount of fluids prior to going to sleep.
We can provide more information on a good night’s sleep as well as relaxation exercises if you feel this would be beneficial.
Medication
This section aims to give you some information on common medication used in cardiac conditions. The medication you are prescribed will be personal to you, your cardiac condition and other factors such as any other illnesses or risk factors. As with most medications there can be side effects associated therefore read the information provided and be aware. Never stop or reduce medication without speaking to a healthcare professional. You can speak to your cardiac rehabilitation nurses, pharmacist, consultant or GP if you have any specific questions about your medication.
Anti-platelet medications
These ‘blood thinning’ drugs include Aspirin, Ticagrelor, Clopidogrel and Prasugrel. With the exception of Aspirin, these medications may be referred to as ‘stent protectors. These medications can cause you to bleed for longer after minor cuts due to your blood’s impaired ability to clot.
Aspirin
Aspirin works by reducing the stickiness of blood cells called platelets. This helps to prevent the formation of blood clots in the blood vessels of your heart. Blood clots can block the blood flow to your heart muscle, causing a heart attack. You may get indigestion (heart burn). Taking your Aspirin with or after food will help to reduce this. If you get indigestion, let your doctor know. The protective effect of aspirin only works at a low dose. If you need to take a pain killer, try an alternative such as Paracetamol.
Ticagrelor
Ticagrelor works by reducing the stickiness of blood cells called platelets. This helps to prevent the formation of blood clots in the blood vessels of the heart. Ticagrelor is used, together with aspirin after a heart attack or if you have had angioplasty or stents to the blood vessels in the heart. Ticagrelor is usually taken for up to 12 months however your consultant will let you know exactly how long to take Ticagrelor for.
Shortness of breath might be due to your heart condition but may be a side effect of Ticagrelor. Tell your Consultant, GP or cardiac nurse.
Clopidogrel
Clopidogrel works by reducing the stickiness of blood cells called platelets. This helps to prevent the formation of blood clots in the blood vessels of your heart. If you are allergic to Aspirin, Clopidogrel can be used instead. It is sometimes used together with aspirin after a heart attack, or if you have had angioplasty or stents to the blood vessels in the heart.
Prasugrel
Prasugrel works by reducing the stickiness of blood cells called platelets. This helps to prevent the formation of blood clots in the blood vessels of your heart. It is used, together with Aspirin, after a heart attack or an angioplasty or stents. It can also be used in diabetic patients who have an angioplasty. If you develop a blood clot while already taking Clopidogrel, Prasugrel may be used instead. Check with the doctor at the hospital to make sure that you know how long you should continue to take Prasugrel.
In some cases bleeding can occur in the stomach or bowel when taking antiplatelet medication. This happens very rarely, but can become serious, requiring immediate emergency treatment. Should you notice bleeding from your back passage, pass black tar like stools, or have blood stained vomit contact the emergency doctor or visit the accident and emergency department.
Cholesterol lowering drugs
These drugs reduce the amount of cholesterol in your blood by reducing the way in which your body makes cholesterol. Cholesterol is a fat that can clog the blood vessels and reduce the blood flow to your heart muscle. Cholesterol lowering drugs are used to reduce the cholesterol level after a heart attack, and in heart disease. Avoid drinking grapefruit juice whilst taking a statin, since this can increase the chance of side effects. Cholesterol lowering drugs include statins (Simvastatin Atorvastatin, Pravastatin, Rosuvastatin) and Bezafibrate or Ezetimibe.
Mild side effects may include constipation or diarrhoea, flatulence (wind), feeling sick, headaches. Rarely people can get muscle pain, tenderness or weakness, or liver problems. Report any of these side effects to your doctor.
Statins work best if they are taken before you sleep as your body produces most of its cholesterol during sleep. Cholesterol lowering drugs work together with the diet to reduce cholesterol. You need to continue to follow a healthy diet whilst taking these drugs.
Angiotensin converting enzyme (ACE) inhibitors
ACE inhibitors help to strengthen the heart muscle. They also stop the body from holding onto excess fluid which reduces the strain on the heart muscle. ACE inhibitors are used after a heart attack to strengthen the heart muscle and allow the heart to pump more efficiently. They are also used to treat high blood pressure and heart failure and kidney impairment. These drugs include Ramipril, Lisinopril, Enalapril, Perindopril, Captopril. ACE inhibitors are started at a low dose to reduce side effects and are then usually increased to improve your treatment.
Beta blockers
Beta blockers, such as Bisoprolol, Atenolol, Metoprolol, Carvedilol and Sotalol, lower the blood pressure and slow the heart to give a steadier beat. They also ‘dampen down’ the effects of exercise and stress on the heart. They are used to reduce the risk of another heart attack. They can also be used to prevent angina, treat high blood pressure, abnormal heart beats and heart failure.
Nitrates
Nitrates work by widening the blood vessels allowing more blood and oxygen to get to the heart muscle. Examples of nitrates are Glyceryl Trinitrate (GTN) and Isosorbide Mononitrate. Nitrates are mainly used to prevent and treat angina. The GTN protocol is highlighted in the ‘Angina’ Section of this booklet.
Calcium channel blockers
Common calcium channel blockers include Nifedipine, Amlodipine, Diltiazem, Verapamil and Felodipine. In angina they work by widening the blood vessels and allowing more blood and oxygen to get to the heart muscle. Some drugs in this group (Verapamil and Diltiazem) control the heart or pulse rate. This effect reduces the work load on the heart. These drugs are used to treat angina, sometimes with other drugs. They may also be used to treat high blood pressure and irregular heart rates.
Nicorandil
Nicorandil works by widening the blood vessels, allowing more blood and oxygen to get to the heart muscle and is used to treat angina.
Angiotensin II receptor antagonists (ARB’s)
These drugs strengthen the heart muscle and help the heart to pump more efficiently. They are used to treat high blood pressure and may also be used for heart failure, and after a heart attack if you are not able to take an ACE inhibitor. Examples of ARB’s are Candesartan, Valsartan, Losartan and Irbesartan. Side effects may include dizziness, skin rashes and itching.
Diuretics
These drugs are often known as ‘water tablets’ and remove excess fluid within the body via the kidneys. As a result the heart has less work to do. Diuretic medications include Furosemide, Bumetanide, Amiloride, Chlortalidone, Bendroflumethiazide and Spironolactone. They can be used to treat high blood pressure and to remove excess fluid. Side effects may include gout, fatigue and muscle cramping and stomach upset.
Anti-arrhythmic drugs
These drugs work differently but each of them affects how fast and regularly the heart beats. Examples of anti-arrhythmics include Digoxin and Amiodarone. Arrhythmias are irregular rates or rhythms of the heart. Anti-arrhythmic drugs are used to control heart rate and rhythm.
Thrombolytic agents
Only a very small percentage of patients now require this drug. It is only given in hospital. Thrombolytic drugs (such as Reteplase) dissolve the clot which has blocked an artery and caused a heart attack which is why it is often referred to as a ‘clot buster’. The aim is to give thrombolytic agents as soon as possible after the onset of symptoms of a heart attack to reduce the damage caused to the heart muscle. This type of drug is not suitable for everybody.
Anticoagulants
Anticoagulant medicines prevent blood clots from forming. They are sometimes called blood thinners, but they do not actually thin the blood. Instead they increase the time it takes for your blood to form a clot.
There are two main types of anticoagulants. Warfarin is currently the most commonly prescribed anticoagulant in the UK today and NOACs (which stands for ‘new oral anticoagulants’) and includes Dabigatran, Rivaroxaban and Apixaban.
Which anticoagulant you are given depends upon the condition it is treating, other medical conditions you may have, and what you and your doctor agree is best for you. The most common reasons for being on anticoagulation medication include arrhythmia, mechanical valve replacement and other clotting risk factors.
The main side effect of taking any anticoagulant medicines is bleeding. It may cause internal bleeding, or make bleeding from a minor injury worse. Speak to your GP or cardiac nurse if you experience cuts which bleed for longer than usual, bleeding that does not stop by itself, excessive nose bleeds, bleeding gums, severe bruising, blood in urine or bowel movement.
If you suffer a head injury, such as falling and hitting your head, or experience a blow to the head, seek medical help without delay to rule out internal bleeding which may not be immediately obvious.
The BORG scale
While exercising we ask you to use the ‘BORG scale’ to rate how strenuous an activity feels to you. When rating your perceived exertion try to consider how much effort the activity required and how much breathlessness and fatigue you are experiencing.
| Rating | Effort | Description |
|---|---|---|
| 0 | Nothing at all | Little or no effort |
| 0.3 | Nothing at all | Little or no effort |
| 0.5 | Nothing at all | Little or no effort |
| 0.7 | Light | Little or no effort |
| 1.0 | Light | Little or no effort |
| 2.0 | Light | Little or no effort |
| 3.0 | Moderate | Training range, how you should feel exercise or activity |
| 4.0 | Moderate | Training range, how you should feel exercise or activity |
| 5.0 | Moderate | Training range, how you should feel exercise or activity |
| 6.0 | Strong | To be avoided during training |
| 7.0 | Strong | To be avoided during training |
| 8.0 | Very strong | To be avoided during training |
| 9.0 | Extremely strong | Maximal |
| 10.0 | Extremely strong | Maximal |
Please note to exercise safely and effectively we ask you to work at a level 3-5 on the BORG scale. It may take you a few sessions to get used to using the BORG scale so please ask if you have any questions or are unsure.
Cardiac rehabilitation physiotherapy sessions
Our team are here to work with you to begin or return to physical activity in a safe and effective way following your diagnosis. Whatever your fitness level and experience in exercising we can offer you advice and a programme to suit you. We run exercise groups aimed at all levels of fitness, one to one gym sessions and home based sessions. We also offer Tai Chi style exercises and outdoor walking programmes. It may be that you don’t feel able to commit to regular sessions but we are still happy to offer advice on how to independently progress with your physical activity needs in a safe way. Sessions are held at venues around Doncaster to try and make us as accessible as possible;
Venues:
- The Dome (DN4 7PD)
- Armthorpe Leisure Centre (DN3 2BZ)
- Thorne Leisure Centre (DN8 5HX)
- The Fitness Village at Balby Retail Park (DN4 8EE)
- Dearne Valley Leisure Centre (S64 0LB)
- Adwick Leisure Centre (DN6 7QF)
- St Johns Information Centre (DN4 8JS)
Regardless of your previous fitness level we recognise that starting to exercise following a cardiac diagnosis can be daunting which is why we complete a comprehensive assessment to establish your needs and goals and determine an approach that works for you. On your assessment we will discuss your current diagnosis, treatment, symptoms and level of fitness as well as monitoring your blood pressure and heartrate. From here we will offer you the options available and you can choose a programme of care that you feel comfortable with. If you have any questions about the service or returning to physical activity and exercise then please discuss with a member of the cardiac rehabilitation team.
The ‘log book’ within this booklet is designed to help you keep a record as you build up your exercise levels and activities. This allows you to track your progress and help you work towards your goals.
Consideration for your physiotherapy assessment and treatment sessions; Bring this booklet along with you so we can help complete your ‘log book’. Inform the team if you have had any shortness of breath, illness, injury or changes to your medication since they last saw you. Bring your GTN with you if you have one. If you are diabetic we advise you monitor your blood sugar and keep a small snack with you. Avoid large meals and alcohol before exercising. Wear comfortable clothing that is not restrictive and rubber soled shoes that are appropriate for exercise. Jeans are not permitted in the gym area. Water will be provided but feel free to bring a drink. Use the BORG scale (as above) to monitor how hard you are working.
Education sessions; As part of the group sessions we run an education programme which cover topics such as exercise, healthy eating, medication, cardiac anatomy and conditions, stress management and relaxation, emotional support and wellbeing, smoking and alcohol advice, basic life support, sleep, sex and relationships and Tai Chi style exercise. We value your input and experiences in these sessions and encourage you to join in and ask questions. Our education programme aims to improve your knowledge and awareness of your condition and to give you the confidence to manage it.
My future
We hope you have found this information booklet useful. Before you are discharged we will review your condition, functional ability and goals to ensure you have achieved or are on the way to achieving what you have set out to. Hopefully you will now feel you have the tools to independently manage your condition and maintain healthy lifestyle changes. We wish you all the best for the future!
This booklet was produced by Stephanie Blythe, RDaSH Lead for Cardiac Rehabilitation and specialist physiotherapist using a range of sources as shown below
Further information
With special thanks to:
- the British Heart Foundation, NHS Choices, NICE, Sheffield Teaching Hospitals NHS Foundation Trust
These organisations provide a range of online publications which offer further information on the topics discussed in this booklet. Please ask a member of our team if you require any help or advice.
Document control
- DP number: DP8293/06.22.
Page last reviewed: April 30, 2024
Next review due: April 30, 2025