Contents
1 Introduction
Children and young people who did not attend appointments (DNA) have often been considered in the same way as an adult DNA. In the recognition that children and young people differ from adults in that they do not take responsibility for their own health needs it is important to consider children as was not brought (WNB) as opposed to did not attend.
It is recognised that adolescents can have the capacity to make decisions about elements of their health care and may be in a position to make their own judgements around whether or not they attend appointments and may attend these appointments alone (consideration should be given to whether financial costs of attending appointments and other factors such as school bus times affect their ability to attend).
Key principles:
- children and young people have a right to receive appropriate healthcare and it is the responsibility of parents to access this on their behalf
- it is the responsibility of professionals to work effectively to engage with parents, carers, children and young people
- effective intervention is significantly influenced by the quality of engagement that the child or young person and their parents or carer has with the professional
- there should be a clear purpose to engagement which is clearly discussed with the child or young people and their family
- there should be collaborative working between the health practitioner and family
- feedback to a child and their parent or carer is an important part of the engagement process, this should include a review of their care plan and goals to inform any further support needs
- it is important for health professionals to seek to understand why parents or carers do not bring their child for an appointment, in order to address any barriers that there may be to them attending
There are many valid reasons for parents or carers not bringing their child to an appointment such as transport difficulties, forgetfulness, or the perception that an appointment is no longer required. It is recognised from research that non engagement or disengagement from services is a strong feature in domestic abuse, neglect and abuse of children and young people. Repeated cancellations and non-attendance may be as a result of disguised compliance. Health professionals will need to adopt respectful uncertainty in respect of reasons given for children not being brought to appointments.
Family situations should be considered individually and a flexible approach is required to support engagement. In considering the health risk to children and young people and any other risks such as parental factors a response should be proportionate.
The trust delivers services for children with a range of physical and mental health needs and as such the impact for that child and their dependent children or siblings from related non engagement must be considered.
It is recognised that this policy may appear to be predominantly applicable to children under 16 years; however, the principles must equally apply to those aged 16 to 18 years. Often children aged 16 to 18 years will make personal decisions about their health and care needs. Recording their wishes and exploring ways to engage this group of young people is critical to manage the risks associated with them.
Whilst any transition from one clinical service to another has the potential for patient or service user disengagement, nationally transitions from children and young people’s mental health services to adult mental health services have been the focus of numerous research studies; all have identified numerous difficulties, specifically around patient or service user experience, disengagement, thresholds for acceptance and long delays in completing transition. Joint working between the services has also been identified as an obstacle.
All the children’s care group staff to whom this policy applies should be aware of the extra potential of disengagement during any transitioning to other services and provide support as required during this time on an individual basis.
2 Purpose
The purpose of this policy is to set out the trust arrangements for, and the approach to the management of children and young people (and their families) who were not brought to or do not attend appointments or disengage from services.
The importance of attending appointments and engaging with the service should be discussed with the child, young person, parent, carer and legal guardian. Failure to attend appointments and or engage with a service and how this will be managed should be discussed early in the care process.
2.1 Definitions
| Acronym | Long form |
|---|---|
| Did not attend (DNA) | Did not attend a planned appointment without cancellation or non-return of consent |
| Was not brought (WNB) | The parent and carer did not bring their child to a planned appointment |
| No access visits (NAV) | Not available at home to be seen for a planned appointment |
| Unseen child | Any practitioner should consider a child unseen if they become aware that primary health care is not being delivered to that child either in the home or community setting |
| Disengagement | Disengagement is when a child and young person or parent and carer does not respond to requests from health professionals |
| Opting out of health visiting service | Managing families who wish to opt out of the health visiting service. |
| CAMHS | Child and adolescent mental health services |
Behaviours of disengagement are usually cumulative and may include:
- disregarding avoidant of health appointments
- not attending health appointment without explanation or with explanations which indicate that for whatever the reason the parent is not prioritising the appointment
- avoiding telephone calls by professionals
- not completing health questionnaires or consent forms
- not having a general practitioner (GP)
- not being home for professional visits
- not allowing professionals into the home
- agreeing to take action; but never do it
- hostile behaviour towards professionals
- manipulative behaviour resulting in no health care
- actively avoiding contact with professionals
There may be reasons why a family choose to disengage from the service:
- wanting to opt out of the service
- poor past experiences of health professionals
- fear of authority figures
- lack of understanding about the need for health intervention
- cultural differences
- fear of being judged
- family wanting to maintain their privacy
- trying to hide something
- lack of understanding about a health condition or issue
- act of omission, for example, neglect, not seeking medical attention or not taking the child to an appointment
- families engaged in other activities, for example, criminal activity
3 Scope
This policy applies to those patients and service users who have not yet reached their 18th birthday and are therefore defined as children and young people (Children Act 1989 and working together 2018), and covers both:
- children and young people who have been referred to trust services (as defined in the scope of the policy) but whose needs and level of risk have yet to be assessed, (covered in part 5 of this policy)
- children and young people that are entitled to receive universal services where routine contacts are scheduled
- children and young people who have been accepted by trust services, and whose level of assessed risk is known. (covered in section 5 and flowchart 1 of this policy)
Whilst it is recognised that this policy will predominantly apply to services specifically targeted for children and young people; the principles will apply to all services delivered by the trust for patients or service users who are, according to the Children Act, defined as children.
Adherence to this policy is the responsibility of all staff employed by the trust, including agency, locum and bank staff contracted by the trust.
4 Responsibilities, accountabilities and duties
4.1 The board of directors
The chief executive is accountable for this policy, and delegates lead strategic responsibility to a director.
4.2 Director for nursing
As nominated strategic lead, the director of nursing is responsible for:
- the implementation of all policies and procedures which are in place to meet the needs of patients
- monitoring adherences to this and other related policies care coordinator, key worker, allocated worker and caseload holder are responsible for:
- following the appropriate steps in this policy and updating the team manager or deputy where necessary
- reporting any breaches in relation to this policy
4.3 Care group directors
Care group directors are responsible for:
- the ongoing review of the policy to keep it up to date with current best practice.
- providing reports to the operational management group (OMG) on any issues associated with the implementation of the policy
4.4 Service manager
The service manager is responsible for:
- making their staff aware of the contents of this policy
- monitoring the compliance of their staff with the contents of this policy
- promoting collaborative working between services, in order that the needs of the patient remain at the centre of the process
- the implementation of the policy across the specified care groups
- facilitating effective joint working with internal and external partners and stakeholders
- monitoring staff compliance with the relevant mandatory risk management training as set out in the clinical risk assessment and management policy and mandatory risk management training needs analysis matrix
- the development, implementation, and monitoring of effective systems of supervision for clinical staff within their care group
4.5 Team leader or team manager
The team leader or team manager are responsible for:
- supporting staff with the implementation of this policy
- reporting any breaches in relation to this policy
- facilitating multidisciplinary team (MDT) discussion to assist decision making and communication of concern and actions
- in the case of looked after children or other children or young people assessed at risk then it is the team manager and deputy responsibility to arrange timely MDT meetings which include legal guardians. All decision-making is to be documented in the clinical records and communicated to all relevant professionals involved in the case
- reporting any breaches in relation to this policy
4.6 Named Practitioners Safeguarding Children team and safeguarding supervisors
Named Practitioners Safeguarding Children team and safeguarding supervisors are responsible for:
- supporting staff through safeguarding children supervision
- providing appropriate advice and guidance when concerns are raised in respect of children and young people who do not attend appointments, were not brought and disengage or are at risk of disengaging with services
- supporting staff with the implementation of this policy
4.7 Care coordinator, key worker, allocated worker and caseload holder
Care coordinator, key worker, allocated worker and caseload older are responsible for:
- following the appropriate steps in this policy and updating the team manager or deputy where necessary
- reporting any breaches in relation to this policy
4.8 All clinical staff
It is every staff member’s responsibility to alert the care coordinator or key worker if a child or young person has not attended an appointment or it is suspected that they are disengaging from services
5 Procedure and implementation
The information is provided in text format but also in the format of flow chart to enable staff to follow the flowchart and seek further detail from the text.
5.1 Children and young people who are not known to the service and have additional needs (see flowchart 1)
Children and young people referred to, but not yet assessed by trust services:
- if two consecutive appointments are DNA or WNB a letter should be written to the GP informing them of this within 2 working days
If a child or young person misses an appointment without acceptable explanation, the care coordinator or allocated worker must, in the case of a referral which has been accepted as urgent by the service or where there are known or suspected risks (of any kind).
- Attempt contact with the child or young person and or their parent, carer and legal guardian, (within 24 hours), for the purpose of establishing reasons for non-attendance.
Where attempts to contact fail follow steps 1 to 4 listed below:
- ring the GP, any other referrer and all other relevant agencies involved with the child or young person and agree a plan of action
- a team member should attempt, by assertive telephone contact, text and via a home visit, direct contact with the child, young person, parent, carer or legal guardian within 2 working days
- document the plan of action and any contact with the child, young person, parent, carer or legal guardian
- discuss the situation with the team leader or manager
If these actions to secure another appointment have failed the following steps must be taken as directed by the team manager or their nominated deputy:
- discuss with the GP (and any other referrer), all other relevant agencies involved with the child or young person (which may include the child, young person’s school or college). Any discussion should consider all safeguarding and risk issues
- a further appointment should be offered, by phone, text, calling card, or letter, within three working days. This should offer the option of an alternative venue and time most suited to the needs of the child, young person or family concerned, the referrer should be informed
- if the child or young person misses the agreed appointment, any consequent decision to discharge them from the service must only be considered once a discussion(s) with all other agencies involved and the team leader or manager has or have taken place. These discussions must be recorded in clinical records and must consider all issues of risk for which appropriate management plans must be in place and communicated to the referrer
5.1.1 In the case of a non-urgent referral and where there are no known or suspected risks (of any kind)
Follow flow chart 1.
- The child, young person, parent, carer or legal guardian should be contacted by telephone in the first instance or, in the case of there being no response, invited by letter, or text, to contact the service if a further appointment is required. The option of an alternative venue and time most suited to the needs of the child, young person, family concerned should be offered. The letter or text should state that if no contact is made within three weeks, then the child or young person will be discharged from the service.
- If there is no response to the appointment, prior to discharge, the GP or referrer are to be contacted via letter and informed of the proposed discharge and given the opportunity to provide information or contact the family directly.
Routes for the child, young person or family to seek re-referral to the service in the future should also be explained. This letter must be copied to the referrer and or GP.
- If, following a lack of further contact from the child, young person or family, the allocated worker has any concerns about the safety or appropriateness of discharging the child or young person at that point, they must discuss the case with the team leader, the referrer, and any other relevant agencies involved, to decide upon an appropriate course of action. (see appendix a for guidance on risk). The decision making process should be recorded in the care record.
- In any event a decision to discharge a child or young person must be communicated in writing to the GP, any other referrer, and any other relevant agency involved with the child or young person.
- Any action taken and all attempted contacts must be documented in the care record.
5.1.2 Children and young people known to services with additional needs and are suspected to be at risk of disengaging with services
Follow flowchart 1.
If a staff member suspects a child or young person is at risk of disengaging or missing appointments which may impact on their mental health the following action should be taken:
- every child or young person will have an assessment of risk completed and a crisis and contingency plan should form a part of the care planning process
- all those involved in the care of a child or young person have a responsibility to report any break in contact, or a perceived risk of a break in contact to the allocated worker or care coordinator
The allocated worker or care coordinator will decide whether a person is out of contact, based on available assessments and information, professional judgement and discussions with all other agencies involved in the delivery of their care and with a legal responsibility for their care. This decision will be with consideration for the wishes of the child or young person and the assessment of their competency to make informed decisions about their care treatment and risk.
Where the allocated worker, care coordinator or team suspects that a child or young person is out of contact they must:
- make appropriate attempts to contact them or the family. This could include telephone calls, letters, home visit, and discussion with other agencies involved as appropriate
- document their concerns in clinical records and the evidence to support this and any attempts made to contact the child or young person
5.1.3 If the child or young person is suspected to be at risk of disengaging with services and there is no identified risk (flowchart 2)
- The child, young person, parent, carer or legal guardian should be invited by letter to contact the service if a further appointment is required. The option of an alternative venue and time most suited to the needs of the child, young person or family concerned should be offered. The letter should state that if no contact is made within three weeks, then the child or young person will be discharged from the service.
- Routes for the child or young person or family to seek re-referral to the service in the future should also be explained. This letter must be copied to the referrer or GP.
- If, following a lack of further contact from the child, young person or family, the allocated worker has any concerns about the safety or appropriateness of discharging the child or young person at that point, they must discuss the case with the team leader, the referrer, and any other relevant agencies involved, to decide upon an appropriate course of action. (See Appendix 1 for guidance on risk).
- If, following a lack of further contact from the child, young person or family, the allocated worker has any concerns about the safety or appropriateness of discharging the child or young person at that point, they must discuss the case with the team leader, the referrer, and any other relevant agencies involved, to decide upon an appropriate course of action.
- In any event a decision to discharge a child or young person must be communicated in writing to the GP, any other referrer, and any other relevant agency involved with the child or young person.
- Any action taken and all attempted contacts must be documented in clinical records.
5.1.4 In the case of a child or young person with an identified risk
The allocated worker, care coordinator or team manager will:
- attempt contact with the child or young person and or their parent, carer or legal guardian (within 24 hours), with the purpose of establishing reasons for non-attendance disengagement with the service
Flowchart 2, where attempts to contact fail follow steps 1 to 5 listed below:
- urgently review the risk assessment and care plan based on current information and implement the current crisis and contingency plan
- ring the GP, any other referrer, and all other relevant agencies involved with the child or young person advising them they are potentially ‘out of contact’ and discuss what concerns this raises
- a team member should attempt by assertive telephone contact or via a home visit direct contact with the child, young person, parent or carer or legal guardian within 2 working days
- document the plan of action and any contact with the child, young person, parent, carer or legal guardian and other agencies
- discuss the situation with the team leader or manager and agree a plan of action
Having established that the child or young person has disengaged the allocated worker, care coordinator or team manager will:
- inform all those involved in the provision of care for the person that they have disengaged and discuss what concerns this raises and arrange an urgent review meeting with all those involved in the child or young person’s care within 5 working days
The agenda for the review must:
- agree further actions as necessary with time frames for action and review
- agree roles and responsibilities
- consideration of the need for an assessment under the Mental Health Act (MHA) 1983 and 2007
- action to be taken on any relevant safeguarding issues and any action necessary to protect the public
- any consequent decision to discharge the child or young person from the service must only follow discussions with all other agencies involved and the team leader or manager. These discussions must be recorded in clinical records and must consider all issues of risk for which appropriate management plans must be in place and communicated to the referrer and all other agencies or legal guardians involved in the child or young person’s care and where appropriate the child or young person
5.2 Children or young people who are known to services
Flowchart 2, all practitioners should:
- ensure they are appropriately trained in the identification of child safeguarding as this will equip them to make judgements as to whether the child or young person’s health and development is impaired by disengagement with services
- document as per trust policy in relation to any decision making, communications and actions taken
- work in partnership with own and other agencies when families disengage with services
- seek appropriate supervision to aid decision making as required. This could be either through the primary health care meeting or from the named practitioner in the Safeguarding Children team
5.2.1 Managing did not attend (DNA), was not brought (WNB), no access visits (NAV) and disengagement
Flowchart 2:
- after the first DNA, WNB or NAV a contact card or appointment letter (flowchart 2) will be left or sent with a new appointment along with practitioner’s contact details. This second appointment should be as soon as possible but no longer than 14 days from initial contact
- after the second DNA, WNB or NAV a contact card will be left, or a letter sent requesting the service user to contact the practitioner. The practitioner will carry out checks with members of the Primary Healthcare team and multiagency colleagues for an up to date address and contact details and any known difficulties regarding literacy, language or communication. If the patient or service user has not responded within 7 days the practitioner will liaise with relevant professionals or family members who may have had contact with the child and family, for example, midwife, GP, education. If any concerns are identified the practitioner will follow local safeguarding children policy and procedures (see section 9). See flow chart 3 for process
- if there is no response from patient or service user or family and there are no child health and welfare concerns identified the patient or service user should be informed in writing (flowchart 3) that no further visits or appointments will be sent until the next routine review as per the integrated health team core offer
5.2.2 Managing families who wish to opt out of the health visiting service
Follow flow chart 2. The child will remain on the caseload.
5.3 Transient families
Read the below in line with flow charts and refer to those.
5.3.1 Definition of a transient family
A transient family is a family who moves often from one geographical area to another and subsequently has changes of health professionals in the different localities. The children within these families may include children for whom there are believed to be safeguarding concerns. The family’s movement from place to place may have a detrimental effect on the child’s health and wellbeing.
The frequent movement of the family may in some cases be associated with a deliberate attempt to evade the authorities or intent to impede child protection procedures. Families falling within this category require practitioners to maintain close contact.
Families and children who have 3 changes of address or School within a 12-month period are referred to as transient.
5.3.2 Recognition of the transient family
Some families are readily identifiable by their continual movement either across the country or within a particular locality and this may be indicated in their health or education records.
Other factors may also be apparent that indicate transience within a family such as:
- failure to respond to professional enquiries and correspondence
- family where no single agency has a complete picture of the family’s circumstances or information is fragmented across all agencies
- where a family only has temporary registration or has no registration with a general practitioner
- history of missed significant health appointments and or assessments either DNA or WNB
- constant change of health professional within the team that is directly involved
5.3.3. Action to be taken by trust staff
It is the responsibility of trust staff to:
- put an alert on the records (via SystmOne) that the family is transient. The alert should be set to high priority so that all practitioners would be able to see this
- check to see if there are any safeguarding concerns (review records, contact other agencies involved, contact social care) and if there is, follow the relevant safeguarding procedures
- contact early help to ascertain if there is any early help involvement with the family
- if there is early help involvement contact should be made with the lead practitioner
- notify the lead practitioner of any concerns they may have in respect of identified risks, or changes to the family’s social circumstances
- discuss the management of the family at safeguarding supervision
- notify trust safeguarding team that child is missing
5.3.4 Action for health visitors and school nurses
- Staff working within the health visiting and school nursing teams will inform the named health visitor or school nurse of their concerns that the family is transient.
- The school nurse or health visitor responsible for the family’s care at their last known address will remain the named professional until a new address is known. Once the new address is known, responsibility will then be transferred over to the relevant area and team or transferred out of area. The health visitor or school nurse will liaise verbally to inform the relevant professional that the family are transient and therefore at risk, ensuring records are passed on appropriately through child health. If making verbal contact is challenging then it would be good practice to send written information, however this does not negate the need to contact verbally.
- The family will be discussed with other members of the Health team at the team meeting.
- A named health visitor or school nurse is to be allocated who will maintain responsibility for the family while ever they are transient and remain in the locality. This health visitor or school nurse will also be responsible for passing over any information or records if the family relocate outside the area.
- The allocated health visitor or school nurse is to notify general practice services so that they can also put an alert on their system and consider if they have any concerns relating to the family.
5.3.5 Action to be taken if the transient family move away from the area
In the event that the transient family move during an episode of care trust staff are to report this to social care. Refer to Flow charts 1 and 2 and consider flowchart 3.
6 Training implications
Mandatory safeguarding children training and awareness is in place to assist practitioners to recognise the risks and vulnerabilities of children or young people who are not brought or don’t attend appointments or disengage with services.
To support both managers and individual staff and volunteers in identifying the level of training they require, a training matrix is available on the trust site and within the trust training plan.
It is the responsibility of the relevant senior managers or lead clinicians in each directorate to make staff aware of the policy and its contents by:
Covering the policy contents during the local induction of any new staff.
Making staff aware of the policy and its contents at staff or team meetings.
7 Monitoring arrangements
7.1 The number of children and young people who do not attend or disengage from services
- How: Audit of the electronic care record system and comparison with national and regional data.
- Who by: Team manager.
- Reported to: Children care group.
- Frequency: Annual.
7.2 Number of serious incidents involving children and young people who do not attend or disengage from services
- How: Investigation of any reported serious incident Investigation is to include scrutiny of compliance with the requirements of this policy.
- Who by: Team manager in conjunction with the care coordinator, and trust patient safety lead.
- Reported to: The children’s care group and the trust health and safety committee.
- Frequency: As and when an incident occurs.
8 Equality impact assessment screening
To access the equality impact assessment for this policy, please email rdash.equalityanddiversity@nhs.net to request the document.
8.1 Privacy, dignity and respect
The NHS Constitution states that all patients should feel that their privacy and dignity are respected while they are in hospital. High Quality Care for All (2008), Lord Darzi’s review of the NHS, identifies the need to organise care around the individual, ‘not just clinically but in terms of dignity and respect’.
Consequently, the trust is required to articulate its intent to deliver care with privacy and dignity that treats all service users with respect. Therefore, all procedural documents will be considered, if relevant, to reflect the requirement to treat everyone with privacy, dignity, and respect, (when appropriate this should also include how same sex accommodation is provided).
8.1.1 Indicate how this will be met
No issues have been identified in relation to this policy.
8.2 Mental capacity act
Central to any aspect of care delivered to adults and young people aged 16 years or over will be the consideration of the individual’s capacity to participate in the decision-making process. Consequently, no intervention should be carried out without either the individual’s informed consent, or the powers included in a legal framework, or by order of the court.
Therefore, the trust is required to make sure that all colleagues working with individuals who use our service are familiar with the provisions within the Mental Capacity Act (2005). For this reason, all procedural documents will be considered, if relevant to reflect the provisions of the Mental Capacity Act (2005)to ensure that the rights of individual are protected, and they are supported to make their own decisions where possible and that any decisions made on their behalf when they lack capacity are made in their best interests and least restrictive of their rights and freedoms.
8.2.1 Indicate how this will be achieved
All individuals involved in the implementation of this policy should do so in accordance with the guiding principles of the Mental Capacity Act 2005 (section 1).
9 Associated documents
- Disengagement policy
- Safeguarding children manual
- Healthcare record keeping policy
- Transition, child adolescent mental health services (CAMHS) to adult mental health and learning disability services policy
- Clinical risk assessment and management policy
To be read in conjunction with the local safeguarding children board (LSCB) multiagency procedures in the geographical areas in which the Trust provides services:
- Doncaster LSCB procedures (opens in new window)
- Rotherham LSCB procedures (opens in new window)
- North Lincolnshire LSCB procedures (opens in new window)
- Incident management policy
- Lone working policy
- NSPCC Was Not Brought (opens in new window)
10 References
- Department of Education (DoE) (2018) keeping children safe in education.
- HM Government (2007) Statutory guidance on making arrangements to safeguard and promote the welfare of children under section 11 of the Children Act 2004. London Department of Education and Skills.
- HM Government (July 2018) Working together to safeguard children: a guide to inter-agency working to safeguard and promote the welfare of children (opens in new window).
- HM Government (July 2018) information sharing: advice for practitioners providing safeguarding services to children, young people, parents and carers (opens in new window).
- NICE, Child abuse and neglect, guidance and guidelines (opens in new window).
- The Children Act 1989, London: Office of public sector information (opens in new window).
- The Children Act 2004, London: Office of Public Sector Information (opens in new window).
11 Appendices
11.1 Appendix A Guidelines and prompts for the decision-making process and assessing risk
In order to promote the safety and wellbeing of all children and young people, it is vital that failure to attend is considered seriously. Any additional information or circumstances known to coexist with the current difficulty, which may exacerbate risk can be greatly varied and must be considered.
Whilst not an exhaustive list, the following prompts should be used to assist decision-making by practitioners, supervisors, teams or managers as indicators.
Those children, families or service users where:
- a referral to children social care has been made
- where children are subject to child in need or child protection plans
- the child is subject to early help
- the practitioner has attended or been invited to a professionals or strategy meeting
- there are concerns regarding an unborn child
- they are a looked after child either by order of the court or on a voluntary basis or cared for under a private fostering arrangement
- they are a vulnerable young person who has dependent children
- they are the dependent child of a vulnerable person
- they are the dependent child of a person known to have complex mental health problems or risk factors
- they are a child or young person with a co-existing learning or physical disability
- they are a vulnerable young person who has caring responsibilities
- they are the dependent child or young person of a person with problematic substance misuse
- they are the dependent child or young person of a person with a learning disability
- there are concerns regarding domestic abuse by adults in the household
- there are concerns regarding adult involvement in criminal activity within the household
11.2 Appendix B Person known to services does not attend, was not brought, at risk of disengagement, no access visit
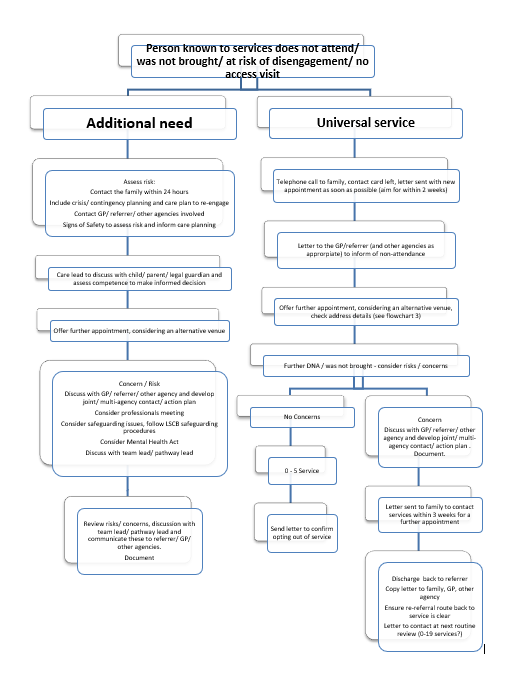
11.2.1 Additional need
- Assess risk:
- contact the family within 24 hours include crisis, contingency planning and care plan to re-engage
- contact GP, referrer, other agencies involved
- signs of safety to assess risk and inform care planning
- Care lead to discuss with child, parent, legal guardian and assess competence to make informed decision.
- Concern or risk:
- discuss with GP, referrer, other agency and develop joint, multiagency contact or action plan
- consider professionals meeting
- consider safeguarding issues, follow LSCB safeguarding procedures
- consider Mental Health Act
- discuss with team lead or pathway lead
- Review risks, concerns, discussion with team lead or pathway lead and communicate these to referrer, GP or other agencies or document.
11.2.2 Universal service
- Telephone call to family, contact card left, letter sent with new appointment as soon as possible (aim for within 2 weeks).
- Letter to the GP or referrer (and other agencies as appropriate) to inform of non-attendance.
- Offer further appointment, considering an alternative venue, check address details (see flowchart 3).
- Further DNA or was not brought, consider risks or concerns:
- if no concerns:
- 0 to 5 service
- Send letter to confirm opting out of service
- If it has concerns:
- discuss with GP, referrer, other agency and develop joint or multiagency contact or action plan. Document.
- letter sent to family to contact services within 3 weeks for a further appointment
- discharge back to referrer, copy letter to family, GP, other agency, ensure re-referral route back to service is clear, letter to contact at next routine review (0 to 19 services?)
- if no concerns:
11.3 Appendix C Missing young child or young person
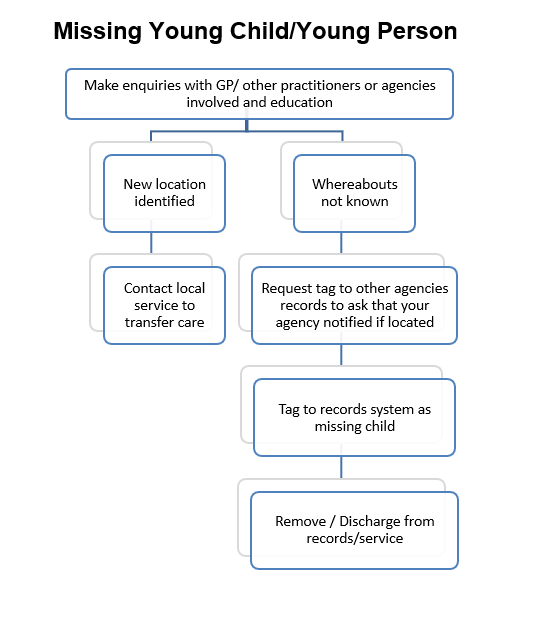
11.3.1 Make enquiries with GP or other practitioners or agencies involved and education
11.3.1.1 New location identified
- Contact local service to transfer care.
11.3.1.2 whereabouts not known
- Request tag to other agencies records to ask that your agency notified if located.
- Tag to records systems as missing child.
- Remove and discharge from records or service.
if an initial appointment is DNA or WNB a letter should be written to the GP informing them of this within 2 working days.
Document control
- Version: 5.1.
- Unique reference number: 375.
- Approved by: Clinical policies review and approval group.
- Date approved: 20 February 2024.
- Name of originator or author: CAMHS service manager and first contact practitioner.
- Name of responsible individual: Clinical policies review and approval group.
- Date issued: 27 February 2024.
- Review date: August 2024.
- Target audience: Children’s care group staff and staff within RDaSH.
Page last reviewed: April 30, 2024
Next review due: April 30, 2025