Contents
1 Policy summary
Female genital mutilation (FGM) is a procedure involving partial or total removal of the external female genitalia or other injury to the female genitalia for non-medical reasons. It is commonly known by other names including ‘female circumcision’, ‘cutting’, ‘initiation’ or ‘sunna’ (HM Government, 2020).
FGM is prevalent in 30 countries. These are concentrated in countries around the Atlantic coast to the horn of Africa, in areas of the Middle East, and in some countries in Asia.
It is estimated that approximately 103,000 women aged 15 to 49 and approximately 24,000 women aged 50 and over who have migrated to England and Wales are living with the consequences of FGM. In addition, approximately 10,000 females aged under 15 who have migrated to England and Wales are likely to have undergone FGM. The true extent is unknown due to the hidden nature of FGM. (HM Government, 2020).
FGM is a deeply embedded social norm, practised by families for a variety of complex reasons. It is often thought to be essential for a girl to become a proper woman, and to be marriageable. The practice is not required by any religion.
FGM is an unacceptable practice for which there is no justification. It is a form of violence and child abuse and as such colleagues have a statutory obligation under national safeguarding protocols (for example, working together to safeguard children 2015) to protect children and adults at risk of FGM.
2 Introduction
Multiagency statutory guidance (opens in new window) on female genital mutilation supports agencies to work together to protect and support those at risk of, or who have undergone, FGM. This guidance has further information to support colleagues and should be used in conjunction with this policy. Cases should be dealt with as part of existing structures, policies and procedures on child protection and adult safeguarding (HM Government, 2020).
There are characteristics of FGM that colleagues should be aware of to ensure that they can provide appropriate protection and support to those affected. The following principles should be adopted by all agencies in relation to identifying and responding to those at risk of, or who have undergone FGM, and their parent(s) or guardians:
- the safety and welfare of the child is paramount
- all agencies should act in the interests of the rights of the child, as stated in the United Nations convention on the rights of the child (1989)
- FGM is illegal in the UK
- FGM is an extremely harmful practice – responding to it cannot be left to personal choice
- accessible, high quality and sensitive health, education, police, social care, and voluntary sector services must underpin all interventions
- as FGM is often an embedded social norm, engagement with families and communities plays an important role in contributing to ending it
- all decisions or plans should be based on high quality assessments (in accordance with ‘Working Together to Safeguard Children’ (2018)
The Serious Crime Act (2015) (opens in new window) strengthens current FGM legislation and places a mandatory duty upon healthcare colleagues to notify the police when, in the course of their work, they identify that an act of FGM has been carried out on a female who is under 18 years of age. This must be completed as soon as possible after a case of FGM is discovered and it is advised to do this by the next working day. However, a maximum timeframe of one month is allowed for exceptional circumstances (HM Government, 2015b).
3 Purpose
To provide guidance and response to FGM and to assist all colleagues in the prevention and detection of FGM. The policy uses the term ‘female’ to represent people born with a vagina, clitoris, cervix and ovaries the biological sex of internal and external reproductive organs. It and is not a representation of a person’s gender identity.
Specifically, this guidance will aim to support colleagues to:
- ensure early Identification of FGM and act on any safeguarding issues that are identified for both adult and children
- appropriately share and record FGM information
- provide practical guidance for colleagues about the appropriate response and support for adults and children who have experienced or are at risk of FGM
- report to the police if they are informed by a child under the age of 18that an act of female genital mutilation (FGM) has taken place or observe physical signs that an act of FGM may have been carried out on a child under the age of 18. This is a mandatory requirement
4 Scope
This policy is applicable to all trust colleagues, agency colleagues and other colleagues not employed directly by the trust such as volunteers who in the course of their duties, may come into contact directly with, or who may become party to information about, safeguarding children’s issues.
5 Procedure or implementation
5.1 Quick guide
- Have you discussed FGM with the patient and their family? Use the quick guide for health professionals (opens in new window) for advice with starting the conversation.
- Have you completed an FGM risk assessment template (opens in new window)?
- Have you recorded your actions and the outcome of the assessment on the FGM template on the patient’s healthcare records? Ensure any risk is documented on both adults and child’s electronic record and place alert on child’s record if considered, at risk of or undergone, FGM.
- If you have identified a child at risk and undergone FGM have you followed local safeguarding procedure and made a referral to children social care? Complete a safeguarding incident form on Ulysses to inform RDaSH Safeguarding team.
- Have you reported a known case of FGM to a child under 18 to the police under the FGM mandatory reporting duty (opens in new window).
- Have you shared relevant information with health professionals including GP, health visitor, school nurse and the RDaSH Safeguarding team.
- Have you considered any ongoing specialist support for anyone affected by or undergone FGM?
5.2 General health care management principles
The Department of Health (2017) produced FGM safeguarding and risk assessment quick guide for health colleagues, the guidance has further information to support colleagues and should be used in conjunction with this policy. All RDaSH colleagues should be aware of the countries where FGM practice is prevalent and the factors to consider when deciding whether a girl or woman may be at risk of FGM. This knowledge will support colleagues to identify and consider any actions to take and will inform any subsequent plan.
It is important that colleagues are alert to indicators that FGM has already taken place so that:
- the adult or child receives the care and support they need
- enquiries can be made about any female children who may need to be safeguarded
- mandatory reporting and investigations can be considered
The WHO (2008) provides formal guidance on the classification of FGM. There are four types of FGM which are classified, however, in practice it may not always be possible to specify exactly which type of FGM applies in every case. Please note, examination to confirm findings following a disclosure of FGM is not required.
There is no mandatory requirement to routinely ask every child and adult if they have had FGM however colleagues must be aware of FGM indicators and risk factors, including country of origin and to use their professional judgement to decide when it is appropriate to ask a patient if they have had FGM (DOH, 2017).
5.3 The law in England and Wales
FGM is illegal in England and Wales under the Female Genital Mutilation Act since 2003. The FGM Act was subsequently strengthened by the Serious Crime Act (2015) and introduced the mandatory requirement for specified colleagues to report to the Police any known cases of FGM in under 18 year olds that have been identified in the course of professional employment. The amendment also included the use of FGM Protection Orders (see point 5.10) which can be used to protect children at risk and give lifelong anonymity for victims of FGM.
Further offences were added as follows:
- extra-territorial jurisdiction over offences of FGM committed abroad by UK nationals
- an offence of failing to protect a child from the risk of FGM
More detailed information is contained within chapter 3 of multi agency statutory guidance on female genital mutilation (opens in new window) (HM Government, 2020).
5.4 FGM Mandatory reporting
The FGM mandatory reporting duty is a legal duty as stated in the FGM Act (2003) (opens in new window) (as amended by the Serious Crime Act 2015).
Failing to comply with the duty is likely to be dealt with through existing disciplinary measures which may include referral to the relevant professional regulator.
The legislation requires regulated health professionals in England to make a report to the police where, in the course of their professional duties they either:
- are informed by a female child or young person under the age of 18 that an act of FGM has been carried out on them
- observe physical signs which appear to show that an act of FGM has been carried out on a female child or young person under the age of 18 and they have no reason to believe that the act was necessary for the child’s physical or mental health or for purposes connected with labour or birth
Reports under this duty should be made as soon as possible and it is best practice to do this by the end of the next working day. However, to allow for exceptional cases, a maximum timeframe of one month is allowed.
For the purposes of the mandatory reporting duty the age is any female currently under the age of 18 (for example, it does not apply where a woman aged 18 or over discloses she had FGM when she was under 18).
Complying with the duty does not breach any confidentiality requirement or other restriction on disclosure which might otherwise apply. The duty is a personal duty which requires the individual professional who becomes aware of the case to make a report; the responsibility cannot be transferred. The only exception to this is if you know that another individual from your profession has already made a report; there is no requirement to make a second.
5.5 FGM protection orders (FGMPO)
An FGMPO (opens in new window) is a civil order which may be made for the purpose of protecting a child who is at risk of FGM, or against who an FGM offence has been committed. The court can make an order which prohibits, requires, restricts as it considers appropriate to stop those who would seek to subject a child to FGM or have already arranged for, or committed, FGM. Examples of the types of orders the court might make:
- to protect a victim or potential victim from being taken abroad
- to order the surrender of passports or any other travel documentation of the child to be protected
- to include terms which relate to the conduct of the individuals named in the order both inside and outside of England and Wales
Orders may be made against people who are not named in the application. This is due to the numbers of people who may be involved in the wider community.
5.6 Safeguarding principles, adult
If an adult patient discloses FGM or if a colleague suspects that an adult has undergone FGM or are considered at risk of FGM consideration should be given to any physical or emotional needs a woman may be experiencing, and consent should be gained to signpost or refer to any appropriate specialist services.
When discussing FGM with a woman ensure she is seen alone and be sensitive to the intimate nature of the subject. Language barriers should not prevent discussion regarding FGM, ensure RDaSH approved interpreter services are used and not family members.
If the woman is pregnant or has female children, the welfare of the unborn child or others in her extended family must also be considered (see point 5.5). The Department of Health (2017) have provided risk assessment tools (opens in new window) to support colleagues when considering the safeguarding risks posed to both girls and women. Assessment of risk should include consideration of country of origin, presenting clinical symptoms and other social information. There is no mandatory requirement for automatic referral of adult women to social care or the police as there is with a child however support should be offered if they wish to report to the police as a crime.
If the adult patient is vulnerable or at risk’ then local safeguarding procedures should be followed.
5.7 Additional safeguarding considerations
5.7.1 Domestic abuse
FGM and forced marriage, which may accompany FGM, is recognised as forms of domestic abuse and consideration should be made for any other acts of controlling or coercive behaviour. Local safeguarding procedures should be followed. For further information see domestic abuse policy.
5.7.2 Breast flattening
In some countries large stones, a hammer or spatulas that have been heated over scorching coals can be used to compress the breast tissue, this is known as breast flattening or ironing.
The practice is performed to help disguise the onset of puberty in females, which it is believed will help to deter male attention and protect them from sexual harassment, assault, exploitation, and rape or sexually transmitted diseases.
Although there is no specific law within the UK around breast flattening or breast ironing, it is a form of physical abuse and if colleagues are concerned a child may be at risk of, or suffering significant harm, they must refer to their local safeguarding procedures.
It should also be acknowledged that some young people may choose to bind their breasts using constrictive material due to gender transformation or identity.
5.8 Safeguarding principles: children
FGM is a harmful and illegal act to which a child is unable to resist or consent. FGM places a child at risk of or undergone significant harm under section 47 of the Children Act (1989)(opens in new window) and is classified as a form of physical child abuse, it must therefore be addressed within the framework of child protection as stated in working together to safeguard children (2018).
Where FGM is suspected in a child, or there is a risk it may take place colleagues should:
contact the police If you suspect a child is at immediate risk of harm from FGM
make a referral into children’s social care in accordance with local safeguarding children’s board’s procedures
inform your line manager and the RDaSH Safeguarding team for advice
if a child has undergone FGM report to the police as mandatory duty
share information with the child’s GP, health visitor or school nurse
complete the FGM data set on child’s SystmOne records (found on the safeguarding templates)
- complete an IR1
Cases involving FGM can be complex depending on the presenting factors and circumstances, further management of each case will need to be assessed on an individual basis. Advice and guidance can also be accessed from:
- RDaSH named doctor safeguarding children
- RDaSH nurse consultant safeguarding
- RDaSH named nurse or professional safeguarding children and adults
- children or adult social care
- the police
- the NSPCC
5.9 Documentation and data collection
The Department of Health’s FGM prevention programme is supported by:
- delivering a digital system to strengthen the safeguarding of girls at risk of FGM. This is female genital mutilation, information sharing (FGM-IS) which provides a national information technology system for healthcare colleagues to record that a girl has a family history of FGM. The FGM-IS is part of the NHS spine. The Safeguarding team can view, add and remove the FGM indicator, and it can be accessed via the summary care record application (SCRa), or with a local clinical system integrated with FGM-IS
- presenting a national picture of the prevalence of FGM across the NHS in England. This is the female genital mutilation enhanced dataset. NHS digital collects data on FGM within the NHS in England on behalf of the Department of Health (DH). The data collected is used to produce information that helps to:
- improve how the NHS supports women and girls who have had or who are at risk of FGM
- plan the local NHS services needed both now and in the future
- help other organisations, for example, local authorities to develop plans to stop FGM happening in local communities
Data is collected from NHS acute trusts; mental health trusts and GP practices and reports are published as an official statistic every quarter.
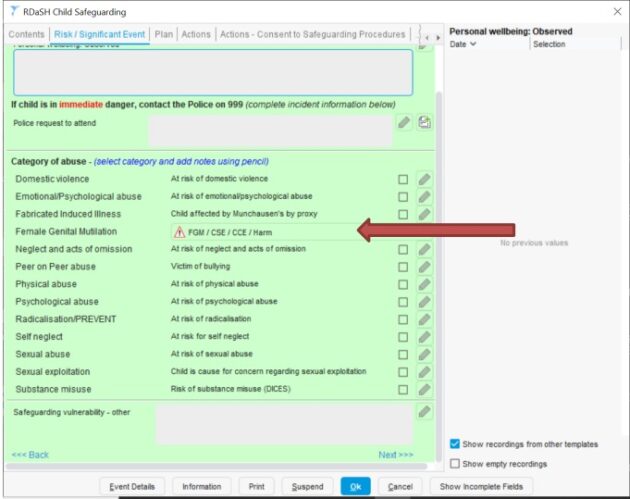
If FGM is disclosed or identified during any healthcare consultation this should be documented within the FGM page in the patients’ electronic records. This can be accessed within the child safeguarding template under risk or significant event see below:

Risk or significant event tab. 
RDaSH FGM form tab. 
FGM enhanced dataset. Documentation should include:
- completion of the FGM template, for example, FGM identified, parent has undergone FGM, child at risk of FGM including the FGM enhanced dataset within the safeguarding template
- all observations made relating to the identification of FGM or risk of FGM
- all actions taken
- all information shared and with whom or, documentation why they have chosen not to share information
Please note if during a consultation with an adult female you have identified a child at risk, this must be recorded in both the adult and child’s records using the FGM page within the safeguarding module.
A Ulysses incident form (IR1) should then be completed for every case of FGM that is identified ensuring the incident is recorded as child or adult safeguarding, even if this has not subsequently resulted in a referral to social care. This reporting mechanism is to ensure that the safeguarding team have oversight of all cases involving FGM.
5.10 Information sharing
In the UK, the duty to share information where there is a concern or risk to a person or child’s welfare, is more important that the right to confidentiality. Healthcare colleagues have a professional and statutory duty to record, refer and share information where there is a significant ‘public interest’ to do so. Information sharing is a crucial part of early intervention and prevention of FGM.
If identified by a healthcare professional, information should be shared with the child’s GP, health visitor or school nurse (dependent on age of child) and potentially other professional delivering care to the child depending upon circumstances.
Where colleagues remain in doubt regarding information sharing, they should contact the RDaSH Safeguarding team for advice.
If a decision is taken not to share, then the reason for this should be documented clearly in the patients’ healthcare record.
6 Training implications
6.1 Recognising and preventing FGM
- Employee groups requiring training: All colleagues required to undertake level 3 safeguarding adults and children training.
- Frequency: Once.
- Length of training: 60 minutes.
- Delivery method: e-learning.
- Training delivered by: training link (opens in new window).
- Where are the records of attendance held: ESR.
7 Equality impact assessment screening
To access the equality impact assessment for this policy, please email rdash.equalityanddiversity@nhs.net to request the document.
7.1 Privacy, dignity and respect
The NHS Constitution states that all patients should feel that their privacy and dignity are respected while they are in hospital. High Quality Care for All (2008), Lord Darzi’s review of the NHS, identifies the need to organise care around the individual, ‘not just clinically but in terms of dignity and respect’.
Consequently, the trust is required to articulate its intent to deliver care with privacy and dignity that treats all service users with respect. Therefore, all procedural documents will be considered, if relevant, to reflect the requirement to treat everyone with privacy, dignity, and respect, (when appropriate this should also include how same sex accommodation is provided).
7.1.1 Indicate how this will be met
No issues have been identified in relation to this policy.
7.2 Mental capacity act
Central to any aspect of care delivered to adults and young people aged 16 years or over will be the consideration of the individual’s capacity to participate in the decision-making process. Consequently, no intervention should be carried out without either the individual’s informed consent, or the powers included in a legal framework, or by order of the court.
Therefore, the trust is required to make sure that all colleagues working with individuals who use our service are familiar with the provisions within the Mental Capacity Act (2005). For this reason, all procedural documents will be considered, if relevant to reflect the provisions of the Mental Capacity Act (2005)to ensure that the rights of individual are protected, and they are supported to make their own decisions where possible and that any decisions made on their behalf when they lack capacity are made in their best interests and least restrictive of their rights and freedoms.
7.2.1 Indicate how this will be achieved
All individuals involved in the implementation of this policy should do so in accordance with the guiding principles of the Mental Capacity Act 2005.
8 Links to any other associated documents
- Domestic abuse policy
- Female genital mutilation classification (opens in new window)
- Female genital mutilation (FGM) protection orders guidance (opens in new window)
- Female genital resource pack (opens in new window)
- FGM safeguarding and risk assessment quick guide for health colleagues opens in new window)
- FGM safeguarding pathway (opens in new window)
- Multiagency statutory guidance on female genital mutilation (opens in new window)
- National FGM centres: resources for health (opens in new window)
- Safeguarding adult policy
- Safeguarding children policy
9 References
- Department of health (2017) Female genital mutilation risk and safeguarding for colleagues (opens in new window).
- FGM safeguarding and risk assessment quick guide for health colleagues (2017) (opens in new window).
- Home office (2020) multiagency statutory guidance on female genital mutilation (opens in new window).
- HM government (1989). Children Act 1989 (opens in new window).
- HM government (2018) Working together to safeguard children.
- Legislative GOV.UK (2015). Serious Crime Act 2015 (opens in new window).
- UNICEF UK (1989): The United Nations convention on the rights of the child (opens in new window).
- World Health Organisation. Female genital mutilation. [online] (opens in new window).
10 Appendices
10.2 Appendix A Responsibilities, accountabilities and duties
The trust, the chief executive and directors of the trust are responsible for ensuring that robust systems are in place to identify and manage the risks associated with safeguarding adult at risk and to support the effective multiagency partnership working and responses which are required.
This includes the identification and training of suitable staff to fulfil the roles set out within the multiagency safeguarding adult’s procedures. All staff are responsible for fulfilling their responsibilities to safeguard adult at risk.
The trust’s nominated executive director: The trust has a nominated executive director for safeguarding, who takes a professional lead in promoting best practice in safeguarding at board level. In this trust, the nominated executive director for safeguarding adults is the director of nursing and allied health professionals.
Deputy director of nursing (operational lead) has responsibility to provide expert advice, strategic and operational leadership for safeguarding and professional standards. To continually develop a proactive approach to safeguarding through collaboration with the local authority and other agencies. To ensure all mandatory and statutory requirements around safeguarding are met and develop support systems.
Nurse consultant safeguarding has responsibility to provide expert advice, strategic and operational leadership for safeguarding and professional standards. To continually develop a proactive approach to safeguarding through collaboration with the local authority and other agencies. To ensure all mandatory and statutory requirements around safeguarding are met and develop support systems.
Named nurses or named professionals (practice leads) have responsibility to provide an expert professional leadership role in relation to safeguarding adults. To work at a strategic level across the health and the social care community, fostering and facilitating multiagency working and training in respect of safeguarding adults. To act as an expert resource on safeguarding adults issues, providing accessible, accurate and relevant information to colleagues.
The practice leads are responsible for delivering support, advice and guidance to the safeguarding managers, safeguarding supervisors and enquirers.
They have a key role in promoting best practice and are available as a source of advice or guidance and support for managers and staff involved in safeguarding.
Service managers, modern matrons or area clinical managers are responsible for:
- ensuring all colleagues have access to the relevant multiagency safeguarding procedures in their workplace
- maintaining compliance with the policy and multiagency safeguarding procedures within their services
- arranging staff attendance at training, updates in relation to safeguarding
- providing support for staff involved in safeguarding adults
Employees of RDaSH: ‘Safeguarding is everybody’s business’.
All employees (including volunteers) have a responsibility to safeguard and promote the wellbeing of children and adults at risk of harm. Employees must be able to recognise and report safeguarding concerns to their line manager or the Safeguarding team to ensure actions can be taken to address the concerns.
10.2 Appendix B Monitoring arrangements
10.2.1 Adherence to safeguarding procedures
- How: Audit.
- Who by: Safeguarding team.
- Reported to: Safeguarding assurance group.
- Frequency: Annually.
10.3 Appendix C Actions to be taken if a child or young person is at risk of FGM

- Is the child or young person at immediate risk of harm from FGM?
- if no, clinical contact, include assessment of risk
- gather information using the ‘talking about FGM’ guide
- assess risk and complete the risk assessment tool to guide decision making
- is this a new risk? Or has the risk increased since the last contact with the child?
- consider whether other children are at risk in the immediate or extended family
- discuss the case with your line manager and inform the RDaSH Safeguarding team
- if required, make a referral into children’s social care
- discuss the referral with the parents if it is safe to do so for example, unless by doing so the child would be placed at an elevated level of risk
- discuss the case at safeguarding supervision
- if yes, advice and referral
- contact police on 999
- refer to children’s social care
- contact line manager and the RDaSH Safeguarding team for advice and support
- if no, clinical contact, include assessment of risk
- Documentation:
- document all observations, concerns and any actions taken in the healthcare record
- complete a safeguarding incident form on Ulysses
- Information sharing:
- information sharing is a crucial part of early intervention and FGM prevention. Consider sharing information with: health visitor, GP, school nurse and midwife
- if a decision is taken not to share information this should be recorded in the health records with the rationale for this
10.4 Appendix D Actions to be taken if someone has already been subjected to FGM
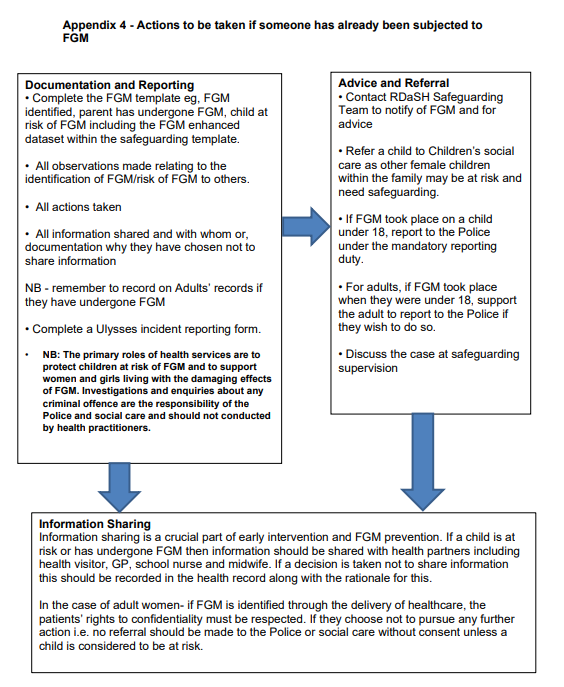
- Documentation and reporting:
- complete the FGM template, for example, FGM identified, parent has undergone FGM, child at risk of FGM including the FGM enhanced dataset within the safeguarding template
- all observations made relating to the identification of FGM or risk of FGM to others
- all actions taken
- all information shared and with whom or, documentation why they have chosen not to share information. Note: remember to record on Adults’ records if they have undergone FGM
- complete a Ulysses incident reporting form. Note, the primary roles of health services are to protect children at risk of FGM and to support women and girls living with the damaging effects of FGM. Investigations and enquiries about any criminal offence are the responsibility of the police and social care and should not conducted by health practitioners
- Advice and referral:
- contact RDaSH Safeguarding team to notify of FGM and for advice
- refer a child to children’s social care as other female children within the family may be at risk and need safeguarding
- if FGM took place on a child under 18, report to the Police under the mandatory reporting duty
- for adults, if FGM took place when they were under 18, support the adult to report to the police if they wish to do so
- discuss the case at safeguarding supervision
- Information sharing:
- information sharing is a crucial part of early intervention and FGM prevention. If a child is at risk or has undergone FGM then information should be shared with health partners including health visitor, GP, school nurse and midwife. If a decision is taken not to share information this should be recorded in the health record along with the rationale for this. In the case of adult women, if FGM is identified through the delivery of healthcare, the patients’ rights to confidentiality must be respected. If they choose not to pursue any further action for example, no referral should be made to the police or social care without consent unless a child is considered to be at risk
Document control
- Version: 1.
- Unique reference number: 1045.
- Approved by: Clinical policies review and approval group.
- Date approved: 4 July 2023.
- Name of originator or author: Nurse consultant for safeguarding.
- Name of responsible individual: Executive director of nursing and allied health professionals.
- Date issued: 13 July 2023.
- Review date: 31 July 2025.
- Target audience: All staff within the trust
Page last reviewed: April 30, 2024
Next review due: April 30, 2025