1 Introduction
The Rotherham, Doncaster and South Humber Trust (RDaSH), (the trust) aims to provide high quality, safe and effective services to all patients and recognises the importance of enabling effective continuity of care, particularly at times of transition when patients may be particularly vulnerable.
The transition from child to adult services can be a difficult time for young people. During this time there may be many other changes in a young person’s life, including changes from school to further or higher education or employment; changes in self-identity and relationships; and changes which arise from the shift from childhood to adulthood, all of such can result in uncertainty, anxiety and stress.
It is important that any required transition process is managed sensitively and collaboratively to support continued engagement of the young person and their parents or carers and safe and effective service delivery.
The involvement of the young person and their carers, collaborative working and effective communication between everyone involved is central to successful transition arrangements.
Children and young people’s mental health services (CAMHS) and adult mental health services (AMHS) or learning disability services will work in partnership with young people and their parents or carers and with each other and will share their expertise and resources to achieve smooth and effective transitional care arrangements.
It is also very important that the services work together to provide adequate support for parents or carers.
The importance of using the care programme approach (CPA) for children and young people with mental health needs is increasingly recognised. Standard 9 of the National Service Framework for Children, Young People and Maternity Services (DH, 2004), identifies CPA as good practice in delivering effective transitional care for young people: ‘The care programme approach, modified to meet the needs of younger people, should be used to plan transition, and transition supported by agreed protocols,’ and ‘When children and young people are discharged from in-patient services into the community and when young people are transferred from child to adult services, their continuity of care is ensured by use of the care programme approach.’
Adults who have parenting responsibilities for a child under 18 years may require help with these responsibilities. In such cases, councils may also have a duty to provide services under section 47 of the Children Act 1989, to safeguard and promote the welfare of children in their area. Where appropriate the framework for the assessment of children in need and their families should be used to explore whether there are any issues relating to children in need and their parenting. See care programme approach (CPA) policy and safeguarding children policy.
2 Purpose
The purpose of this policy is to ensure a safe, effective and positive transition of care for those young people receiving CAMHS who, due to the ongoing nature of their health and, or mental health needs, will continue to require care and treatment from adult mental health or adult learning disability services.
It sets out the requirement for the CAMHS, special needs schools and adult mental health services assessment and care planning systems to interlink proactively and smoothly, in order that the experience of the young person is positive, and the transition arrangements and ongoing care provision is safe and effective.
3 Scope
This protocol applies to young people up to the age of 18 who are under the care of CAMHS, and principally, but not exclusively, to staff working in CAMHS, adult mental health and learning disability services. For young people who are being treated within CAMHS for an eating disorder, the transition age is 19 years.
4 Responsibilities, accountabilities and duties
4.1 The board of directors
The board of directors has responsibility for the implementation of this policy and the monitoring of compliance. This responsibility is delegated to the trust chief executive who will delegate lead strategic responsibility to a director.
4.2 Chief operating officer
As nominated strategic lead, the chief operating officer is responsible for:
- the implementation of all policies and procedures which are in place to meet the needs of patients
- monitoring adherences to this and other related policies
- adequate resources and training being available to the clinical teams
- monitoring staff compliance with training as set out in the mandatory and statutory training policy and mandatory risk management training needs analysis matrix
- the development, implementation and monitoring of effective systems of supervision for clinical staff
4.3 Executive medical director
The executive medical director is responsible for providing clinical leadership within the trust and for the provision of senior clinical advice to the board of directors. The executive medical director is responsible for resolving issues where there are differences of opinion, which cannot be resolved by the care group medical directors in the locality care groups, and the lead consultant in children and young people’s mental health (CAMHS).
4.4 Director of nursing and quality
The director of nursing and quality has lead responsibility for clinical assurance within the trust, supported by the deputy director of nursing and quality. They are responsible for supporting implementation this policy through for example, clinical audit and mandatory risk management training.
4.5 Care group directors
Care group directors in children’s, Doncaster, Rotherham, North Lincolnshire.
Care group directors are responsible for:
- the implementation of the policy across the specified care groups
- the ongoing review of the policy to keep it up-to-date with current best practice
- promoting collaborative working between services, in order that the needs of the patient remain at the centre of the process
- providing reports to the operational management group (OMG) on any issues associated with the implementation of the policy
- facilitating effective joint working with internal and external partners and stakeholders
- monitoring staff compliance with the relevant mandatory risk management training as set out in the mandatory and statutory training policy and mandatory risk management training needs analysis matrix
- the development, implementation and monitoring of effective systems of supervision for clinical staff within their business division
4.6 Care group medical directors
Care group medical directors in Doncaster, Rotherham, North Lincolnshire and lead consultant psychiatrist, children and young people’s mental health services (CAMHS).
The role of the care group medical director is to provide advice to colleagues within children’s and locality care groups. The role is supportive and facilitative. The care group medical director may be asked to advise and, or provide a second opinion for patients with complex needs where there are professional differences of opinion between care groups.
4.7 Service managers
Service managers in children and young people’s mental health services (CAMHS), locality adult mental health and learning disability.
- Service managers are responsible for the implementation of the policy within their areas of responsibility.
- They are the next point of escalation in cases where there are differences of opinion at team manager and, or at pathway meetings.
- They will monitor that all relevant staff access the relevant mandatory risk management training as set out in the mandatory and statutory training policy and mandatory risk management training needs analysis matrix.
4.8 Community team managers
Community team managers in children and young people’s mental health services (CAMHS), adult mental health and learning disability.
- The manager is responsible for identifying the appropriate numbers and levels of staff and the training required for those staff to deliver safe and effective services.
- The adult community team managers are responsible for the appropriate allocation of transition cases to staff.
- The manager is responsible for the provision and monitoring of supervision within their team in line with the clinical and management supervision policy for clinical staff.
- The CAMHS manager is responsible for ensuring that appropriate, relevant and up-to-date information is provided to the service which the young person is transferring to.
- Adult mental health and learning disability services will identify a key worker for CAMHS staff to liaise with in relation to discussing relevant team to meet the needs of the young person and discuss any transition issues.
4.9 Community clinical staff
Community clinical staff in children and young people’s mental health services (CAMHS), adult mental health and learning disability) care coordinator or lead professional or allocated worker.
Working collaboratively with colleagues in CAMHS or adult mental health services and special needs schools, in order that the needs of the patient remain at the centre of the process.
- Implementing this protocol and the policy guidance set out within the care programme approach (CPA) policy.
- Implementing the disengaging with services (C or YP and CAMHS) policy.
- Informing the manager of any circumstances in which the application of this protocol is compromised.
- CAMHS practitioner will provide up-to-date relevant clinical information to summarise care and treatment provided from CAMHS, alongside future care needs.
4.10 Clinical staff
All clinical staff involved in the delivery of care to children, young people and adults, are responsible for:
- alerting the care co-ordinator or key worker or allocated worker of any concerns regarding quality, safety or effectiveness of care or if a child or young person has not attended an appointment or it is suspected that they are disengaging from services
4.11 Peer support workers
Peer support workers based within children and young people’s mental health services (CAMHS) and learning disability.
Peer support workers help young people, their carers and their CAMHS workers supporting with a young person’s transition to adult services or discharge from CAMHS as they approach 18 years old.
Through our own experiences of being patients in mental health services PSWs are better able to understand a young person’s situation.
PSWs support the young person, by:
- building a relationship with them, using our own lived experiences of recovering from mental ill health to show a deeper understanding of their situation
- listening to the young person fully and helping them to explore their hopes and fears about the future
- encouraging them to take responsibility for themselves and their mental health
- helping young people to become more independent and supporting them to expand their comfort zone
- helping the young person to get familiar with adult services (transport, location and people they need to know)
- building up a plan to manage their health and wellbeing which they can use with support from adult services
- helping the young person to find solutions to some of their problems by teaching them problem-solving techniques
- supporting the young person, their carers and their CAMHS worker to make their transition or discharge run smoothly
- peer support workers will work collaboratively with the lead professional or care coordinator to support the delivery of the transition and care plan
- alert the care co-ordinator or key worker or allocated worker of any concerns regarding quality, safety or effectiveness of care, or if a child or young person has not attended an appointment or it is suspected that they are disengaging from services
5 Procedure
5.1 General principles of transition
The transition process must be managed sensitively and collaboratively to support continued engagement of the young person and their parents or carers and safe and effective service delivery.
The involvement of the young person and their carers, collaborative working and effective communication between everyone involved is central to successful transition arrangements.
The transition process should be considered for appropriateness at 6 months prior to service age limit, considering the clinical reasoning for requirement of ongoing treatment and intervention moving forwards for the young person.
In circumstances where treatment can be concluded within CAMH services but would be beyond 18 years of age this can be supported to reduce the requirement to transfer care and impact on treatment.
Where a referral is received for a young person and is within 6 months of transition age, choice of service will be offered and age appropriateness or emotional maturity considered.
CAMHS and adult service understanding of each other’s service offer supports the effective transition between services. Good knowledge of the service being referred to or received from supports the engagement with young people in the process, they are assisted to understand the service offer moving forwards and how this may be similar or different to current service provision.
To support the joint working between services regular CAMHS or adult service attendance at each other services team meetings to share developments, explore any challenges or concerns and increase communications.
Joint working and care planning between adult and CAMH services identifies the transition processes and who is responsible for different elements of care plan delivery. Allocation of future identified worker is imperative to positive transition processes. See appendix A for an example of a transition care plan.
The majority of the Mental Capacity Act (2005) applies to young people aged 16 to 17 years who may lack capacity. All staff must therefore work within the provisions of the Act and its Code of Practice (2007). See MCA Mental Capacity Act 2005 policy and MCA deprivation of liberty (DoL) policy.
Where the care programme approach (CPA) is applicable it will underpin the transitional process and any ongoing care planning needs, that is:
- comprehensive assessment of health and social care needs
- agreement and production of a care plan
- appointment of a care coordinator and
- regular review of care
Due consideration will be given to the content and wishes of any advance statement produced by the young person.
All discussion and decision-making should take place as far as possible with the involvement of the young person, their parents or carers and relevant workers of both services during the transition process.
5.2 Transition from children and young people’s mental health services (CAMHS) to adult mental health services learning disability
Transition from CAMHS to adult mental health, learning disability services
The CAMHS care coordinator or lead professional will identify those young people known to their services age 17 and a half years and over, whose care will potentially need to transfer to adult services. For locality specific arrangements for transition to adult mental health see appendix B to D, for learning disability service transition see appendix E.
Once agreement has been reached about the adult mental health or learning disability service which will be appropriate for the young person to transition to discussions will take place with the young person, their parents or carers and peer support worker.
Adult mental health services will identify a care coordinator who will liaise with the CAMHS lead professional, a joint transition meeting will take place to include the young person and carers and peer support workers as appropriate to the wishes of the young person. The purpose will be to discuss and agree with the young person and their parents or carers the components of, and responsibility for the transitional care plan and any ongoing care needs, including identification and management of any safety or risk issues.
A transition care plan will be developed and recorded in collaboration with the young person to address the following issues:
- future care plan needs, and services offered within adult mental health or learning disability services
- timescales for transition
- involvement of peer support workers
- communication and involvement of carers or parents
- exit or discharge plans from CAMHS
The responsibility for leading the transition arrangements will remain with CAMHS if the young person is currently involved with CAMHS at the time of being eligible for adult services.
An initial transfer plan will be agreed between CAMHS and adult mental health or learning disability services, together with the name of the lead professional or care co-ordinator under CPA.
Both CAMHS and adult mental health services or learning disability (as appropriate) will share equal responsibility for the delivery of care for the service user throughout the transition process and CAMHS will only discharge that duty at the end of the agreed transfer process. A CAMHS discharge date will be agreed upon completion of the transfer and formally recorded.
Information relevant to the provision of effective care and treatment will be shared with the consent of the young person. Only in exceptional circumstances will information be shared without their consent, for example, in line with local policies to ensure safe and effective service delivery. If over 16 and lacks capacity information can be shared in their best interests. If under 16 and not Gillick competent then consent can be given from person with parental responsibility.
Transitional arrangements will be implemented at a pace with which the young person and their parents or carers are happy and which promotes consistent quality, safety and continuity of care.
Peer support workers are able to continue to support the young person following discharge from CAMHS with the engagement in adult mental health services for an agreed period of time as per care plan.
Wherever possible, when significant mental health problems have already been identified, the treatment episode should continue until completion with CAMHS or until an appropriate transitional point is reached within the care plan.
Where a young person has an education health care plan (EHCP) in place, this will inform and be part of the transition between services. EHCPs cover ages 0 to 25 years of age, as part of the Children’s Act 2014 supporting access to education where a young person has additional needs.
5.3 New referrals to adult mental health services learning disability
For new referrals of young people aged 17.5 years and over, consideration of services will be completed by CAMHS and adult mental health services (via the access or single point of Access team) or the specialist learning disability service. Consideration will be given to the preference on the young person, expected duration of intervention required and presenting needs.
5.4 Transition and joint working with children and young people’s mental health services (CAMHS) and early intervention in psychosis team
For young people aged under 16 years, the responsibility and care coordination will be led by the CAMHS clinician, with close liaison with the Early Intervention in Psychosis team for additional support as necessary. Medical input will be provided by a child and adolescent psychiatrist with support from the early intervention in psychosis psychiatrist for those under 16 years of age.
For young people aged 16 to 18 years, the responsibility for care coordination will be led by the Early Intervention in Psychosis team, with additional support and therapeutic interventions from the CAMHS as required or beneficial for the young person and their family. Medical input will be provided by the early intervention in psychosis psychiatrist.
See appendix F for further detail.
6 Training implications
No specific training for transition.
As a trust policy, all staff need to be aware of the key points that the policy covers. Staff can be made aware through:
- team meetings
- one to one meetings
- supervision
- special meetings
- practice development days
- local induction
7 Monitoring arrangements
7.1 Number of transitions taking place with a care plan in place
- How: Quarterly report to commissioners.
- Who by: Performance team.
- Reported to: Finance, performance and people meeting and local commissioners.
- Frequency: Quarterly.
8 Equality impact assessment screening
To access the equality impact assessment for this policy, please email rdash.equalityanddiversity@nhs.net to request the document.
8.1 Privacy, dignity and respect
The NHS Constitution states that all patients should feel that their privacy and dignity are respected while they are in hospital. High Quality Care for All (2008), Lord Darzi’s review of the NHS, identifies the need to organise care around the individual, ‘not just clinically but in terms of dignity and respect’.
As a consequence the trust is required to articulate its intent to deliver care with privacy and dignity that treats all service users with respect. Therefore, all procedural documents will be considered, if relevant, to reflect the requirement to treat everyone with privacy, dignity and respect, (when appropriate this should also include how same sex accommodation is provided).
8.1.1 How this will be met
This policy supports the development of personalised care planning for young people who are transitioning from CAMHS to adult mental health and learning disability services.
8.2 Mental Capacity Act (2005)
Central to any aspect of care delivered to adults and young people aged 16 years or over will be the consideration of the individuals’ capacity to participate in the decision-making process. Consequently, no intervention should be carried out without either the individual’s informed consent, or the powers included in a legal framework, or by order of the court.
Therefore, the trust is required to make sure that all staff working with individuals who use our service are familiar with the provisions within the Mental Capacity Act (2005). For this reason all procedural documents will be considered, if relevant to reflect the provisions of the Mental Capacity Act (2005) to ensure that the rights of individual are protected and they are supported to make their own decisions where possible and that any decisions made on their behalf when they lack capacity are made in their best interests and least restrictive of their rights and freedoms.
8.2.1 How this will be met
All individuals involved in the implementation of this policy should do so in accordance with the guiding principles of the Mental Capacity Act (2005) (section 1).
9 Links to any other associated documents
- Care programme approach (CPA) policy
- Safeguarding children policy
- Disengaging with services (C or YP and CAMHS) policy
- Consent to care and treatment policy
- Mental Capacity Act (2005) policy
- Mental Capacity Act advance statements and advance decisions to refuse treatment
- Supervision policy
- Mandatory and statutory training policy
- Mental Capacity Act deprivation of liberty (DoL) policy
10 References
- Department of Health (2008) Refocusing the Care Programme Approach: Policy and Positive Practice Guidance.
- Department of Health (2004) National Service Framework for Children, Young People and Maternity Services.
- HM Government (2000) The Framework for the Assessment of Children in Need and their Families.
11 Appendices
11.1 Appendix A example transition care plan
11.1.1 Summary of problem or need
Move from CAMHS to adult mental health services for ongoing mental health interventions.
11.1.2 Goal, what do we want to achieve?
To transfer from CAMHS to adult mental health services in a planned and supported way.
11.1.3 How will we know that we have achieved it?
I will be receiving support from a new adult mental health worker and engaged in treatment.
We will agree what I want to achieve from coming to the adult mental health services and how we are going to do this.
11.1.4 Actions
- Meeting to be held between CAMHS and adult mental health staff member.
- Meeting with me, my CAMHS worker, my peer support worker and my Mum to discuss the new service and my needs.
- We will agree what I want to achieve from coming to the adult mental health services and how we are going to do this.
- My mum will also have the opportunity to talk about her worries about the change.
- The peer support worker will help me to get used to going to the new place for appointments and offer support.
11.1.5 Involvement, who will do what?
My CAMHS worker will talk about the change in services.
The peer support worker will help with the practical things (going to the new venue etc).
The adult mental health worker will work with me on a new care plan.
11.1.6 Timeframe, when will we aim to have this done by?
It is planned that the transition will have happened by my 18th birthday, but if this hasn’t occurred, we will review the timescales to when it feels right.
11.2 Appendix B Rotherham children and young people’s mental health services (CAMHS) to adult mental health services and new referrals pathways
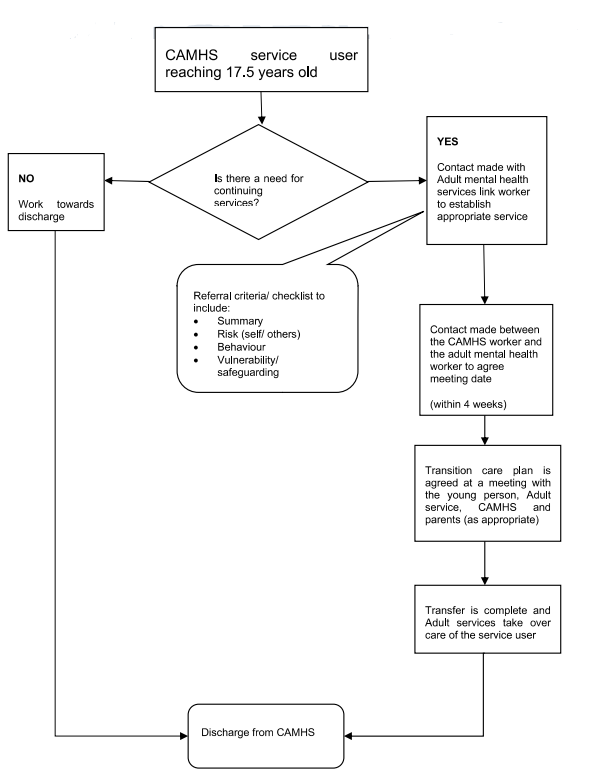
- CAMHS service user reaching 17.5 years old.
- Is there a need for continuing services?
- No, work towards discharge, discharge from children and young people’s mental health services (CAMHS).
- Yes, contact made with adult mental health services link worker to establish appropriate service. Referral criteria checklist to include:
- summary
- risk (self or others)
- behaviour
- vulnerability or safeguarding
- Contact made between the CAMHS worker and the adult mental health work to agree meeting date (within 4 weeks).
- Transition care plan is agreed at a meeting with the young person, adult service, CAMHS and parents (as appropriate).
- Transfer is complete and adult services take over care of the service user.
- Discharge from CAMHS.
11.3 Appendix C North Lincolnshire children and young people’s mental health services (CAMHS) to adult mental health services and new referrals pathways
- Young person identified as requiring transition to community adult mental health services.
- CAMHS care coordinator makes referral to adult mental health services via an e-referral on SystmOne.
- Referral discussed as part of weekly leadership meeting and care co-ordinator to be invited to present and discuss the referral:
- referral declined or signposted. End process
- Referral accepted based on service criteria.
- Community pathway identified. If patient in a placement CAMHS to continue to be lead agency who care co-ordinates until the age of 18 years.
- Allocated community practitioner makes contact with CAMHS worker to arrange hand over and joint visit with service user, family or carers.
- Team leaflet to be sent out. End process.
11.4 Appendix D Doncaster children and young people’s mental health services (CAMHS) to adult mental health services and new referrals pathways
- CAMHS to contact relevant AMH locality CMHT and complete e-referral (Central, East, North, South).
- AMH CMHT to arrange a clinical meeting for discussion.
- Joint visit arranged and timescales for transition agreed.
- Patient will be allocated a lead professional or care co-ordinator. End process.
11.5 Appendix E children and young people’s mental health services (CAMHS) to learning disability services pathways
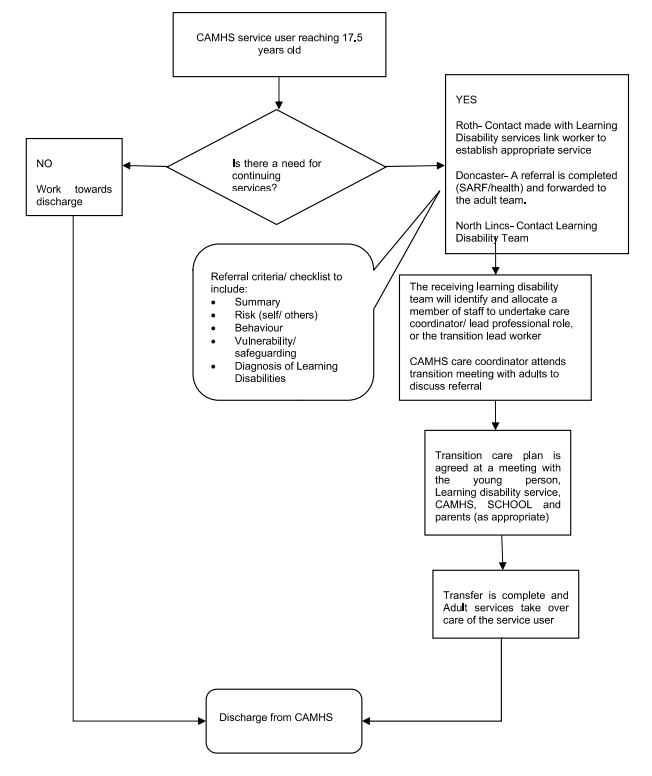
- CAMHS service user reaching 17.5 years old.
- Is there a need for continuing services?
- No, work towards discharge, discharge from CAMHS.
- Yes, Rotherham, contact made with learning disability services link worker to establish appropriate service. Doncaster, a referral is completed (SARF or health) and forwarded to the adult team. North Lincolnshire, contact Learning Disability team. Referral criteria or checklist to include:
- summary
- risk (self or others)
- behaviour
- vulnerability or safeguarding
- diagnosis of learning disabilities
- The receiving learning disability team will identify and allocate a member of staff to undertake care coordinator or lead professional role, or the transition lead worker. CAMHS care coordinator attends transition meeting with adults to discuss referral
- Transition care plan is agreed at a meeting with the young person, learning disability service, CAMHS, School and parents (as appropriate)
- Transfer is complete and adult service take over care of the service user.
- Discharge from CAMHS.
11.6 Appendix F children and young people’s mental health services (CAMHS) and early intervention in psychosis joint working
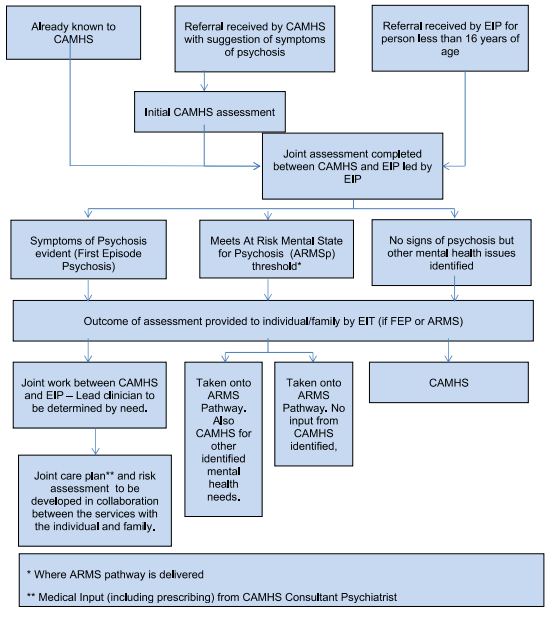
- Already known to CAMHS, referral received by CAMHS with suggestion of symptoms of psychosis (initial CAMHS assessment) or referral received by EIP for person less than 16 years of age.
- Joint assessment completed between CAMHS and EIP led by EIP:
- option 1, symptoms of psychosis evident (first episode of psychosis)
- option 2, meets at risk mental state for psychosis (ARMSp) threshold (where ARMS pathway is delivered)
- option 3, no signs of psychosis but other mental health issues identified
- Outcome of assessment provided to individual or family by EIT (if FEP or ARMS:
- option 1 outcomes:
- joint work between CAMHS and EIP, lead clinician to be determined by need
- joint care plan (medical input (including prescribing) from CAMHS consultant psychiatrist) and risk assessment to be developed in collaboration between the services with the individual and family
- option 2 outcomes, either:
- taken onto the ARMS pathway, with CAMHS involved for other identified mental health needs
- taken onto the ARMS pathway, with no input from CAMHS identified
- option 3 outcome:
- CAMHS
- option 1 outcomes:
Document control
- Version: 6.2.
- Unique reference number: 49.
- Approved by: Clinical policy review and approval group.
- Date approved: 5 December 2024
- Name of originator or author: Service manager, CAMHS.
- Name of responsible individual: Clinical quality group or service manager, CAMHS.
- Date issued: 18 December 2024
- Review date: 31 March 2025
- Target audience: Clinical staff, particularly children and young people’s mental health services (CAMHS), adult mental health services and learning disability services.
Page last reviewed: June 13, 2025
Next review due: June 13, 2026
Problem with this page?
Please tell us about any problems you have found with this web page.