Contents
1 Introduction
1.1 What is PREVENT?
The office for security and counter terrorism (OSCT) in the Home Office is responsible for providing strategic direction and governance on CONTEST (government counter terrorism strategy). As part of CONTEST, the aim of PREVENT is to stop people becoming terrorists or supporting terrorism.
CONTEST is primarily organised around four key principles. Work streams contribute to four programmes, each with a specific objective:
- PURSUE, to stop terrorist attacks
- PREVENT, to stop people becoming terrorists or supporting terrorism
- PROTECT, to strengthen our protection against a terrorist attack
- PREPARE, to mitigate the impact of a terrorist attack
The health service is a key partner in PREVENT and encompasses all parts of the NHS, charitable organisations and private sector bodies which deliver health services to NHS patients.
PREVENT has 3 national objectives:
- objective 1, respond to the ideological challenge of terrorism and the threat we face from those who promote it
- objective 2, prevent people from being drawn into terrorism and ensure that they are given appropriate advice and support
- objective 3, work with sectors and institutions where there are risks of radicalisation which we need to address
The health sector contribution to PREVENT will focus primarily on objectives 2 and 3. PREVENT training undertaken in line with objectives 2 and 3 will be known as HealthWRAP training.
1.2 Why health care staff?
The overall principle for health providers is to improve the health and wellbeing through the delivery of healthcare services while safeguarding those individuals who are vulnerable to any form of exploitation. PREVENT is also about protecting individuals.
PREVENT aims to protect those who are vulnerable to exploitation from those who seek to get people to support or commit acts of violence.
Healthcare staff are well placed to recognise individuals, whether patients or staff, who may be vulnerable and therefore more susceptible to radicalisation by extremists or terrorists. It is fundamental to our ‘duty of care’ and falls within our safeguarding responsibilities.
Every member of staff has a role to play in protecting and supporting vulnerable individuals and colleagues who are at risk of radicalisation.
2 Purpose
This policy describes how the trust implements the PREVENT agenda. The PREVENT agenda ensures that:
- NHS staff know how to safeguard and support vulnerable individuals, whether patients or service users or staff, who they feel may be at risk of being radicalised by extremists
- appropriate systems are in place within NHS organisations for staff to raise concerns if they think this form of exploitation is taking place
- healthcare organisations promote and operate safe environments where extremists are unable to operate
3 Scope
The PREVENT agenda is relevant to all our staff, including volunteers, in particular those who work with vulnerable people.
4 Responsibilities, accountabilities and duties
4.1 The director of nursing and quality
The director of nursing and quality is responsible for:
- managing the PREVENT strategy and policy documents on behalf of the trust
4.2 The deputy director of nursing and quality
The deputy director of nursing is responsible for:
- liaising with the director of nursing and quality to manage the PREVENT Strategy
- the implementation and operation of the PREVENT strategy
4.3 The head of education
The head of education is responsible for:
- making arrangements for a suitable number of training places and events to be delivered to allow all relevant staff identified in the training needs analysis to access the HealthWRAP training programme
- liaising with the HealthWRAP trainers to plan and implement a HealthWRAP training and awareness programme
- providing training reports to the trust as required
4.4 Nurse consultant for safeguarding
The nurse consultant for safeguarding is responsible for:
- acting as lead advisor on PREVENT strategy and implementation
- acting as advisor to the HealthWRAP trainers
- providing data to NHS England and clinical commissioning groups as required
4.5 Safeguarding adults leads or safeguarding children named nurses
The safeguarding adult leads and safeguarding children named nurses are responsible for:
- providing support and advice on PREVENT concerns raised by staff
- assisting managers to take concerns to the appropriate authority
- delivering the HealthWRAP training and awareness programme
4.6 Team managers, service managers and associate nurse directors (ANDs)
Managers are responsible for:
- arranging for staff to attend the HealthWRAP training as required
- supporting staff with the processes to escalate a concern
- facilitating the appropriate escalation of PREVENT concerns (see the flowchart in appendix A)
- liaising with human resources department if the concern raised is about a member of staff
4.7 All trust staff
All members of trust staff (including volunteers) are responsible for:
- completing the required PREVENT Health WRAP training session face to face or online
- reporting all PREVENT related concerns to their manager in line with the escalation flowchart in appendix A
- assisting their manager in appropriate escalation
5 Procedure and implementation
5.1 The process of exploitation
It is suggested that there is no single profile or indication of a person who is likely to become involved in terrorist-related activity. To date there is no universally accepted view of why vulnerable individuals become involved.
The factors surrounding exploitation are many and they are unique for each person. The increasing body of information indicates that factors thought to relate to personal experiences of vulnerable individuals affect the way in which they relate to their external environment.
In this sense, vulnerable individuals may be exploited in many ways by radicals who target the vagaries of their vulnerability. Contact with radicals is also variable and can take a direct form, for example, face to face, or can happen indirectly through the internet, social networking or other media. More commonly this will occur through a combination of the above.
5.2 Contact with radicals
It is generally more common for vulnerable individuals to become involved in terrorist-related activity through the influence of others. Initial contact may be via peers, siblings, other family members or acquaintances, with the process of radicalisation often being a social one. Such social interaction takes place in a range of unsupervised environments such as gyms or cafés, in private homes and via the internet.
Access to extremist material is often through leaflets and local contacts. However, the internet plays an important role in the communication of extremist views. It provides a platform for extremists to promote their cause and encourage debate through websites, internet forums and social networking, and is a swift and effective mechanism for disseminating propaganda material. Healthcare organisations should be aware of anyone making frequent visits to websites showing images such as armed conflict around the world and providing speeches and access to material from those involved in the radicalising process.
5.3 Use of extremist rationale (often referred to as ‘narrative’)
Radicals usually attract people to their cause through a persuasive rationale contained within a storyline or narrative that has the potential to influence views. Inspiring new recruits, embedding the beliefs of those with established extreme views and or persuading others of the legitimacy of their cause is the primary objective of those who seek to radicalise vulnerable individuals.
5.4 What factors might make someone vulnerable?
In terms of personal vulnerability, the following factors may make individuals susceptible to exploitation. None of these are conclusive in themselves and therefore should not be considered in isolation but in conjunction with the particular circumstances and any other signs of radicalisation.
5.4.1 Identity crisis
Adolescents or adults at risk who are exploring issues of identity can feel both distant from their parents or family and cultural and religious heritage, and uncomfortable with their place in society around them. Radicals can exploit this by providing a sense of purpose or feelings of belonging. Where this occurs, it can often manifest itself in a change in a person’s behaviour, their circle of friends, and the way in which they interact with others and spend their time.
5.4.2 Personal crisis
This may, for example, include significant tensions within the family that produce a sense of isolation of the vulnerable individual from the traditional certainties of family life.
5.4.3 Personal circumstances
The experience of migration, local tensions or events affecting families in countries of origin may contribute to alienation from UK values and a decision to cause harm to symbols of the community or state.
5.4.4 Unemployment or under-employment
Individuals may perceive their aspirations for career and lifestyle to be undermined by limited achievements or employment prospects. This can translate to a generalised rejection of civic life and adoption of violence as a symbolic act.
5.4.5 Criminality
In some cases a vulnerable individual may have been involved in a group that engages in criminal activity or, on occasion, a group that has links to organised crime and be further drawn to engagement in terrorist-related activity.
5.4.6 Grievances
The following are examples of grievances which may play an important part in the early indoctrination of vulnerable individuals into the acceptance of a radical view and extremist ideology:
- a misconception and or rejection of UK foreign policy
- a distrust of western media reporting
- perceptions that UK government policy is discriminatory (for example, counterterrorist legislation)
5.4.7 Other factors
Similarly to the above, the following have also been found to contribute to vulnerable people joining certain groups supporting terrorist-related activity:
- ideology and politics
- provocation and anger (grievance)
- need for protection
- seeking excitement and action
- fascination with violence, weapons and uniforms
- youth rebellion
- seeking family and father substitutes
- seeking friends and community
- seeking status and identity
5.5 Raising concerns about service users
If a member of staff has a concern that someone is being radicalised, then they should discuss the concerns with their manager and or relevant safeguard professional, to decide if the concerns are valid. Please refer to the flowchart in appendix A.
Once the concern has been recognised as valid, complete an IR1 incident report; refer to the flowchart in appendix A.
If the concern is deemed to be valid the channel process (forum for considering interventions for those who are at risk of radicalisation) should be followed by the manager or safeguarding lead in partnership with the local police PREVENT lead.
All concerns, discussions and advice should be documented in line with trust policy.
If anyone has immediate concerns that an individual is presenting an immediate terrorist risk to themselves, others or property, then they should contact the national counter-terrorism hotline on 0800 789 321, or the police on 999.
6 Training implications
All staff are to be made aware of the PREVENT strategy and how it is being implemented within the trust. This is facilitated by, for example, payslip attachments, trust-wide communication processes such as team meetings, and during induction.
All staff who work with patients and service users will attend a HealthWRAP and PREVENT training and awareness session, or complete this via eLearning
These sessions will ensure that staff are:
- aware of their professional responsibilities, particularly in relation to the safeguarding of adults at risk and children
- familiar with the trust’s relevant protocols, policies and procedures
- aware of who they should contact to discuss concerns
- aware of the processes and support available when they raise a concern
6.1 Training needs analysis
6.1.1 PREVENT HealthWRAP trainers
- How often should this be undertaken: Once.
- Length of training: 2 days.
- Delivery method: Lecture.
- Training delivered by whom: External trainers.
- Where are the records of attendance held: Electronic staff record system (ESR).
6.1.2 All clinical staff and staff who work with patients or service users on a regular basis
- How often should this be undertaken: Once.
- Length of training: 1 to 1 and half hours.
- Delivery method: Delivered via induction programmes and bespoke sessions.
- Training delivered by whom: Approved HealthWRAP tutors.
- Where are the records of attendance held: Electronic staff record system (ESR).
7 Monitoring arrangements
7.1 Successful completion of HealthWRAP training
- How: Numbers successfully completing.
- Who: Head of education as part of annual training report.
- Reported to: HR and OD Group.
- Frequency: Annually.
7.2 Concerns raised (including pre-PREVENT discussion)
- How: Number of concerns reported via the IR1 system.
- Who: Consultant for safeguarding.
- Reported to: Risk management group.
- Frequency: Quarterly.
8 Equality impact assessment screening
The completed equality impact assessment for this policy has been published on this policy’s webpage on the trust policy library or archive website.
Link to equality impact assessment: Prevent strategy policy EIA.
8.1 Privacy, dignity and respect
The NHS constitution states that all patients should feel that their privacy and dignity are respected while they are in hospital. High quality care for all (2008), Lord Darzi’s review of the NHS, identifies the need to organise care around the individual, ‘not just clinically but in terms of dignity and respect’.
As a consequence the trust is required to articulate its intent to deliver care with privacy and dignity that treats all service users with respect. Therefore, all procedural documents will be considered, if relevant, to reflect the requirement to treat everyone with privacy, dignity and respect, (when appropriate this should also include how same sex accommodation is provided).
8.1.1 How this will be met
There are no additional requirements in relation to privacy, dignity and respect. Central to any aspect of care delivered to adults and young people aged 16 years or over will be the consideration of the individuals capacity to participate in the decision making process. Consequently, no intervention should be carried out without either the individual’s informed consent, or the powers included in a legal framework, or by order of the court.
Therefore, the trust is required to make sure that all staff working with individuals who use our service are familiar with the provisions within the mental capacity act. For this reason all procedural documents will be considered, if relevant to reflect the provisions of the Mental Capacity Act (2005) to ensure that the rights of individual are protected and they are supported to make their own decisions where possible and that any decisions made on their behalf when they lack capacity are made in their best interests and least restrictive of their rights and freedoms.
8.2.1 How this will be met
All individuals involved in the implementation of this policy should do so in accordance with the guiding principles of the Mental Capacity Act 2005 (section 1).
9 Links to any associated documents
10 References
- Building partnerships, staying safe, the health sector contribution to HM.
- Government’s PREVENT strategy: guidance for healthcare workers, Department of Health, November 2011.
- Counter Terrorism and Security Act, HM government, 2015.
11 Appendices
11.1 Appendix A Raising a prevent concern (flow chart)
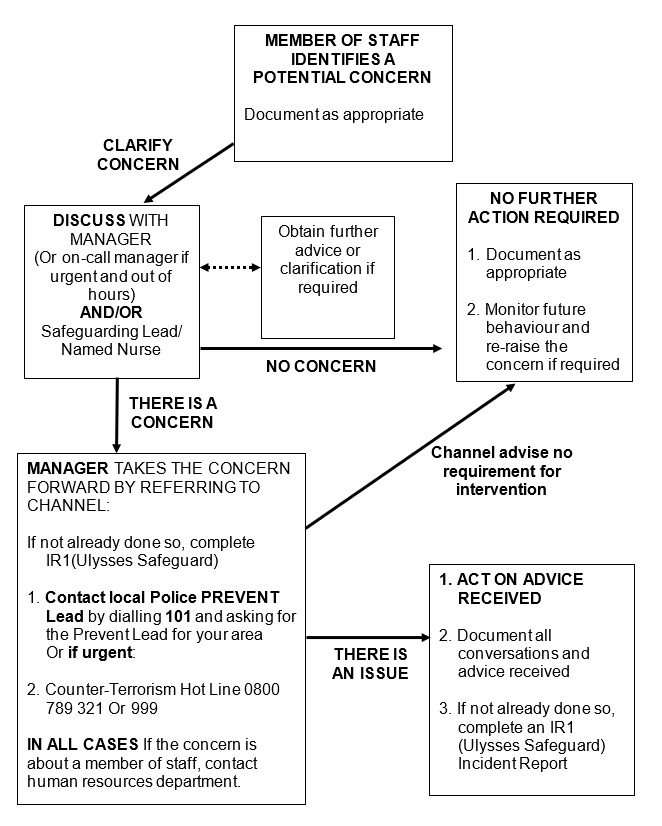
- Member of staff identifies a potential concern. Document as appropriate.
- Clarify concern.
- Discuss with manager (or on-call manager if urgent and out of hours) and, or safeguarding lead or named nurse. Obtain further advice or clarification if required.
- no concern, no further action required, document as appropriate and monitor future behaviour and re-raise the concern if required
- There is a concern, manager takes the concern forward by referring to channel:
- if not already done so, complete IR1 (Ulysses Safeguard)
- contact local police prevent lead by dialling 101 and asking for the prevent lead for your area
- or if urgent counter-terrorism hot line 0800 789321 or 999
- in all cases if the concern is about a member of staff, contact human resources department
- If channel advise no requirement for intervention, no further action required, document as appropriate and monitor future behaviour and re-raise the concern if required.
- If there is an issue, act on advice received:
- document all conversations and advice received
- if not already done so, complete an IR1 (Ulysses Safeguard) incident report
Document control
- Version: 5.1.
- Unique reference number: 155.
- Approved by: Clinical policy review and approval group.
- Date approved: 5 March 2024.
- Name of originator or author: Safeguarding adults lead.
- Name of responsible committee or individual: Executive director of nursing and allied health professionals.
- Date issued: 2 April 2024.
- Review date: 30 June 2024.
- Target audience: All staff.
Page last reviewed: April 25, 2024
Next review due: April 25, 2025