1 Introduction
The searching of a person or their property should only be carried out where there is cause for concern or an identified need, for example, where dangerous or violent propensities of patients create a self-evident and pressing need for additional security. In such circumstances clinical staff have a statutory duty to provide both a safe and therapeutic living and working environment for patients and staff and to protect the public. Therefore searches are an essential and justifiable component for safe practice.
Hospital managers are required to provide an operational policy on searching patients detained under the Mental Health Act, their belongings, surroundings and their visitors and that when preparing such a policy the position of informal patients should be considered (Code of Practice Mental Health Act (2015), section 8.29).
This policy takes into account guidance issued within a number of documents, including the violence and aggression, short term management in mental health, health and community settings. (NICE, 2015) and NHS Protect. For the purpose of searching a detained patient it also follows the clear principles laid out within the Code of Practice Mental Health Act (2015), section 8.30, which are:
- to create and maintain a therapeutic environment in which treatment may take place and to ensure the security of the premises and the safety of patients, staff and the public
- the authority to conduct a search of a person or their property is controlled by law, and it is important that hospital staff are aware of whether they have legal authority to carry out any such search
- searching should be proportionate to the identified risk and should involve the minimum possible intrusion into the person’s privacy and dignity
- to undertake all searches with due regard to and respect for the patient’s dignity
2 Purpose
The purpose of this policy is to promote a safe and therapeutic environment for all patients, staff, and the public by providing clinical staff who work within in-patient services with:
- details of best practice, roles, and responsibilities in relation to the searching of a person, or property
- a framework which promotes all patients involved in any form of search being treated with respect, and having their dignity maintained throughout the process
- an awareness of the legal framework and principles that surround the searching of property or a person so that they can act accordingly
3 Scope
This policy applies to all clinical staff in in-patient services, including nurses, allied health professionals and medical staff, where there is an identified need to have assurance of security due to the behaviour of some patients.
The policy does not cover the routine checking of patient’s property on admission, which does constitute a search.
4 Responsibilities, accountabilities and duties
4.1 The board of directors
The board of directors is responsible for the implementation of this policy and the monitoring of compliance.
4.2 Care group medical directors, service managers and matrons
Care group medical directors, service managers and matrons are responsible for:
- the dissemination and effective implementation of this policy within their areas of responsibility
- facilitating effective local induction arrangements for staff within their areas of responsibility and staff attendance at any training which is identified as necessary to equip them with the knowledge and skills to effectively implement this policy
- bringing any issues which may affect the implementation of this policy to the attention of senior managers
4.3 All clinical inpatient services staff
All clinical inpatient services staff have a responsibility to:
- conduct their practice in line with this policy
- where applicable conduct their practice in accordance with the principles set out within the Mental Health Act (1983) and its Code of Practice (amended by the Mental Health Act (2015)), which are set out in section 1 above
- complete a local induction and attend any training which is provided to promote the implementation of this policy
5 Procedure
5.1 Authority to search
The legal powers for staff to search patients have not been expressly laid down in statute. However, the suggestion is that staff acting in good faith and with reasonable care are entitled to conduct searches to maintain appropriate security and prevent harm to individuals.
Within in-patient settings, NHS staff who have completed the trust approved enhanced prevention and management of violence and aggression (PMVA) training can undertake lawful searches of both patients and visitors. However, this must be an action that is both proportionate and justifiable in relation to the assessed risk.
The justification for searching will usually be the risk of harm to the individual or others, and, or reasonable grounds for suspecting criminal activity that would compromise the safety of others, for example, weapons, or a wider social problem, such as a chronic substance misuse problem in the clinical area (ACPO or NHS SMS, 2006).
If clinical staff have a reasonable belief that a patient is in possession of dangerous or restricted items such as weapons, tools, drugs, alcohol, cameras or lighters they have the authority under common law and by duty of care to take reasonable measures to prevent the patient from possessing these items. Hence, search practices constitute a reasonable preventative measure.
5.2 Decision to search
If staff suspect that a patient is in possession of a dangerous item or any item classed as restricted within the clinical area which could prove harmful to themselves or others, then a search will be undertaken. Some inpatient services have area specific standard operating procedures in place which staff can refer to for guidance as to what may constitute a restricted item in their area of work.
5.2.1 Consent
The consent of the person should always be sought before a personal search of them or a search of their possessions is attempted. If consent is given, the search should be carried out with regard to ensuring the maximum dignity and privacy of the person. Undertaking a personal search in a public area will only be justified in exceptional circumstances.
Consent obtained by means of a threat, intimidation or inducement is likely to render the search illegal.
Any person who is to be searched personally or whose possessions are to be searched should be informed that they are not obliged to consent. This does not mean that a search will or should not take place, and staff should be guided by section 5.2.4 of this policy.
5.2.2 Patients who lack capacity to consent to the search being conducted
If there are any concerns about the patient’s capacity to consent to a search being undertaken, a formal assessment of their capacity to consent will need to be completed and recorded on MCA1 in the patient’s clinical records. If the outcome of this assessment is that they lack capacity to consent, and the person is not subject to the Mental Health Act then a best interest decision under the MCA will then need to be made in respect of the search going ahead. This should follow the best interests process outlined in the trusts MCA Mental Capacity Act 2005 policy be recorded on MCA 2.
5.2.3 Consent not given, detained patients
In certain circumstances, it may be necessary to search a detained patient or their possessions without their consent.
If a detained patient refuses consent or lacks capacity to decide whether to consent to the search, their responsible clinician (or, failing that, another senior clinician with knowledge of the patient’s case) should be contacted without delay in the first instance, if practicable, so that any clinical objection to searching by force may be raised. The patient should be kept separated and under close observation, while being informed of what is happening and why, in terms appropriate to their understanding. This is particularly important for individuals who may lack capacity to decide whether to consent to the search.
In the event it is deemed necessary to use physical interventions to conduct the search due to the patient being uncooperative or attempting to prevent or deter a search, the approved practices for physical intervention must be adhered to. See reducing restrictive interventions (RRI) policy (formerly PMVA policy) for full details.
5.2.4 Consent not given, informal patients
If an informal patient does not consent to staff searching their person then the following process should be followed:
- staff request that the patient hand over any dangerous or restricted items
- if the patient refuses or denies possession of any such items and staff continue to have concerns, staff should assess the patents’ capacity to refuse consent and document the outcome appropriately
- if the patient is deemed to have capacity then the consultant in charge of the patient’s care should be contacted and a multi-disciplinary team (MDT) meeting convened to discuss the possibility of discharge and removal from the ward environment. Appropriate use of the Mental Health Act should be considered where applicable
- if discharge is not appropriate the MDT may consider increased observations, segregation or other observational approaches
- if the risk is assessed as significant and immediate, then a discussion with the police and, or a search can be carried out against their consent
5.3 Search procedure
Searches should not be delayed if there is reason to think that the person is in possession of anything that may pose an immediate risk to their own safety or that of anyone else.
Once a decision has been made to conduct a search, the suitably trained member of staff will ask the patient to hand the item(s) over to them.
If the item is handed over the following procedure must be followed:
- the patient will be reviewed by staff and offered the opportunity to discuss the incident
- the consultant in charge of the patient’s care will be informed at the earliest opportunity
- the nurse-in charge of the ward will make a decision whether they believe all items have been handed over and whether a person or room search is necessary
If the patient denies having any items in their possession:
- the patient is to be placed on one-to-one observation. see policy; supportive observation of inpatients identified as posing a significant risk to themselves or others. The nurse in charge of the ward will discuss with the matron or senior nurse (or manager on-call in the absence of the matron or senior nurse) and the consultant in charge of the patient’s care what further action needs to be taken.
Staff should not delay a search should there be reason to believe the patient is in possession of something that may pose an immediate risk to themselves or others.
Prior to conducting a search all staff involved in the search will wear personal protective equipment; including gloves, apron.
All personal searches will be conducted in a private room away from the ward communal areas.
Note, where there is a difference of opinion amongst the clinical team whether to proceed with a search the matter is to be escalated to the appropriate managers. Where further resolution is required managers should refer to the relevant associate medical or nurse director for discussion and a decision.
5.3.1 Information about the search procedure
A person being searched or whose possessions are the subject of a search should be kept informed of what is happening and why. If required and practicable the services of an interpreter should be sought. The specific needs of people with impaired hearing or a learning disability should be considered. The searching of children and young people should only be undertaken if there is significant or immediate risk. Any other decision to search a child or young person should be made by the MDT.
Staff should refer to the interpreters policy (provision, access and use of, for patients, service users and carers) for further advice.
5.4 Gender identity
The following guidance should be followed when searching a patient to ensure a person’s gender identity is acknowledged and respected and they are treated with dignity:
Sensitive enquiry should be made with the patient around their gender identity, regardless of how they present to ensure their gender identity is respected. This should include enquiry around a person’s pronouns (he or him or his, she or her or hers, they or them or their) which should then be used throughout the persons contact with the service.
If the person is unwilling to make such an election, the staff member should observe the gender the person predominantly presents as should be treated as such unless the patient requests otherwise.
As a guiding principle, staff should always address people according to the gender role in which they have described to you or, failing that the gender role in which they present. Despite possible challenges to their own beliefs and attitudes, staff should consistently maintain a professional manner in their dealing with patients who are transgender or non-binary and accord them the highest level of dignity.
This simple courtesy consistently fosters cooperation and trust. Once a person’s gender identity is known and before a person search is implemented or carried out, the searching staff member should be advised of the gender. This is important to maintain the dignity of the person being searched as well as the searching staff.
5.5 Patients who may object to a personal search being conducted on religious or cultural grounds
Any decision to undertake a personal search is done so based on the outcome of a risk assessment and genuine concerns around the safety of the patient being searched and, or others. This is to be discussed openly but sensitively with the patient, explaining that the concerns are about safety and in no way challenging or judging their religious or cultural beliefs. However whilst safety is paramount in the event of any patient objecting to a person search being undertaken on religious or cultural grounds staff should consider the following:
- the need for the search to be conducted by two staff of the same gender as the patient
- the level of agitation or distress which having the search undertaken may cause to the patient, and what action the clinical team may need to take to minimize or effectively manage this
- whether the patient would wish to speak to a religious leader or someone from their local community following completion of the search
Staff need to consider the following scenarios when conducting a search and requesting patients to remove items of clothing, as part of that search, this is to ensure a person’s religious and cultural belief are respected throughout the process:
- some Muslim men cover their heads whilst at prayer. If there are specific concerns then headwear may be searched.
- some Muslim women will choose to cover their hair and head with a scarf, usually called a Hijab and in some cases, they will choose to cover their faces with a veil, commonly known as a niqab. They must not be made to uncover their hair in public or in front of men as this could cause serious offence and distress. When required for security or identification purposes, the removal of the veil or face covering must be done in private with only female staff present. Following its removal, the person must be given the opportunity to use a mirror and to have privacy and time to put it back on.
- headscarves and veils are also used in other cultures and faith groups and must be searched with the same respect and care. For example, Orthodox Jewish men cover their heads with a skull cap (yarmulke or kippah) and orthodox Jewish married ladies cover their hair with a scarf
- some Sikh men and women will wear the Turban at all times. The turban covers the hair on the head completely with the tops of the ears customarily under the turban. Great care and sensitivity should be taken when searching a turban. Some Sikh may wish to wear a pathka, a piece of material used to tie around the head. The pathka must be treated in the same way as a turban.
- Rastafari Heritage encourages and promotes the use of traditional and spiritual headwear. Respect must be shown if it is considered necessary to search dreadlocks or headwear
5.6 Non-intimate person search (with patients consent)
A personal search should be carried out by a member of the same-sex unless necessity dictates otherwise. The search should be carried out in a way that maintains the person’s privacy and dignity and respects issues of gender, culture, and faith. There should always be a minimum of 2 clinical staff, one must be a registered nurse, present at all times during a search if it is not possible to conduct a same-sex search.
The patient will be escorted either to their own room, seclusion room or a private area by 2 clinical staff members one of whom must be a registered nurse and one of the same gender as the patient.
A full search of the patient will be conducted by staff using the metal detector and pat down technique. If necessary, staff can ask that the patient opens their mouth to allow a visual check. Any dangerous items, drugs or alcohol will be removed and disposed of. However, staff need to be aware that the metal detector will not pick up hypodermic needles.
The outcome of the search will be fully documented in the patient clinical records and reported to the Consultant in charge of the patients care, who will decide if further action is necessary.
5.7 Non-intimate person search (without patient consent)
If a search is considered necessary, despite the patient’s objections, and there is no clinical objection to one being conducted, the search should be carried out. If force must be used, it should be the minimum necessary.
The patient will be escorted to their own room, seclusion room or a private area (whichever is thought the most appropriate by the nurse in charge) by at a minimum of 2 clinical staff members one of whom must be a registered nurse and one of the same gender as the patient.
Opportunity should be given to the patient to produce any hidden items voluntarily.
If they still refuse, the nurse in charge will inform the patient that they feel a person search is necessary and again seek the patient’s consent.
- If consent is still not given, the search will be carried out in accordance with the procedures set out in the policy, prevention and management of violence and aggression policy for full details.
- A full search of the patient will be conducted by staff using the metal detector and pat down technique. If necessary, staff can ask that the patient opens their mouth to allow a visual check. Any dangerous or banned items, drugs or alcohol are to be removed.
The outcome of the search will be fully documented in the patient records and reported to the consultant in charge of the patient’s care who will then decide if further action is necessary.
Note, if it is thought that the patient has in their possession a weapon of some sort, it may be necessary for the police to be informed and for them to complete the person search.
When a person is arrested other than at a police station, a police officer may search that person under section 32(1) of police and Criminal Evidence Act (1984) (PACE) if they have reasonable grounds for believing that they may present a danger to themselves or any other person. Under section 32(8) of PACE, a police officer may seize and retain anything found if there are reasonable grounds to believe that the person may use it to cause physical injury to themselves or others. Reasonable force can be used if necessary.
Where a patient physically resists being personally searched, physical intervention should normally only proceed on the basis of a multi-disciplinary assessment, unless it is urgently required. A post-incident review should follow every search undertaken where consent has been withheld.
5.8 Room search (with or without patient consent)
Each patient should be searched before the room search is carried out. They should be given the opportunity to surrender any items of risk or contraband. They should also be asked to remove any religious items and, or items of value to them. These items should be searched after searching the person but before searching the room. The patient should then be handed the items back after they have been searched for the patient to keep them safe.
The search will be completed by at least 2 members of clinical staff, one of whom must be a registered nurse and one of the same gender as the patient. The registered nurse will be responsible for leading the room search.
Staff are to wear gloves and aprons whilst carrying out the room search and the search metal detector can be used prior to any hand searching being undertaken.
The room search is to be carried out in a systematic fashion for example by starting at the right- or left-hand side of the room.
The leading staff member will commence the room search with the second staff member following and searching the exact same area as the lead person. This system ensures that nothing is missed (therefore, staff are following each other around the room and not searching separate areas).
The search must be thorough for example, search from top to bottom. Ensuring that on top of wardrobes or shelving etc. are searched as well as drawers, cupboards, under beds, baggage etc.
Wards should also consider the use of mirror equipment for the searching of hard to access areas.
All items in the room will be replaced as originally found, except any dangerous or banned items, drugs, or alcohol, which will be removed and disposed of.
The outcome of the room search will be documented in the patient records and conveyed to the consultant in charge of the patients care, who will decide if further action is necessary.
5.9 Types of searches
5.9.1 Quadrant pat down
This procedure involves gloved hands patting and searching through clothing, feeling for abnormal shapes and textures which may indicate an illicit object under their clothing.
The person conducting the search must be the same gender as the individual being searched. The second staff will ideally also be the same gender. One of the 2 staff present must be a registered nurse. However due regard must be given to the sexual orientation of the patient and if this is an issue then the patient may have a choice of the gender of clinical staff carrying out the search. The role of the second staff member is to observe the procedure and communicate with the patient.
The patient is to be asked if they have anything on them which they are not permitted to have, and if yes then these items should be placed on a table or in a box, as it could potentially be an item that could cause harm or be of interests to the police.
The patient is to then be asked to empty out their pockets and remove any coats or shoes they are wearing which will be searched by staff. These items should be placed on a table or box and staff will search these items after they have conducted the person search. Items such as wallets or purses should only be handled by the patient. Staff should ask the patient to open and show staff what is inside the searched item. This removes the potential of allegations being made.
Patient will then be asked to stand with their feet shoulder width apart and feet pointing out and their arms up with palms showing to the sky (this disengages muscle groups keeping staff safer).
A quadrant search includes both the front and rear of the patient and the staff member conducting the search should start by standing at the right-hand side of the patient (facing in the same direction). If necessary, the patients’ interlinked hands can be held during the search.
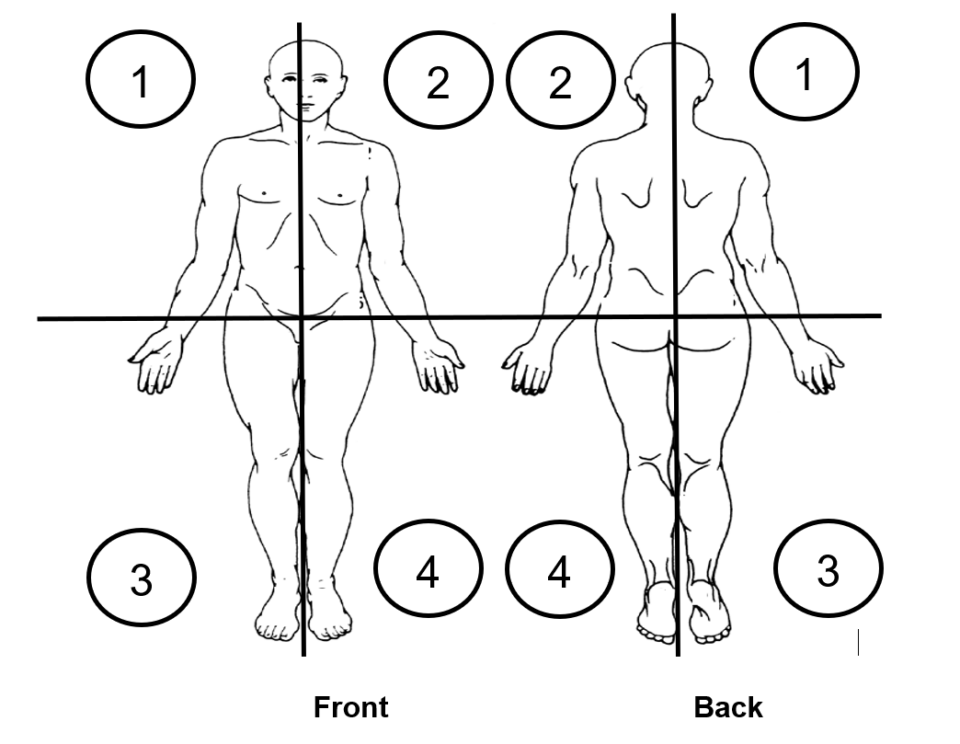
Facing the front of a person body search quadrants as follows:
- upper left, 1
- upper right, 2
- lower left, 3
- lower right 4
Facing the back of a person body search quadrants as follows:
- upper left, 2
- upper right, 1
- lower left, 4
- lower right 3
The staff member conducting the search will start with quadrant one and the quadrant searches must overlap slightly into the adjacent quadrants.
To conduct a search the front of the hand is more effective as we feel with our fingertips. Areas such as the groin and chest should be searched using the back of the hand to maintain dignity. The patient will be asked to:
- remove headwear, scarfs, ties.
- shake their hair out or run their own hands through their own hair
- pull over their own waist band over their own trousers.
- fold the bottom of their trousers up over them self’s
- lift their collar up
Once this is completed the person is to be searched in systematic manner covering all 4 quadrants front and back with a metal detector.
Once the search with a metal detector is complete staff will use their gloved hands.
The staff member then moves onto quadrant two and is to kneel onto their outside leg with their inside leg up the side of the patients leg or knee (this will allow the staff member to control the patients balance in the event of them becoming agitated).
Quadrant three and four is then to be searched as follows:
- pull over the waist band of the patients’ trousers or skirts to visibly see if any items are there before checking with hands
- if pockets have not already been emptied voluntarily pull out the pockets to check for contents. (do not immerse hand into pocket)
- pat down the outside of the leg and sock area. (if necessary shoes can be removed at this point)
- ask patient to slightly part their legs and search their inner leg (do not touch genital area)
- once inner leg search has been completed ask the patient to return their legs or feet together
- once the entire right-hand side (quadrants one and two) have been searched (front and rear) the process is to be repeated on the left-hand side of the patient
- when changing sides the staff member is to do so from behind and not cross in front of the patient
- in the case of any patient who is confined to a wheelchair or is unable to stand for any period of time staff will need to adapt the quadrant search accordingly
- the genital areas and breasts are to be avoided unless there is strong suspicion that these areas are being used to conceal items. In the case of strong suspicion, consider the body search (level 1 or 2) rather than a pat down of these areas
- this search may also include the use of the metal detector
5.9.2 Body search level 1
- This is the quadrant pat down procedure as detailed above extended to include removal and search of clothing, excluding underwear.
- A visual examination of the underarms and uncovered skin is carried out.
- There will be two clinical staff members present for this search, at least one registered nurse and both staff will be the same gender as the patient. However regard must be given to the sexual orientation of the patient and if this is an issue then the patient may have a choice of the gender of nurses carrying out the search.
- This means it may require cooperation between wards to ensure sufficient nurses or clinical staff of the same gender.
5.9.3 Body search level 2
- This is level 1 search extended to include a complete strip and visual examination of the buttock cleft, groin, under breasts and other visible skin folds.
- There will be two clinical staff members present for this search, at least one registered nurse and both clinical staff will be the same gender as the patient. However regard must be given to the sexual orientation of the patient and if this is an issue then the patient may have a choice of the gender of staff carrying out the search.
- Cooperation will be required between wards to allow for the availability of sufficient nurses or clinical staff of the same gender.
It is expected that the undertaking of a level 1 or 2 search will be extremely infrequent and in all cases must be preceded by a multi-disciplinary discussion and decision, including medical staff.
There should be support for patients and for staff who are affected by the process of searching. This may be particularly necessary where a personal search has had to proceed without consent or has involved physical intervention.
5.10 Floor restraint searching
This method of searching should only be used in exceptional circumstances such as prior to the seclusion of a patient and will only be conducted after the patients early warning scores (EWS) have been completed, and the patient is in the SUPINE (face up) position.
Once the patient is in SUPINE restraint the lead person will ask the patient if they have any items on their person that are illegal, dangerous or restricted. The patient should then be informed that they will be searched.
A staff member of the same gender as the patient, in the presence of the nurse accountable for the search, will then begin the search. Initially using the metal detector.
The search will be conducted in a systematic or logical order, for example, starting at the head and working down one side, and all areas such as pockets, collars, cuffs, hair, waistbands, socks and shoes etc. are to be searched. Once the search has been competed on one side the staff member conducting the search will move to the other side of the patient, and the staff who are undertaking the restraint will be required to adjust their position to allow easy access to the patient for the search to be completed. Wherever possible the staff member conducting the search is to avoid leaning over the patient to search their other side as this can be intimidating for the patient.
Staff are not to put their hands into any pockets and should use equipment such as tongs to pull anything out.
If the search is being undertaken prior to seclusion the patients’ shoes, socks, belts etc. are to be removed as per the procedure identified in the secluded or segregated policy management of a secluded or segregated patient.
Once the metal detector search has been completed a ’pat down’ search should be conducted over the same areas previously searched in order to pick up on anything that is not metal and so overlooked in the previous search.
Staff are to use the front of the hand as this is more effective; areas such as the groin and chest should be searched using the back of the hand to maintain dignity.
Throughout the search the lead nurse should be constantly reassuring patient and keeping them informed as to what is happening and why.
Once the SUPINE search has been completed (this can take as long as it needs to take, do not rush it as both patient and staff should be safe and secure in this position), the clinical team can consider if a search of the back of the patient is required.
5.10.1 Action if a search of the patients back is felt necessary
The patient should not be turned to a prone position to conduct a search of their back. The restraint team should turn the patient onto their side to conduct a search of their back (the restraint can still be maintained during this time). The patient can then be turned onto their opposite side if required to ensure that a thorough search is undertaken.
Once the patient is on their side a full metal detector search can be completed of their back (this may require adjustments from the restraint team) followed by a pat down search.
It is important that during the search staff are mindful of the physical monitoring (EWS) of the patient (as per policy), and if necessary, the search can be halted in order to complete this.
5.11 Documentation
A comprehensive record of every search, including the reasons for it and details of any consequent risk assessment, should be made.
In all cases the following action must be taken by the nurse accountable for the search, as soon as possible after the search has taken place, and before the end of their period of duty:
- complete and submit an electronic incident form (IR1)
- complete the record for when a search is carried out (see appendix A) and file in the patients clinical records
- make an entry regarding the incident on the ward report or equivalent
- explain to the patient that any illicit or dangerous items will be disposed of and not returned to them on discharge
- for any other items removed the patient’s money and property procedures must be followed
Where a patient’s belongings are removed during a search, the patient should be told why they have been removed, given a receipt for them, told where the items will be stored, and when they will be returned. This will be recorded in the electronic patient record.
- The nurse in charge will decide the level of observation the patient will require and record this in the clinical record.
- The patient’s risk assessment and care plan will be amended accordingly.
- Inform the patient of the listening and responding to concerns and complaints policy (formally complaints handling policy) should they continue to be unhappy with the procedure.
5.12 Action to be taken if a visitor is suspected of possessing a dangerous item, drugs or alcohol
The nurse in charge will discuss staff suspicions with the person concerned, explaining why the items are not allowed onto the ward and ask them to hand in anything they may have on them.
If they deny having anything on them, the nurse in charge will ask the person concerned if they will consent to having their baggage and person searched.
If they agree, staff will continue as for person search, informing the person that any illicit or dangerous items will be removed, disposed of and not returned to them. Any other items will be removed, a receipt issued and retained until the visitor leaves.
If the person refuses to have baggage and person searched, staff will deny them access to the ward and ask them to leave, explaining their reasons.
The patient they had come to visit will be informed why the person was not allowed access to the ward.
An electronic incident form (IR1) will be submitted.
The record for when a search is carried out is to be completed (see appendix A) and filed in the clinical records of the patient who was being visited.
The incident will be documented on the ward report and the matron or senior nurse notified.
The senior medical staff of the patient whom the person had come to visit will be informed. A decision will then be taken whether the visitor may visit the patient, this will be a multi-professional decision lead by the nurse in charge of the ward or matron along with the consultant. Due regard when making the decision must be given to the maintenance of a safe environment for all patients and staff. The decision will be fully documented within the clinical records and will also have a process for review included.
Inform the visitor of the listening and responding to concerns and complaints policy (formally complaints handling policy).
5.13 Disposal of dangerous and illicit items
If the search uncovers items that are considered as potential criminal activities or where a need arises to preserve evidence then the items should be:
- stored in clear bags that are sealed with the following information on:
- date and time
- location of find
- ideally a picture of the item and where it was found
- statement made by the person finding the item
- Items preserved as evidence must be stored in a secure location for example, a ward safe or lockable medicine cupboard
- Handled as little as possible to preserve and avoid the contamination of any evidence
The police are to be contacted and the local security management specialist (LSMS) informed.
Further advice on how to preserve evidence will be given by the police and or the LSMS.
5.13.1 Alcohol removed from the patient
This will be disposed of by 2 staff members with the patient present, if they wish. The alcohol will be poured down the sink and the bottles or cans safely disposed of. A record is to be made in the clinical records indicating what was disposed of and by whom.
5.13.2 Prescription or over the counter drugs removed from patients
Any medicines brought into hospital by a patient remain their property and will not normally be destroyed or otherwise disposed of without their agreement.
In the event that the patient is unable to consent to the disposal or not of these medicines agreement can be sought from their carer.
If the patient or carer refuses to agree to the disposal of the medicines they can either:
- be held in a sealed bag in a separate section of the medicines cupboard from all other stock until they can be returned to the patient on discharge
Or if the patient insists:
- be returned home
However, the patient and or their carer must be advised that as the treatment regime will be reviewed whilst the patient is on the ward it is likely that the supplied discharge medication will be different, and that this may pose a real risk that the wrong medication may be taken in future.
If there are safety concerns in relation to the medication being returned home, the nurse in charge in consultation with the consultant in charge of patients care may make a decision to refuse to return the medicines and have them destroyed.
For the safe disposal of any medicines, staff should refer to the guidelines issued by their supplying pharmacy.
All actions taken should be fully documented within the patient’s clinical record.
5.13.3 Suspected illegal drugs
The trust does not condone the use of illicit substances and in accordance with its duties under the Misuse of Drugs Act (Home Office 1971) will not knowingly permit the use of or dealing in illicit substances on its premises.
If any visitors are seen to be in possession of a suspected illicit substance, they will be asked to leave the premises.
If any visitor is seen or suspected to have passed illicit substances to a patient or other visitor, they will be asked to leave. The nurse in charge of the ward will then consult with the matron about the need to report the matter to the police and consider the appropriateness of further visits by this person in line with visiting patients on inpatient areas policy.
If it is a patient who is suspected to have illicit substances on their person or in their room or belongings, the nurse in charge of the ward will discuss their suspicions with them and ask that they voluntarily hand over the substance for destruction.
This discussion must be held in the company of another staff member who will act as witness to the handing over and disposal of the suspected illegal drug.
The illicit substance will be:
- placed in an envelope
- an entry will be made in the controlled drug register under the heading of unidentified substance
- the envelope will be labelled with a reference number linking it to the entry in the controlled drugs register
- the envelope will be sealed. Both the nurse in charge and the witnessing staff member will sign and date across the sealed flap of the envelope
- this envelope will then be locked in the ward-controlled drug cupboard
- to maintain patient confidentiality their name will not be documented in the controlled drug register
- the chief pharmacist, accountable officer for controlled drugs should be notified of the unknown or illicit substance as soon as it is practicable, and arrangements will be made for the removal and safe disposal of the substance by the trust pharmacy department
- if staff involved in the removal of illicit substances from a patient have reason to suspect that the quantity involved is greater than for personal use advice should be sought from the modern matron regarding the need for the matter to be reported to the police
Note, under no circumstances will any suspected illicit substances be returned to the patient.
If the patient refuses to hand over the illicit substance for destruction they are to be placed on 1-to-1 nursing observation and the need for further action, including searching will be discussed with the modern matron and the patient’s consultant.
All actions taken will be recorded in the patient’s clinical record, or in the case of a visitor, on the ward report.
An electronic incident form (IR1) will be completed and submitted for all incidents.
5.13.4 Weapons
Small sharps can be disposed of in the ward sharps bins, but with regard to any guns, hunting knives or other items that staff are unsure about, the police should be notified, who will collect and dispose of the item. An entry will be made in the patient’s clinical record indicating what was disposed of, when and by whom.
Note, under no circumstances will illicit or dangerous items be stored and returned. Nor will anyone be compensated for the loss of such items.
6 Training implications
The Mental Health Act Code of Practice 2015 requires that staff involved in undertaking searches should receive appropriate instruction and refresher training which within the trust will be provided at induction and as part of the ongoing enhanced prevention, management of violence and aggression training.
As a trust policy, all staff need to be aware of the key points that the policy covers. Staff can be made aware through a variety of means such as:
- all user emails for urgent messages
- one to one meetings or supervision
- continuous professional development sessions
- posters
- daily email (sent Monday to Friday)
- practice development days
- group supervision
- special meetings
- intranet team meetings
- local induction
7 Monitoring arrangements
7.1 Analysis of search incidents reported and actions taken or learning from incident reports
- Who by: Analysis of search incidents reported and actions taken or learning from incident reports
- Frequency: Analysis of search incidents reported and actions taken or learning from incident reports.
7.2 Review of any complaints received which relate to the implementation of this policy or procedure
- How: Complaints report.
- Who by: Complaints.
- Reported to: Review of any complaints received which relate to the implementation of this policy or procedure.
- Frequency: Complaints report.
8 Equality impact assessment screening
To access the equality impact assessment for this policy, please email rdash.equalityanddiversity@nhs.net to request the document.
8.1 Privacy, dignity and respect
The NHS Constitution states that all patients should feel that their privacy and dignity are respected while they are in hospital. High Quality Care for All (2008), Lord Darzi’s review of the NHS, identifies the need to organise care around the individual, “not just clinically but in terms of dignity and respect”.
As a consequence the trust is required to articulate its intent to deliver care with privacy and dignity that treats all service users with respect. Therefore, all procedural documents will be considered, if relevant, to reflect the requirement to treat everyone with privacy, dignity and respect, (when appropriate this should also include how same-sex accommodation is provided).
8.1.1 How this will be met
There is no requirement for additional consideration to be given with regard to privacy, dignity or respect other than previously identified.
8.2 Mental Capacity Act (2005)
Central to any aspect of care delivered to adults and young people aged 16 years or over will be the consideration of the individuals’ capacity to participate in the decision-making process. Consequently, no intervention should be carried out without either the individual’s informed consent, or the powers included in a legal framework, or by order of the court.
Therefore, the trust is required to make sure that all staff working with individuals who use our service are familiar with the provisions within the Mental Capacity Act (2005). For this reason all procedural documents will be considered, if relevant to reflect the provisions of the Mental Capacity Act (2005) to ensure that the rights of individual are protected and they are supported to make their own decisions where possible and that any decisions made on their behalf when they lack capacity are made in their best interests and least restrictive of their rights and freedoms.
8.2.1 How this will be met
All individuals involved in the implementation of this policy should do so in accordance with the guiding principles of the Mental Capacity Act (2005) (section 1).
9 Links to any other associated documents
- Chaperoning policy
- Listening and responding to concerns and complaints policy (formally complaints handling policy)
- Patients missing or absent without leave (AWOL) policy
- Reducing restrictive interventions (RRI) policy (formerly PMVA policy)
- Interpreters policy (provision, access and use of, for patients, service users and carers)
- Supportive therapeutic observation policy
- Prevent strategy policy
- Clinical risk assessment and management policy
- Drug misuse on trust premises policy
- Patients’ monies and property procedure
- MCA Mental Capacity Act 2005 policy
10 References
- ACPO or NHS SMS, (2006) Association of Chief police officers in prevention, detection and investigation work and application of sanctions in respect of security matters within the NHS.
- Department of Health (2015) Code of Practice Mental Health Act (1983)
- NICE (2015) violence and aggression: Short term management in Mental Health, Health and Community settings
- Health and Safety at Work Act 1974 (HASAWA)
- Home Office (1971) Misuse of Drugs Act, The Stationary Office
- PACE (1986)
11 Appendices
11.1 Appendix A record of when a search of a person or their property is undertaken
Refer to appendix A: record of when a search of a person or their property is undertaken (staff access only).
Document control
- Version: 7.3.
- Unique reference number: 405.
- Approved by: Clinical effectiveness meeting.
- Date approved: 13 May 2025.
- Name of originator or author: Freedom to speak up guardian
- Name of responsible individual: Chief nursing officer.
- Date issued: 23 June 2025
- Review date: 31 December 2025.
- Target audience: Inpatient clinical staff.
Page last reviewed: June 25, 2025
Next review due: June 25, 2026
Problem with this page?
Please tell us about any problems you have found with this web page.