1 Policy summary
The primary care mental health service (PCMHS) is part of the primary and community mental health transformation programme for adults and older adults, implementing care through promoting wellbeing, prevention, and enablement of the patient group. Adopting a “no wrong door” approach, reflecting wherever patients seek their support they will be seamlessly guided to the most appropriate service rather than referred to another part of the mental health system. The purpose is to balance the patient seeking contact “as and when” needed, aiming to prevent illness or a worsening of symptoms. This reflects access to care not just when the patient is ill but according to the need to maintain wellbeing. This approach will encourage the patient to maintain individual responsibility for their health, wherever possible and appropriate.
2 Introduction
Traditionally, mental health services have a complex series of pathways and teams. The use of differing referral criteria, standards and processes create a system that is complex for those working within the system and for patients alike (NHS Sheffield, September 2021).
The NHS long term plan (NHS England and NHS Improvement, 2019) makes a renewed commitment to improve and widen access to care for adults needing mental health support.
The Community Mental Health Framework for Adults and Older Adults (2019) focusses on “putting community at the centre of community mental health services”. Local areas have been supported to ‘redesign and reorganise core community mental health teams to move towards a new place-based, multi-disciplinary service across health and social care aligned with primary care networks (PCNs).
Since November 2022, a clearly defined model (appendix C) was created to show how people with a serious mental illness could be supported in their recovery.
Individuals and communities can maximise their health and wellbeing potential utilising new and existing community assets via an integrated care system approach. The patient’s journey will be to access the right care, support and treatment at the right time and to have a clear journey, not be passed around the health system. Patient journeys are to be considered as “step-up”, “step-down” or “move-across” to the most appropriate intervention rather than the notion of referral and discharge, thus removing the barriers patients currently experience between primary and secondary care.
Where a patient is in a service that is not right for them, we will navigate them to the appropriate service or support.
PCNs are based on GP registered lists, typically serving natural communities of around 30,000 to 50,000. They are small enough to provide the personal care valued by both patients and GPs, but large enough to have impact and economies of scale through better collaboration between practices and others in the local health and social care system. Included within these PCNs are more specific clinical functions, the provision of mental health care being one of them. (NHS England)
The introduction of the PCMHS will incorporate the following:
- the introduction of PCN mental health practitioners (MHP), along with mental health and wellbeing triage coaches (MHWBTC) where applicable, in the Rotherham, Doncaster and North Lincolnshire PCN’s through the new additional roles reimbursement scheme (ARRS)
- establishing the primary care mental health hub (PCMHH) aligned as per PCN commissioning, which is tabled in appendix D
The primary care mental health service operates a model of delivery akin to general practices meaning all people registered to a general practitioner (GP) will be able to access the service (where they meet the eligibility criteria) without traditional GP referrals. As many mental health conditions are dynamic in terms of severity, longevity, and complexity, it is expected that people will have their needs met via self-management or community support without needing specialist mental health clinical input. Times will exist where the person needs to re-access clinical support services, and this should be easy and frictionless, joint working will see a number of people re-access support at a point where their condition has not deteriorated as significantly as in previous episodes of care (NHS Sheffield, September 2021).
The primary care mental health service works as an integrated part of a PCN. In collaboration with GPs, social care, voluntary, community and social enterprise (VCSE) providers, patients, family members and carers and wider specialist mental health teams work to support good physical, psychological and social wellbeing for the PCN population, while ensuring responsive access to patients with the most complex of presentations.
3 Purpose
This policy sets the processes and procedures that the primary care mental health service, including ARRS roles, are required to follow to ensure safe, quality and effective care for our patients. This is in line with the national community mental health transformation and the goals set by NHS England.
The purpose of the PCMHS is to improve coordination and collaboration of services. The aim of the team is to:
- provide an inclusive community based-offer, integrating community mental health services with PCN’s
- remove traditional barriers between primary care mental health, specialist mental health and VCSE mental health provision, through new models of care, moving away from referral and discharge systems that lead to cliff edges
- help prevent individuals from falling between gaps in services, such as those whose needs are higher than what Talking Therapies can offer but do not meet the traditional thresholds for specialist mental health teams; or those who have not engaged with specialist mental health services as they require support to reach these interventions. To overcome this, evidence-based interventions will be provided at a PCN level for people with serious mental illness and complex emotional needs (traditionally defined as personality disorder)
- work in partnership with commissioned VCSE services, in order to:
- provide better care to people already receiving mental health support in the community
- increase access to community based support services
- support people with severe mental illness (SMI) receive a comprehensive physical health check
4 Scope
This document will apply to all Rotherham, Doncaster, and South Humber NHS Foundation Trust (RDaSH) colleagues including substantive, temporary, those on honorary contracts and locum, of all grades and disciplines, working on behalf of the primary care mental health service and should be read in conjunction with more detailed role specific local working instructions.
For further information about responsibilities, accountabilities and duties of all employees, please see appendix A.
5 Procedure
5.1 Quick guide
5.1.1 Entry and primary care
- Patients contact GP surgery for support with their mental health or co-morbid presentation.
- Care navigators and reception within GP surgeries direct patients to the mental health practitioners (MHP) or mental health wellbeing triage coach (MHWBTC) where in place.
- Patients in crisis should not be booked in with the MHWBTC or MHPs. Traditional referral routes should be followed for people in crisis.
- Referrals into the PCMHH can also come from single point of access (SPA), where in place, social care, local authority, prison and other third sector partners.
5.1.2 Primary care network mental health practitioner first contact
- Care navigator will book patients seeking support with their mental health with the MHWBTC (where applicable) or the MHP where triage is not in place.
- Ardens dialog template to be completed and read code “XaL0u” entered for first contact.
- PHQ and GAD completed as appropriate.
- signpost to appropriate support and refer or book for further brief interventions with MHP.
- Patient to be stepped out of PCMHS, if no further support is required by the MHP.
5.1.3 Primary care network mental health practitioner intervention
- Up to 4 sessions of brief interventions can be provided with the mental health practitioner.
- Ensure dialog and Dialog+ be undertaken on the primary care SystmOne or EMIS unit.
- Read code “XaZrH” to be entered for patients follow-up contact.
- Patient to be stepped out of PCMHS, if no further support is required by the mental health practitioner.
- if further support is required, then patients can be stepped up to the PCMHS or Talking Therapies via agreed referral route.
- Referral to specialist mental health services can also be made where deemed appropriate via agreed referral route.
5.1.4 Step up to primary care mental health hub
- Only routine referrals go to the PCMHH, admin to register patient on SystmOne if not already registered.
- DialOG and Dialog+ to be completed.
- If deemed appropriate discuss referrals and decisions made at Multidisciplinary team (MDT) meeting.
- Step patient into appropriate intervention and pathway, if suitable for PCMHH and allocate to relevant caseload.
- Read code “XaZrH” to be entered for patients follow-up contact.
- Update recovery plan and safety plans, and as required complete goals based outcomes and ReQoL-10.
- Complete dialog (Dialog+) once interventions complete and then discuss at MDT, if deemed appropriate.
- Step patient out of PMCHS, if no further intervention required or step up to specialist mental health services.
5.1.5 Specialist mental health
- If deemed appropriate discuss at MDT when someone is identified as requiring more intensive support from specialist mental health services.
- Specialist Mental Health team representatives to be part of the MDT and decision-making.
- Referral required to step up patients care to the Specialist Mental Health team. Assessment to be completed as agreed in each locality.
- Interventions and support undertaken.
- Complete Dialog, Dialog+ along with either or both goals based outcomes and ReQoL-10 before, during and after interventions.
- Following intervention, navigate care as appropriate, for example step down to PCMHS, if requiring low moderate level support or step out to primary care if no further intervention is required.
6 Safe operating standards
Safe operating standards include:
- operating days and times
- minimum staffing levels
- on call or duty manager provision of advice and support
Please refer to your local working instruction for details on the safe operating standards within your locality.
7 Roles and multidisciplinary team
The primary care mental health multidisciplinary team (MDT) contains a range of colleague disciplines who act as an integrated team to meet the SMI and complex needs of the population of the PCN. Every member of the MDT is pivotal in providing the care, support, and treatment interventions within the integrated team.
MDT roles are listed in appendix A and are not exhaustive. It is important to note that the roles in place and taking part in an MDT may differ between localities.
8 Referral
There are two main referral routes into the PCMHS and these reflect the development of “step-up” and “step-out” pathways rather than referral and discharge.
For patients with mental health related concerns GP’s can directly step them across to the MHPs, or MHWBTC where they are in place, or as locally agreed. GPs can also discuss the best pathway with a clinical member of the PCMHS.
First contact patients will be booked into appointment slots via the care navigators within GP surgeries. Patients who have a degree of complexity or comorbidity that require a more detailed assessment of their mental health needs, can then be booked to see the MHP either via the MHWBTC, the care navigator or GP themselves. This differs between GP surgeries, so please check your local working processes. The MHP will manage any follow-up appointments.
Should a patient require stepping up from the GP or MHP to the PCMHH, all routine referrals can be sent by email or e-referral (where in place).
Traditional referral routes will remain for GP’s or others to refer complex cases including requests for urgent or crisis interventions where a degree of risk to self or others is present.
8.1 Step up and step out or down
As deemed appropriate a regular MDT will be held within the PCMHS to discuss:
| Meaning | |
|---|---|
| Step down | Near the end of a specific intervention or period of care, a patient led review will be completed and will inform the next step when a less intensive level of care is required. |
| Step up | When a patients risk has increased, their needs intensified and, or effective engagement has reduced, which may require multiple agencies to be involved.
For example, MHP worker to PCMHH or PCMHH to specialist mental health services. Please note this only applies to routine patients, not for those requiring a crisis response. |
| Step across | This would reflect when a patient is signposted to another service.
For example, Talking Therapies to PCMHH. |
| Step out | Once a period of brief intervention has been offered the expectation is that a patient can step out of the PCMHS.
|
For patients who avoid contact with the PCMHH team, please refer to the disengagement policy.
8.2 Inclusion and exclusion
Inclusion and exclusion criteria for the PCMHS is listed below.
For inclusion and exclusion criteria specific to each area please see local working instruction. MHPs have the flexibility to work with the clinical director of their PCN to review, make slight amendments and agree.
8.2.1 Inclusion
- People over the age of 18 with a severe or complex mental health need that is impacting on their mental health and that can be met in a primary care setting.
- People wanting to engage with support for their mental health.
- People who are living within the place geographical boundary and registered with a GP within the appropriate PCN.
- People who require a routine assessment and onward referral to specialist mental health services.
8.2.2 Exclusion
- People who do not present with a severe or complex mental health issue.
- People under the age of 18.
- People in need of a crisis response.
- People whose needs can be met by the NHS Talking Therapies (previously IAPT) and any other similar commissioned provision such as IESO.
- People who require ADHD or ASD assessment.
- People whose needs are already being met by specialist mental health services.
9 Mental health practitioner and mental health wellbeing triage coach appointments
Appointments with MHPs and MHWBTC are available five days a week and include phone reviews in addition to face-to-face appointments. For PCNs with MHWBTC in place, only phone appointments are offered. Any variation from this would need to be for a specific clinical reason and as by local agreement.
Care navigators and reception colleagues within the GP surgeries have direct access to automatically book a patient into a daily triage slot.
Appointment time slots are 20 or 30 minutes, at times these slots may need to be longer for the MHPs to allow them to undertake follow-up appointments, therefore they can double book slots or alternatively split their 30 minutes into 15-minute slots. Admin time also needs to be accounted for within the working day. Table 2 below shows the break-down per MHP or MHWBTC role and the maximum capacity of appointments that could potentially be undertaken.
MHP or MHWBTC will work via the clinical system in place, be that SystmOne or EMIS.
Appointments are recorded on the shared PCN appointment ledger wherever possible.
In the absence of a shared ledger, appointments are recorded on the individual practices appointment ledgers.
The MHPs should spend 70% of their time (27 to 30 hours) delivering clinical contacts and the remaining 30% of their time offering advice, support, consultation, and the facilitation of onward access to mental and physical health, well-being, and biopsychosocial interventions. The addition of a MHWBTC to PCN’s releases clinical time from the MHP to support this.
| Role | Mental health practitioner, band 7 whole time equivalent | Mental health practitioner band 6 whole time equivalent | Mental health wellbeing triage coach, band 4 whole time equivalent |
|---|---|---|---|
| Maximum capacity | AM: Six (30 minutes appointment) PM: Six (30 minutes appointments) |
AM: Six (30 minutes appointment) PM: Six (30 minutes appointments) |
AM: Six (20 minutes appointment) PM: Six (20 minutes appointments) |
| Maximum total per day | 12 appointments (6 hours) | 12 appointments (6 hours) | 18 appointments (6 hours) |
| Referral, signposting, escalation, notes and breaks | 2 hours | 2 hours | 2 hours |
| Total per week (5-day week) | 60 appointments | 60 appointments | 90 appointments |
| Total per year, per mental health practitioner or mental health wellbeing triage coach worker (42-week period) if 100% slots utilised | 2,520 | 2,520 | 3,780 |
10 Assessment
All patients requiring a step up from a GP surgery to the PCMHH are required to be seen by a MHP, through the single point of access (SPA), where one is in place, or as agreed in each locality. Appropriate triage and documentation should be completed before patient is stepped up to the PCMHH and sent via agreed referral route (see section 8, referral).
Referrals or step-ups from other services including but not limited to the local authority, MAPPA, police and so much on, can continue to be made either through a SPA function (where one is in place), or directly into the PCMHH.
Every patient who is referred for a mental health assessment will be triaged, within 4 weeks, as agreed in each locality. If deemed appropriate an MDT decision will be made regarding the need for any further assessment to establish a treatment plan, or whether advice and guidance or signposting can be offered before stepping back to the referrer. In cases where step up to specialist mental health services is required, assessments will be completed as agreed in each locality.
Documentation and processes should be proportionate and enable the delivery of high quality care. Assessments will vary according to the needs of the individual and the complexity of their need(s). For people with less complex needs an assessment can be a relatively brief initial contact in which an understanding of the person’s current problems and a shared view of an intervention have been developed and agreed with them. The intervention itself may comprise a simple, short advice session that enables the person to obtain help for themselves, initiation of a treatment with medication and subsequent follow-up, or perhaps no further help will be required. For people with more complex needs, the assessment will be more comprehensive, and may require multidisciplinary input and interventions are also likely to be multi-professional in nature.
A single trusted assessment approach will be undertaken, resulting in a cumulative assessment that is built on throughout the patient journey, avoiding the need for patients to repeat their stories. This is an approach where assessors carry out holistic assessment of need, avoids duplication and speeds up response time so that people can be stepped up or down in a safe and timely way. For details on tools that will support this approach please see section 15, clinical documentation.
Assessments will be layered, the first layer, completed by the PCMHS, will contain sufficient detail to assess need and risk; this layer will be kept as brief as possible whilst maintaining quality and safety. If a patients need is beyond what the PCMHS can support and they require step up to specialist mental health services, then another layer of assessment will be completed to evidence the need. On accepting the patient, specialist mental health teams would undertake the next layer and more complex end of the assessment as recognised as necessary, meaning only those patients whose needs require full mental health assessments to plan their care, receive one.
If someone is in acute risk of ending their lives, a referral for crisis assessment should be made by email. Copies of email correspondence with SPA should be recorded in SystmOne or EMIS (as applicable). The email should be followed up with a call to ensure the referral has been received and actioned and document phone calls with SPA services in the SystmOne and EMIS notes.
11 Care planning
Care planning and care coordination is reframed under the community mental health transformation in order to work for everyone, it will focus on improved outcomes and deliver place based integrated mental health care to people, this will be done through moving towards a personalised care approach. The Community Mental Health Transformation Framework envisages a shift away from risk assessments and ineffective predictive approaches to safety planning and “positive risk taking”, with colleagues supported by managers and to do so under progressive, partnership clinical governance arrangements.
Assessment of risk and safety planning will form part of a wider care planning process. A personalised approach to managing risk is a key part of the personalised care and support planning process. Once risks are identified, through personalised conversations options are explored that are relevant to the individual to help mitigate the risk. Patients with certain markers of risk (for example, frequent consultations, multiple psychotropic drugs and specific drug combinations) are further assessed and considered for referral to specialist mental health services (NCISH, September 2022).
Every person who requires support, care and treatment in the community should have a co-produced and personalised care plan that takes into account all of their needs, as well as their rights under the Care Act, and section 117 of the Mental Health Act when required. The level of planning and coordination of care will vary, depending on the complexity of their needs. For people with more complex needs, who may require interventions from multiple professionals, one person will have responsibility for coordinating care and treatment. This key worker role can be provided by workers from different professional backgrounds. The care plan will include timescales for review, which should be discussed and agreed with the person and those involved in their care at the outset.
Digital technologies, such as mobile applications, may be used. However, for a significant proportion of people there will be an intervention detailed in an agreed personalised care and support plan, developed mutually (subject to the person’s capacity).
(The Community Mental Health Framework for Adults and Older Adults, September 2019).
12 Interventions
Within the PCMHS specific interventions can be provided based on identified patient needs, some of which are listed below. As this is a new and developing service, the interventions and input available will continue to evolve and may differ slightly between localities.
- psychoeducation
- formulation
- motivational interviewing
- guided self help
- mindfulness and relaxation
- social prescribing
- social work support
- medication optimisation
- emotional regulation
- basic cognitive behaviour therapy (CBT)
- advice and support
- signposting
13 Caseload management
MHP will not hold a caseload, interventions will be on an appointment basis only. Where brief interventions support is required via the MHP a maximum of 4 sessions should be delivered, anyone requiring additional sessions should be stepped up to the PCMHH.
Caseload management for the PCMHH will be monitored and managed via the SystmOne clinical system. As a new service with new roles no definitive maximum caseload has been agreed, but work is ongoing to understand what this is, as we begin to understand the model more. Caseloads should be discussed as part of clinical and management supervision.
14 Non-medical prescribing
There are a number of patient and service benefits relating to non-medical prescribing. This section applies to those who undertake non-medical prescribing as part of their role.
There will be access to non-medical prescribing within the PCMHS where applicable. Full responsibilities as set out by RDaSH can be found in the non-medical prescribing policy. In addition, roles and responsibilities for people undertaking non-medical prescribing within their role are set out in their governing bodies, code of conduct, and guidance by the Royal Pharmaceutical Society.
Involvement from the NMP (prescribing advice and guidance or intervention) will be discussed and agreed during the team MDT.
Other interventions should be considered to meet psychological, social and general holistic needs of the patient prior to an NMP review.
15 Clinical documentation
15.1 Recording interventions
All MHP and MHWBTC clinical records will be recorded in the PCN electronic patient records. The PCN will provide full access to the relevant primary care systems in line with local data sharing agreements.
Colleagues in the PCMHH will record all contacts using the appropriate SystmOne template as detailed below. For specific detail please refer to your RDaSH local working instruction.
Documentation expected to be completed within the PCMHS, including MHP or MHWBTC are:
- dialog or short triage assessment to be completed on first contact within primary care, RDaSH mental health triage (Adult) template
- PHQ and GAD where appropriate
- DIALOG+ to be completed by MHP in primary care system and if stepping up to PCMHH DIALOG+ to be completed on RDaSH SystmOne template
- for initial contact (triage or assessment) the read code “XaL0u” requires adding to template
- for follow-up contact (including, treatment) read code “XaZrH” needs adding to the template. This code can be added by the MHP based in primary care or the PCMHH team, whoever has the second contact with that patient
- care plan, DIALOG+ recovery plan and WRAP
- risk management, DIALOG+ and safety plan
- patient reported outcome measures, DIALOG, ReQoL-10 and goal based outcomes (GBO), as required
- Additional tools, CORE-10, PHQ9 and GAD7
Should a patient require stepping up to the specialist mental health services, assessments will be undertaken as agreed in each locality. As a new service, agreement on what systems and documentation will evolve.
The clinical documentation process is illustrated in the example below:
- triage:
- complete RDaSH MH triage template
- core documentation
- additional tools
- assessment:
- patient to complete DIALOG questionnaire prior to first appointment
- complete DIALOG+ assessment
- complete safety plan
- additional tools PHQ9, GAD7, CORE-10
- interventions:
- review DIALOG questionnaire
- complete recovery plan
- review safety plan
- complete ReQoL-10 and GBO
- additional tools PHQ9, GAD7, CORE-10
- step down:
- complete DIALOG questionnaire
- additional tools PHQ9, GAD7, CORE-10
Please note that MHPs will only undertake DIALOG and DIALOG+ assessments. Colleagues in the PCMHH will complete DIALOG+ assessments, the safety and recovery plans as well as any additional tools as required.
15.2 Clinical governance
The PCMHS will deliver high quality care, effectiveness and ensure safety for the patients referred into their care. The PCMHS will follow risk and incident reporting, the principle of freedom to speak for colleagues and where necessary learning from incidents, whether near misses or actual.
The care, support and interventions that are provided by the PCMHS are delivered within a primary care community setting, where patients are low to moderate risk. Therefore documentation and processes will be proportionate and enable the delivery of high quality care. Please refer to the care planning section within this policy, as well as information on moving towards personalised care approach for further detail.
The PCMHS within each locality has clear clinical leadership, but there will also be a shared model of leadership amongst the different PCNs. Please refer to your local working instruction for details of the leadership structures.
Clinical governance will be monitored through supervision arrangements, team meetings and multidisciplinary team meetings. Further monitoring is detailed within the monitoring arrangements in appendix B.
15.3 Data protection
Patient information will be used in accordance with the data protections regulations policy.
16 Safeguarding
The PCMHS works to the RDaSH safeguarding adults policy and the RDaSH safeguarding children policy and should escalate and report concerns accordingly.
Responding to safeguarding concerns:
- make an immediate evaluation of the risk and take steps to ensure that the adult or child is in no immediate danger
- where appropriate, call 999 for emergency services if there is a medical emergency, other danger to life or risk of imminent injury, or if a crime is in progress
- consider if there are other adults with care and support needs or children who are at risk of harm and take appropriate steps to safeguard them
- contact the trust safeguarding team for advice if required
- report the incident internally on the electronic reporting system
- ensure all decision-making is recorded in the electronic patient records, using the safeguarding adult or safeguarding children templates
- all safeguarding concerns must be reported to the Adult Safeguarding team in the local authority or children’s social care on the same day that the concerns were identified. Contact details can be found in the corresponding safeguarding policies
- safeguarding concerns should always be shared with a clinical lead and the practice. Patients with safeguarding concerns should be discussed at the next available MDT meeting
Colleagues are to adhere to the RDaSH lone working policy and where applicable complete lone worker risk assessments with their line manager.
17 Training implications
Training and development will reflect local and national drivers including NICE guidance, the needs of the trust or local authority and individuals who use services.
Colleagues development needs will be identified and reviewed and appraised annually in line with the trust personal development review (PDR) policy.
The trust recognises that continuing professional development is a key element of ensuring the delivery of evidence based quality services. Role development and scope of practice is also increasingly relevant to the provision of colleagues training and supervision.
All colleagues should refer to the trusts mandatory and statutory training policy.
As a new service with new roles, training in new approaches will be required as agreed by the trust. Work is ongoing, as we understand the model more.
18 Equality impact assessment screening
To access the equality impact assessment for this policy, please email rdash.equalityanddiversity@nhs.net to request the document.
18.1 Privacy, dignity and respect
The NHS Constitution states that all patients should feel that their privacy and dignity are respected while they are in hospital. High Quality Care for All (2008), Lord Darzi’s review of the NHS, identifies the need to organise care around the individual, “not just clinically but in terms of dignity and respect”.
As a consequence the trust is required to articulate its intent to deliver care with privacy and dignity that treats all service users with respect. Therefore, all procedural documents will be considered, if relevant, to reflect the requirement to treat everyone with privacy, dignity and respect, (when appropriate this should also include how same sex accommodation is provided).
18.1.1 How this will be met
All employees, contractors and partner organisations working on behalf of the trust must follow the requirements of this policy and other related policies, particularly those relating to information governance. All health employees must also meet their own professional codes of conduct in relation to confidentiality.
18.2 Mental Capacity Act (2005)
Central to any aspect of care delivered to adults and young people aged 16 years or over will be the consideration of the individuals’ capacity to participate in the decision-making process. Consequently, no intervention should be carried out without either the individual’s informed consent, or the powers included in a legal framework, or by order of the court.
Therefore, the trust is required to make sure that all staff working with individuals who use our service are familiar with the provisions within the Mental Capacity Act (2005). For this reason all procedural documents will be considered, if relevant to reflect the provisions of the Mental Capacity Act (2005) to ensure for that the rights of individual are protected and they are supported to make their own decisions where possible and that any decisions made on their behalf when they lack capacity are made in their best interests and least restrictive of their rights and freedoms.
18.2.1 How this will be met
All individuals involved in the implementation of this policy should do so in accordance with the guiding principles of the Mental Capacity Act 2005 (section 1).
19 Links to any other associated documents
The Primary Care Mental Health team (including ARRS roles) policy should be read in conjunction with related policies which include:
19.1 NHS England guidance
- NHS long term plan
- The community mental health framework for adults and older adults NHS England primary care networks
19.2 Trust policies
- Corporate and local service induction policy
- Mandatory and statutory training policy
- Non-medical prescribing policy
- Healthcare record keeping policy
- Safeguarding adults policy
- Safeguarding children’s policy
- Disengagement policy
- Data protection regulations policy
- Lone working policy
20 References
- NHS England, Community Mental Health and NHS Talking Therapies for anxiety and depression, Annexes: National guidance to support seamless and person centred access to appropriate mental health care, page 16, July 2023
- NHS long term plan
- NHS Sheffield primary and community mental health service, service operational policies (SOPs), version 1.8, September 2021
- The community mental health framework for adults and older adults, prepared by: NHS England and NHS Improvement and the National Collaborating Central for Mental Health
- The National Confidential Inquiry into Suicide and Safety in Mental Health (NCISH), Safer Services: A toolkit for specialist mental health services and primary care, University of Manchester, Healthcare Quality Improvement Partnership (HQIP)
21 Appendices
21.1 Appendix A responsibilities, accountabilities and duties
The trust has a “duty of care” and a “duty of confidentiality” to ensure that all aspects of healthcare record keeping are properly managed. The trust must adhere to the legislative, statutory, and good practice guidance requirements relating to healthcare records management.
The chief executive has overall accountability and responsibility for healthcare records within the trust. This function is delegated to the executive medical director and the executive director of nursing and allied health professionals, who are responsible for driving high quality standards of healthcare record keeping.
The trust’s executive medical director (and trust Caldicott guardian) plays a key role in ensuring that NHS and partner organisations comply with current national guidance and relevant legislation regarding the handling and safeguarding of patient identifiable information. The Caldicott guardian will advise employees on matters relating to the management of patient identifiable information, for example where issues such as the public interest conflicts with duties such as maintaining confidentiality.
Senior managers of the trust are responsible for the quality of the healthcare records that are generated by all trust employees to ensure patient safety and quality service delivery.
Head of information management and business intelligence will advise the trust on how to maintain an efficient and effective patient information system, which complies with all the data collections required within the NHS.
All RDaSH colleagues who come into contact with patients, are seen by doctors, nurses, allied health professionals, pharmacists, psychologists, bank colleagues and agency workers, students and volunteers. All are expected to ensure that each person coming into their care and their carers are treated with dignity and respect.
Members of the multidisciplinary team including external agencies, the patient and their family or carers should be aware of and involved in their care and treatment within the primary care mental health service in a timely manner.
All clinical and non-clinical colleagues involved in the care and treatment of a patient within the primary care mental health service, should ensure local and national guidance in relation to this is adhered to.
21.1.1 Multidisciplinary team roles
The roles listed below are not exhaustive and it is important to note that what roles are in place and taking part in an MDT may differ between localities and may also change as the primary care mental health service is a developing service.
21.1.1.1 Service manager, clinical lead, cognitive behaviour therapy lead
Will aim to offer within each individual PCN:
- overall clinical leadership in terms of the MDT approach and strive for clinical efficiency, effectiveness and safety for people with severe or complex mental health needs, in the primary care setting
- will be the focus for contacts with external agencies
- will offer clinical supervision and line management for some roles within the PCMHN
The clinical lead will also offer some clinical intervention according to:
- their professional background and expertise
- coordinate between the PCN’s
- ensuring there is service consistency
- sharing clinical expertise across the whole network
21.1.1.2 Mental health practitioners
Mental health practitioners (MHP) are clinically registered practitioners, mental health nurses, mental health social workers or allied health professionals. The team will work alongside PCN colleagues (with the population needs of the PCN determining exact skill mix) to meet the needs of those with serious mental illness in line with the new mental health framework. The role of the MHP is a more specialist role than triage or gatekeeping. Depending on population needs and expertise they may directly undertake non-medical prescribing, social work interventions or evidence based psychosocial interventions in conjunction with other team members (NHS Sheffield, September 2021).
These roles should support people with complex mental health needs, rather than people for whom NHS Talking Therapies provision would be suitable. MHP or MHWBTC should not be treating cases of anxiety or depression, which are more appropriately seen in NHS Talking Therapies (NHSE, 2023).
MHPs will be employed by RDaSH but be fully embedded into the PCNs via a service agreement. This arrangement will maximise the opportunity to integrate two different organisations and working cultures, in an area where seamless transfers of patient care are particularly critical.
A PCN must comply with the following requirements:
- the roles must be embedded within the PCN’s core network practices and be fully integrated within the multi-disciplinary team delivering healthcare services to patients
- have access to other healthcare professionals, electronic ‘live’ and paper-based record systems of the PCN’s core network practices, as well as access to admin or office support and training and development as appropriate
- have access to appropriate clinical supervision and administrative support
21.1.1.3 Mental health and wellbeing triage coaches (MHWBTC)
Some PCN’s may have MHWBTC attached to them. The role of the MHWBTC is to work closely between the PCMHS, social prescribing and the mental health practitioners (MHP) to identify low and moderate support needs and signpost or coordinate the most appropriate route of care including Talking Therapies (formerly IAPT) and the VCSE. People who present as needing more than talking therapies will be moved into an appointment with the MHP and an appropriate route of treatment and support will be identified including medicines management and escalations into the PCMHH.
The MHWBTC would support anyone of working age presenting with a mental health need, they would not be expected to support anyone, in crisis, aged under 18, already under secondary or acute mental health services, with an eating disorder, with ADHD or open to child adolescent mental health service (CAMHS).
21.1.1.4 Mental health nurse
A mental health nurse working within the PCMHS is instrumental in promoting and delivering evidence-based care for service users with mental health conditions within primary care. They will independently carry out assessments as trusted assessors and care plan interventions. Where appropriate, following assessment and formulation, liaise and signpost to teams within the community including social care and the voluntary sector, Community Mental Health teams and addictions services.
21.1.1.5 Mental health social worker
The social worker will provide social work service in the primary care community setting, offer interventions including:
- person led assessments
- risk assessment (within the context of primary care)
- support social care planning
- promote service user recovery
- promote social inclusion
21.1.1.6 Non-medical prescribers (NMP)
Any prescribing completed by a healthcare professional other than a doctor or dentist. Clinician with non-medical prescribing skills will be registered with the trust to prescribe and will be included on the RDaSH NMP database, have their own NMP folder and will adhere to the trust NMP policy.
Full details on responsibilities and accountabilities can be found within the non-medical prescribers (NMP) policy
21.1.1.7 Clinical psychologist and psychotherapist
The Clinical Psychology team work with people on a wide range of psychological difficulties in mental and physical health. They bring enhanced skills of being able to provide formulation, review and interventions to support complex needs such as characteristics of personality disorder, complex cases and trauma informed practice.
21.1.1.8 Clinical associate psychologist (CAP)
The clinical associate psychologist (CAP) work under the supervision of clinical psychologists and can provide support for complex stable individuals or those with intermediate level needs; presentations they support include anxiety, depression, personality disorder, post traumatic stress disorder (PTSD) and complex PTSD. CAPs are trained in assessment, formulation and intervention, which they deliver one to one with patients. CAPs will also support the development of group work activities as part of a range of interventions as well as support teams in a psychological way using their skills to offer a safe and supportive reflective space and helping the team think more psychologically.
21.1.1.9 Mental health wellbeing practitioner (MHWP)
The main responsibilities of mental health wellbeing practitioners (MHWP) are to deliver evidenced based psychologically informed interventions to people with moderate to severe mental health problems and help support adults to receive the right care. The MHWP roles offer wellbeing focused psychologically informed interventions for serious mental health problems for adults individually and in groups, as well as support their families and carers.
21.1.1.10 Occupational therapist
The occupational therapists support a patients’ recovery, helping those who have difficulties carrying out day-to-day activities due to disability, illness, trauma, ageing and a range of long term conditions. The occupational therapist will consider all of the patient’s needs, physical, psychological, social and environmental.
21.1.1.11 Peer support worker
Peer support workers are people who use their lived experience of mental health challenges to support others, they can help a person to maintain their ongoing community needs and engagement beyond formal clinical treatment to support their wellbeing and provide inspiration for their recovery. Peer support workers may be employed directly by RDaSH or hosted within VCSE organisations given their strength and placement to local communities. These roles are of significant benefit to supporting the service to engage with, learn from and to adapt how services are provided. Peer support workers do not provide clinical care.
21.1.1.12 Community connector, social prescriber and link worker community connectors
Community connector, social prescriber, link worker community connectors may be employed by the local authority, primary care or our VCSE partners and link between services. Community connectors can advise on the local offer of VCSE support available in each PCN, they play a key role by giving people time, focusing on ‘what matters to me’ and taking a holistic approach to people’s health and wellbeing in order to connect them to appropriate community groups and services. Depending on a person’s need a community connector may only need to provide advice and signposting, whilst others may require a short term package of support to help their social needs, such as social activities, debt, housing, education, training, employment, or family support.
21.2 Appendix B monitoring arrangements
21.2.1 Compliance with the policy
- How: Through discussion during supervision at team meetings.
- Who by: Team managers.
- Reported to: Exception reported to care group leadership meetings.
- Frequency: As required.
21.2.2 Patient experience, complaints
- How: Review of complaints.
- Who by: Patient Safety and Investigations team
- Reported to: Care groups.
- Frequency: Monthly.
21.2.3 Patient experience, your opinion counts
- How: Review of your opinion counts forms.
- Who by: Service managers.
- Reported to: Care groups.
- Frequency: Monthly.
21.2.4 Improved access to services
- How: Adherence to the access and waiting times standards from initial contact with any primary, secondary care or other service to appropriate mental health care, for patients who need further support after initial contact.
- Who by: This would be recorded in the electronic patient record by colleagues seeing patients within the primary care mental health service. Report would be compiled by the Performance team for organisational monitoring. This data also flows into the MHSDS for national monitoring.
- Reported to: Care group performance meetings.
- Frequency: Monthly.
21.2.5 Improved access to services
- How: Expanding patient access by 5% each year in all transformed and non-transformed community mental health teams. Referrals and contacts recorded.
- Who by: Recorded by colleagues working in the primary care mental health service and specialist community mental health teams in the electronic patient record. Report would be compiled by the Performance team for organisational monitoring. This data also flows into the MHSDS for national monitoring.
- Reported to: Care group quality meetings by performance.
- Frequency: Monthly.
21.3 Appendix C community mental health model
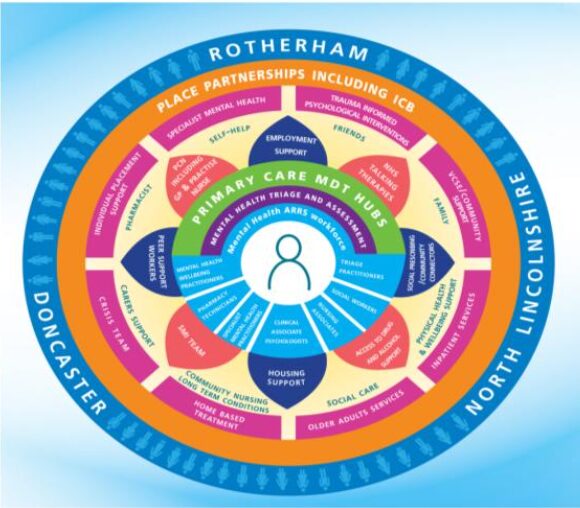
21.3.1 Rotherham, Doncaster, and North Lincolnshire
Place partnerships including integrated care board (ICB):
- specialist mental health (self-help)
- trauma informed psychological interventions (friends)
- voluntary, community and social enterprise (VCSE) or community support (family)
- inpatient services (physical health and wellbeing support)
- older adults services (social care)
- home based treatment (community nursing long term conditions)
- crisis team (crisis support)
- individual placement support (pharmacist)
These encompass:
- employment support
- NHS Talking Therapies
- social prescribing or community connectors
- access to drug and alcohol support
- housing support
- SM team
- peer support workers
- primary care networks including GP and practice nurses
21.3.1.1 Primary care multidisciplinary team hubs
21.3.1.1.1 Mental health triage and assessment
Mental health additional roles reimbursement scheme (ARRS) workforce consists:
- mental health wellbeing practitioners
- pharmacy technicians
- specialist mental health practitioners
- clinical associate psychologists
- nursing associates
- social workers
- triage practitioners
21.4 Appendix D primary care networks
21.4.1 Rotherham
- Maltby Wickersley
- Central North
- Health village and Dearne valley
- Rother Valley South
- Raven
- Wentworth
21.4.2 Doncaster
- North primary care network
- South primary care network
- East primary care network
- Doncaster primary care network
- Central primary care network
21.4.3 North Lincolnshire
- West primary care network
- East primary care network
- North primary care network
- South primary care network
21.5 Appendix E abbreviations
| Term | Meaning |
|---|---|
| ARRS | Additional role reimbursement scheme |
| CAPs | Clinical associate psychology (trainee role) |
| CAMHS | Child adolescent mental health service |
| EMIS | Clinical IT system used by some GP practices |
| GP | General practitioner |
| IAPT | Improving access to psychological therapies |
| LTP | NHS long term plan |
| MDT | Multi Disciplinary team |
| MHP | Mental health practitioner |
| MHWBTC | Mental health and wellbeing triage coach |
| NHSE | NHS England improvement |
| PCMHS | Primary care mental health hub |
| PCMMH | Primary care mental health hub |
| PCN | Primary care network |
| SMI | Serious mental illness |
| SPA | Single point of access (Sheffield Health and Social Care NHS Foundation Trust) |
| SystmOne | Clinical IT system used by the service and some GP Practices in Sheffield |
| RDaSH | Rotherham, Doncaster and South Humber NHS Foundation Trust |
| VCSE | Voluntary, community and social enterprise |
Document control
- Version: 1.1.
- Unique reference number: 1072.
- ratified by: clinical policy review and approval group.
- Date ratified: 5 December 2023 (virtual approval).
- Name of originator or author: service manager, community mental health directorate (Rotherham, Doncaster and North Lincolnshire).
- Name of responsible individual: Chief operating officer.
- Date issued: 1 May 2025.
- Review date: 31 December 2024.
- Target audience: all colleagues working within the primary and community mental health service.
Page last reviewed: July 02, 2025
Next review due: July 02, 2026
Problem with this page?
Please tell us about any problems you have found with this web page.
Report a problem