Contents
- Introduction
- Purpose
- Scope
- Responsibilities, accountabilities and duties
- Procedure or implementation
- Training implications
- Monitoring arrangements
- Equality impact assessment screening
- Links to any other associated documents
- References
- Appendices
To download the ECT care record follow the link: CR11 ECT care record.
1 Introduction
For the Rotherham, Doncaster and South Humber localities there is one centralised electro convulsive therapy (ECT) department which is located in Rotherham. This department provides ECT treatment to patients across these three areas. It is a purpose-built treatment suite and is staffed by a dedicated team that has received training to work within the department.
NICE guidelines (2003; 2009) recommend that electro convulsive therapy (ECT) is used only to achieve rapid and short-term improvement of severe symptoms after an adequate trial of other treatment options has proven ineffective and, or when the condition is considered to be potentially life threatening in individuals with:
- severe depressive illness
- catatonia
- a prolonged or severe manic episode
The decision as to whether ECT is clinically indicated should be based on a documented assessment of risks and potential benefits to the individual including:
- the risks associated with the anaesthetic, current co-morbidities, anticipated adverse events particularly cognitive impairment and the risk of not having treatment
See protocol for maintenance or continuation (appendix A ECT protocol 1).
2 Purpose
These guidelines have been written to reflect the NICE recommendations (2003; 2009) and aims to provide a framework for giving the highest possible quality of clinical care to any patients who are prescribed this course of treatment
3 Scope
The contents of this policy apply to:
- all staff who are employed to work within the ECT department, including staff from the Rotherham older peoples services who provide cover through a service level agreement
- any staff who are responsible for escorting patients to the department for treatment
4 Responsibilities, accountabilities and duties
4.1 Lead consultant for the ECT department
The lead consultant is responsible for:
- the development of the protocols for the department
- training the junior doctors in relation to the safe administration of ECT
- keeping their own practise in relation to ECT updated by attendance at relevant training, and conferences
- reporting any concerns in relation to safe practise within the ECT department
- participating in audit programmes
4.2 Lead nurse for ECT department
The lead nurse is responsible for:
- the day-to-day running and management of the department
- checking that all equipment is maintained and in safe working order
- the care of any patients whilst they are in the department
- keeping their own practice in relation to ECT updated by attendance at relevant training, and conferences
- reporting any concerns in relation to safe practise within the ECT department
- participating in audit programmes; and Training other members of the Nursing team to assist within the department
4.3 Lead anaesthetist
The lead anaesthetist is responsible for:
- assessing patient suitability to receive an anaesthetic
- advising in relation to anaesthetic practice and equipment within the department
- assisting in audit programmes within the department
- attending training to keep themselves up to-date with ECT practice
4.4 Operating department practitioner
The operating department practitioner will work with the anaesthetist to prepare the drugs and equipment needed for the safe delivery of an anaesthetic to the patients.
4.5 Recovery nurse
The recovery nurse is responsible for the post-anaesthetic care of the patients in the department until satisfied that the patient is fit to be transferred to the post recovery room.
4.6 Consultant psychiatrist
The consultant psychiatrist in charge of the patient’s care must make the initial decision to give a patient ECT; this must involve an assessment of the risks and benefits and document alternative treatments which have failed.
The consultant psychiatrist should also decide the initial frequency and laterality of ECT; this will depend on previous response to ECT, cognitive difficulties and urgency of treatment. The choice of electrode placement should be a part of the consent process and discussed with the patient where possible.
See appendix C ECT protocol 3.
The consultant psychiatrist in charge of the patient’s care must also assess the patient’s capacity to consent and follow the appropriate procedures to obtain consent or Mental Health Act documentation. All detained patients should be given the Mental Health Act Commission leaflet number 3. The consultant should document all of the above on the ECT care record (page 3).
The consultant should ensure that copies of the Mental Health Act (1983) documentation is filed in the case notes; this should be in addition to the copy in the case notes to avoid accidental loss).
The consultant nominated deputy or ward staff may refer the patient to the ECT team.
See appendix D ECT protocol 4.
4.7 Qualified ward staff registered mental health nurse
Qualified staff on the ward should complete the care record, ensuring that the theatre checklist is completed, and the physical observations have been written on the treatment sheet.
Ward nursing staff should also make sure that all the relevant documentation is available and completed, to avoid delay in the ECT suite; this may include Mental Health Act papers, the ECT care record, VTE assessment, patient notes (mental health and general, if appropriate), blood results and ECGs.
The patient should also be wearing an identity bracelet with their allergy status identified as necessary (see appendix E ECT protocol 5).
See appendix E ECT protocol 5.
Ward staff also need to make sure that the escort policy is adhered to, to avoid the team refusing treatment of a patient. If there are staffing difficulties, the wards can contact the ECT suite to discuss staggering the patients from that area to allow staff to return.
There may also be issues with a patient who may become violent or aggressive when attending ECT. They can be accommodated but this may need some planning prior to the treatment day, please discuss with ECT staff.
See appendix G ECT protocol G.
The ECT staff are available to talk to patients and offer reassurance if required (if logistically possible); as link nurses undergo training, they will take up this responsibility in the Doncaster and South Humber locations. To arrange a visit from ECT staff or to show a patient around the department contact the ECT office (01709 447013).
Ward staff should also ensure that the patient has been given the information booklet about ECT during preparation for treatment (and if detained under the Mental Health Act (1983) leaflet number 3).
4.8 Escorting nurse
In accordance with the Royal College of Psychiatrists ECT handbook (2006), the escort nurse must be a qualified registered nurse whom the patient knows reasonably well; and who can act as an advocate, assessing concerns and informing the team; as well as giving reassurance to the patient both before and after treatment. The escort should be aware of the patient’s legal and consent status and have an understanding of ECT.
The escort nurse should have at least basic resuscitation training and remain with the patient during all stages of treatment. In the case of in-patients, the ideal escort is the patient’s named nurse, while in the case of outpatients, the patient’s community nurse or key worker should perform this function. If a driver is required, this person must be independent to the escort nurse.
Please refer to section 5.7.
On arrival at the unit, the escort should report to the ECT nursing staff and have in their possession the necessary documentation required for ECT to be given. They should report to the ECT staff any relevant information regarding the patient and their treatment. The escort nurse is responsible for the patient’s possessions and valuables whilst on the ECT unit but can sign them into the lockers provided if they wish to do so.
The escort nurse must remain with the patient throughout their treatment, including in the treatment room in order to provide reassurance to the patient and answer any questions from the ECT team should they arise.
The escort should also monitor the patient closely following treatment (in post recovery or discharge lounge) ensuring they continue to appear physically stable and report any concerns regarding this or the patient’s mental or cognitive functioning to the ECT team.
The escort nurse must obtain permission from the ECT nurse or recovery nurse before the patient can leave the ECT unit. It is the responsibility of the escort nurse to ensure that all relevant documentation is returned with the patient.
4.9 ECT link nurses
Link nurses are to be trained in all the trust’s mental health units, to act as a liaison between the unit and the ECT department. It is envisaged that these nurses will have the knowledge to be able to ensure that preparation for ECT is properly carried out and be able to relay information to the patient and their relatives. They will also be able to pass this information on to other staff. The ECT staff are available to answer any queries or problems that may arise.
5 Procedure or implementation
5.1 Consent to treatment
Treatment under the Mental Health Act 1983 Section 58A of the MHA applies to ECT and to medication administered as part of ECT. It applies to detained patients and to all patients under 18 years of age (whether or not they are detained).
A patient who is consenting may not be given treatment under section 58A unless the clinician in charge, or a SOAD, has certified on MHA Form T4 that the patient has the capacity to consent and has done so.
Evidence that the patient has capacity to consent must be recorded on Form MCA1.
For further guidance refer to the MHA Code of Practice (opens in new window).
In all cases, SOADs should indicate on the certificate the maximum number of administrations of ECT which it approves.
5.1.1 Children and young people under 18
If the patient is under 18, only a SOAD may give the certificate, and the SOAD must also certify that the treatment is appropriate.
For children and young people under 18, a SOAD certificate by itself is not sufficient to authorise the treatment, unless they are detained. Clinicians must also have the patient’s own consent or some other legal authority.
5.1.2 Urgent cases where certificates are not required (sections 62, 64B, 64C and 64E)
Sections 58A does not apply in urgent cases where treatment is immediately necessary (section 62).
This applies only if the treatment in question is immediately necessary to:
- save the patient’s life
- prevent a serious deterioration of the patient’s condition, and the treatment does not have unfavourable physical or psychological consequences which cannot be reversed
Urgent treatment under these sections can continue only for as long as it remains immediately necessary. If it is no longer immediately necessary, the normal requirements for certificates apply.
5.1.3 Patients who lack capacity to consent
A patient who lacks the capacity to consent may not be given treatment under section 58A unless a SOAD certifies on MHA Form T6 that the patient lacks capacity to consent and that:
- the treatment is appropriate
- no valid and applicable advance decision has been made by the patient under the Mental Capacity Act 2005 (MCA) refusing the treatment in question
- no suitably authorised attorney or deputy objects to the treatment on the patient’s behalf
- the treatment would not conflict with a decision of the Court of Protection which prevents the treatment being given
Evidence that the patient lacks capacity to consent must be recorded on Form MCA1.
For further information refer to the MCA Mental Capacity Act 2005 policy and advance statements and advance decisions to refuse treatment policy.
5.2 ECT Department staff requirements
The minimum staffing requirements, which will allow ECT treatment to proceed, are as follows:
- 1 anaesthetist
- 1 operating department practitioner (ODP)
- 1 psychiatric doctor to give the ECT treatment. This doctor must have achieved the required level of competency in the administration of ECT under the supervision of the lead consultant prior to independent practice
- minimum 1 psychiatric nurse. At a minimum, one registered psychiatric nurse who has received additional training to work in the ECT department
- 2 ECT nurse or 1 ECT nurse plus 1 ECT support nurse. If only one ECT nurse, an ECT support nurse who has also received additional training to work in the ECT department
- where possible a member of nursing staff should accompany each patient, who is having ECT treatment (see nurse escort section). On no occasion will a patient be left un-chaperoned. Two staff (gender to be considered) will be in attendance at each stage of the treatment
5.2.1 Students in the department
There are often nursing students and medical students who wish to see ECT treatment; they must be in appropriate training (for example, medical, nursing, recovery, O or T).
Any arrangements made, need to ensure that there is only one student in the room where the ECT treatment is given. For training purposes, it is recommended that half the time is spent in the ECT treatment room and half the time can be spent in the ECT recovery room. This will make it possible for up to two students to attend at the same time; one in the treatment room, one in the recovery room, who can then swap halfway through.
For the purposes of nursing or medical student training, there is little if any benefit to seeing any more than two ECT treatments being given. The time spent in the recovery room can be used to observe issues relating to recovery but can also be spent in informal discussion with one of the trained ECT psychiatric nurses.
Students are present only to observe and will not participate in any way with the ECT treatment.
5.2.2 Volunteers
If volunteers are working in the ECT suite, they cannot be involved in direct clinical care of patients and should not be present in the rooms where the ECT treatment is given or in the room where recovery takes place.
5.3 Relatives or carers in the department
Relatives may be permitted to wait in the outpatient reception. It is not appropriate for relatives to sit in the ECT suite as there are other patients present receiving treatment.
5.4 Equipment and medical physics
There is a standard list of equipment which is used to enable ECT to be given safely.
It must be regularly serviced and maintained by a recognised authority, namely the Biomedical Engineering Department at RDGH in accordance with the trust’s medical devices management policy.
The list of equipment in the department can be found in appendix Q ECT protocol 17.
5.5 Drug requirements within the department
Drugs used on the ECT unit are requested by the consultant anaesthetist and monitored by the operating department assistants.
The nurse in charge of the ECT suite is responsible for ordering, monitoring and appropriate safe storage of the drugs.
Nursing staff must not be involved in the preparation of anaesthetic drugs.
The drugs used in the ECT Suite are ordered by the ECT nurse on a Tuesday morning or after treatment Friday morning. An ECT nurse is to collect medication when it arrives from the Brambles ward.
5.5.1 Drugs used and stored on the ECT unit
Routine stock:
- Suxamethonium Chloride Injection 100mg in 2ml
- Thiopentone 500mg
- Fresenius Propofol 1%
- Lignocaine Injection 1%
- Cyclizine Lactate 50mg
- Atropine Sulphate Injection 600mcg in 1 ml
- Diazepam Injection 5mg
- Ranitidine 50mg
- Water for injections, 10ml ampoules
- Sodium Chloride 0.9% 1 litre for IV infusion
- plus, one vial of alternative anaesthetic and muscle relaxants (to order more if a case occurs), Etomidate 2mg/ml and Atracurium Besilate 10mg/ml
- Emergency (less routine) stock
- Hydralazine Hydrochloride ampules 20mg
- Hydrocortisone as the sodium succinate 100mg
- Disopyramide 50mg in 5ml
- Glycopyprolate USP 600mcg in 3ml
- Aminophylline Injection BP 250mg in 10ml
- Verconium Bromide 10mg
- Glyceryl Trinitrate spray
- Salbutamol inhaler
5.6 Ward preparation for treatment
The medical team need to ensure that a patient is fully assessed prior to ECT. If there are physical complications with a patient, this may mean requesting an anaesthetic assessment or discussing the patient with the ECT staff. If unsure, advice should always be sought from the ECT team to avoid unnecessary delay to the beginning of treatment.
The standard tests are clearly outlined in the care record (U and E, FBC, ECG, X-ray if indicated and a physical examination). However, if there are contraindications to either ECT or anaesthesia, further tests may be required.
See appendix E ECT protocol 5 and appendix G ECT protocol 7.
The medical team must also ensure that the care record for the treatment is also completed. This includes ticking the Mental Health Act status, consent type, prescription required (weekly or twice weekly, unilateral or bilateral) and signing the treatment sheet.
The clinical team should also assess the patient before each treatment to monitor for any sign of adverse side effects and that further treatment is required (this is in addition to the interim reviews identified in the care record).
Medications may also need to be reviewed or withheld or given prior to treatment. It is the medical team’s responsibility to ensure the ward nurses are clearly informed which medications to give and withhold prior to ECT. If there is doubt, contact the ECT team for advice.
See appendix F ECT protocol 6.
In the interim review (at least weekly) the patient’s capacity to consent to ECT, clinical status, and cognitive side effects, including orientation and memory, should be assessed at least weekly and documented in the care record. The patient’s subjective experience of side effects and objective cognitive side effects should also be recorded, for example, through the use of a memory diary.
5.7 Patient transport arrangements
Patients travelling from inpatient facilities with escort (see escort section 4.8 of policy) must be transported in a suitable vehicle. This will usually be a taxi or a trust vehicle where available. The driver should always be in addition to the escorts.
There may be cases where due to mobility or increased risk an ambulance may be required. These should be arranged by ward staff in each area. Any issues with this can be discussed with the ECT team.
5.8 Treatment and recovery
5.8.1 Pre-treatment
Patients will arrive in the department at their agreed time and be asked to sit in the waiting room if safe to do so.
Delivering same sex accommodation within the ECT department.
In order to meet the Department of Health requirements, the following is in place:
- all patients attend the department wearing their own loose-fitting clothing
- treatment is coordinated so there is only one patient in the treatment room, and one patient in the recovery room
- patient flow through the department is controlled by the lead clinician to enable all patients to receive their treatment, and recovery with patients of the same sex. This covers any emergency situation where there may need to be more than one patient in recovery
See appendix B ECT protocol 2.
- The patient will be introduced to the team (and permission obtained for any observers to be present) in the pre-treatment or treatment room as appropriate. The ECT nurse will explain the procedure again and any further explanations required.
- The ECT nurse will fill in the pre-treatment checks before the treatment is given (see care record), including checking documentation, preparation and consent.
- The pre-treatment ECT staff will also complete the ECT register. The Consultant Psychiatrist will also explain what is happening as appropriate.
- The patient will then be taken into the treatment room where the staff will explain what they are doing while they place the monitoring equipment on the patient and prepare them for treatment.
- The consultant psychiatrist will decide and set the appropriate settings for the Thymatron, depending on the prescription (in care record), previous response and side effects.
See appendix H ECT protocol 8.
5.8.2 Treatment
- If during treatment the seizure continues for longer than 2 minutes, steps must be taken to terminate it.
See appendix I ECT protocol 9.
- The patient will then be monitored and observed in both recovery and in the post-treatment room until ready to go into the discharge lounge for a drink and diet.
- Following the ECT treatment being given, the psychiatrist completes the treatment section of the ECT care record.
- The anaesthetist completes the anaesthetic record and passes on any concerns or requests for alterations to treatment, to the recovery nurse and escort nurse.
- The recovery nurse will complete the care record and hand over any difficulties to the escort. The escort must remain with the patient at all times to monitor for any signs of difficulty or distress and offer reassurance or assistance during this time.
See appendix J ECT protocol 10.
- Escorts must ensure that the discharge criteria are met, and that ECT or recovery staff make the decision to discharge the patient from the ECT suite to their ward or transport.
- If there was an untoward event however minor, this should be recorded in both the ECT record pack and the patient’s clinical notes, and an IR1 completed as per trust serious incidents management policy for untoward events.
- Patients may attend for ECT as outpatients so long as it has been arranged in advance between the prescribing consultant psychiatrist and the ECT team. There should be an assessment of risk before, during and after treatment, and supervision protocols must be adhered to.
See appendix K ECT protocol 11.
Also note there may be differences to treatment of the elderly and young people, as deemed appropriate.
See appendix N ECT protocol 14 and appendix O ECT protocol 15.
5.8.3 Post ECT
The ECT department recommends that all patients remain at the department for at least one hour following treatment. This time may need to be extended for outpatients receiving treatment. (see outpatient guidelines page 40 of policy).
Before leaving the department, each patient must have their physical observations recorded (usually in recovery), as per discharge criteria.
See appendix J ECT protocol 10.
On return to the inpatient unit, the department advise that physical observations, for example, blood pressure, pulse and respirations are checked regularly, and the patient is monitored for any side-effects, for example, nausea, vomiting, headache, confusion, post-ictal seizures, muscular aches and stiffness, and memory loss.
Please note, the patient’s level of risk and motivation to self-harm is to be continuously assessed. Following every treatment, staff are to be aware of possible raised level of motivation which can lead to potential risk of the person acting upon thoughts of self-harm or suicide.
5.9 Post treatment care
Patients must be fully assessed at least weekly during a course of ECT. This will include assessing for any side effects, improvement, and an interim physical. (See care record). The cognitive assessment should take place at 24 hours after ECT and should include a mini mental state examination, retrograde amnesia and an assessment of subjective memory impairment.
The consultant psychiatrist or a section 12 approved doctor must assess the patient’s capacity to consent to ECT and complete the appropriate part of the care record (at least weekly on the interim review).
The care record must be completed fully, or treatment may be refused. The patient’s clinical status or symptomatic response should be assessed and documented between each treatment session by their prescribing team.
See appendix D ECT protocol 4.
Any decision to end treatment must also follow the appropriate guidelines. See appendix L ECT protocol 12. Patients will be further assessed by their consultant psychiatrist at 3, 6 and 12-months post ECT, to monitor and address any side effects, and assess the patient’s mental state.
5.10 Action in the event of an emergency
In the event of an adverse healthcare event the ECT team must be informed immediately (if not already present). The doctors will then decide the course of action in line with local policies.
See ECT Anaesthetic Copy.
Protocols for the management of anaesthetic emergencies are on laminated sheets located in the treatment room in the ECT suite. These include malignant hyperthermia, anaphylaxis, local anaesthetic toxicity, difficult airway society guidelines, resuscitation council guidelines and advanced life support guidelines.
The resuscitation trolley is located in the recovery room, with an emergency oxygen cylinder, a drip stand and the defibrillator. Any staff may be asked to collect one of these items. There is also further emergency medication in the ECT drug cupboard.
See appendix O ECT protocol 15.
In the event of a cardiac arrest, the anaesthetist and ODP will manage the situation. An ambulance will be called by telephone 999.
Give the exact location:
ECT Suite
The Woodlands
Oakwood Hall Drive
Rotherham
S60 2UD
Until the ambulance arrives follow local resuscitation policy or early warning guidelines as appropriate.
Any adverse event must be fully documented in the patient’s notes and using IR1 system. It is also good practice to contact the patient’s consultant and the modern matron and inform them verbally of the incident as soon as possible.
6 Training implications
6.1 Medical staff
- How often should this be undertaken: 2 Sessions during attachment Plus on going supervision.
- Length of training: Every four months, or until required level of competence. Decided by consultant.
- Delivery method: Observation discussion practical research reflection policy and protocol.
- Training delivered by whom: Lead consultant associate ECT consultant.
- Where are the records of attendance held: Electronic staff record system (ESR) medical education co-ordinators.
6.2 Nursing staff
- How often should this be undertaken: Each ECT session until required level of competence is achieved.
- Length of training: Each member of nursing staff is assessed individually on competence.
- Delivery method: Observe practical and discussion. Mandatory training, ILS, MVA policy and procedure.
- Training delivered by whom: ECT nurses.
- Where are the records of attendance held: ECT lead nurse.
6.3 Student nurses
- How often should this be undertaken: No formal placement within the ECT department attends on request.
- Length of training: Not applicable.
- Delivery method: Observation Only.
- Training delivered by whom: ECT lead nurse ECT nurse.
- Where are the records of attendance held: Student mentor.
6.4 Link nurses
- How often should this be undertaken: Each session until level of competence.
- Length of training: After initial training nurses will receive yearly refresher.
- Delivery method: Observe practical discussion mandatory training ILS, MVA policy and procedure.
- Training delivered by whom: ECT lead nurse ECT nurse.
- Where are the records of attendance held: Ward manager.
6.5 Students
- How often should this be undertaken: Once in a six week placement.
- Length of training: Once in a six week placement.
- Delivery method: Observe discussion policy and procedure.
- Training delivered by whom: ECT lead consultant associate consultant.
- Where are the records of attendance held: Electronic staff record medical education co-ordinator.
7 Monitoring arrangements
7.1 Compliance with the standards set out within this policy
- How: Audit.
- Who by: Lead consultant and lead nurse for ECT.
- Reported to: The Adult Business Divisions Leadership and Quality Group.
- Frequency: Yearly.
7.2 Number and type of any adverse health care incidents which occur within the department
- How: Incident investigation.
- Who by: Lead nurse for ECT in conjunction with the trust patient safety lead.
- Reported to: Trust Health and Safety Committee and the Adult Business Divisions Leadership and Quality Group.
- Frequency: As and when an incident occurs.
7.3 Staff compliance with the training requirements of this policy
- How: Audit of training records.
- Who by: Modern matron for the Rotherham older peoples service.
- Reported to: The Adult Business Divisions Leadership and Quality Group.
- Frequency: Yearly.
8 Equality impact assessment screening
To download the equality impact assessment associated with this policy, please follow the link: ECT policy EIA.
8.1 Privacy, dignity and respect
The NHS Constitution states that all patients should feel that their privacy and dignity are respected while they are in hospital. High Quality Care for All (2008), Lord Darzi’s review of the NHS, identifies the need to organise care around the individual, ‘not just clinically but in terms of dignity and respect’.
As a consequence the trust is required to articulate its intent to deliver care with privacy and dignity that treats all service users with respect. Therefore, all procedural documents will be considered, if relevant, to reflect the requirement to treat everyone with privacy, dignity and respect, (when appropriate this should also include how same sex accommodation is provided).
8.1.1 How this will be met
In order to maintain the privacy and dignity of patients who are receiving treatment within the department the following is in place:
- all patients attend the department wearing their own loose-fitting clothing
- treatment is planned for there to only ever be one patient in the treatment room, and recovery room at any given time
- patient flow through the department is controlled by the lead clinician to enable all patients to receive their treatment, and recovery with patients of the same sex. This covers any emergency situation where there may need to be more than one patient in recovery
- in the post recovery room there are curtains in place which screen each of the patient bays
8.2 Mental Capacity Act
Central to any aspect of care delivered to adults and young people aged 16 years or over will be the consideration of the individuals capacity to participate in the decision making process. Consequently, no intervention should be carried out without either the individual’s informed consent, or the powers included in a legal framework, or by order of the court.
Therefore, the trust is required to make sure that all staff working with individuals who use our service are familiar with the provisions within the Mental Capacity Act (2005). For this reason all procedural documents will be considered, if relevant to reflect the provisions of the Mental Capacity Act (2005) to ensure that the rights of individual are protected and they are supported to make their own decisions where possible and that any decisions made on their behalf when they lack capacity are made in their best interests and least restrictive of their rights and freedoms.
8.2.1 How this will be met
All individuals involved in the implementation of this policy should do so in accordance with the guiding principles of the Mental Capacity Act (2005).
9 Links to any other associated documents
- Consent to care and treatment policy
- Resuscitation manual
- Clinical risk assessment and management policy
- Medical devices management policy
- MCA Mental Capacity Act 2005 policy
- Advance statements and advance decisions to refuse treatment policy
- Infection prevention and control manual
- Section 62 procedure for clinical staff
- Listening and responding to concerns and complaints policy (formally complaints handling policy)
- Incident management policy
- Control of substances hazardous to health (COSHH) policy
10 References
- This policy is a local implementation of the: The ECT Handbook: The Third Report of the Royal College of Psychiatrists’ Special Committee on ECT (2005), Ed. Allan Scott; Gaskell.
- The handbook has a full list of references. Cheller A. 2000 Resuscitation. A Guide for Nurses. Dept of Health and Welsh Office. Mental Health Act 1983, Code of Practice.
- Department of Health, (2007). Code of Practice: Mental Health Act 1983. Stationary Office.
- Department of Health, (2007). Code of Practice: Mental Capacity Act 2005 Stationary Office.
- Dimond B C, Barker F H (1996) Mental Health Law for Nurses. Blackwell Science.
- Duffett R and Lelliott P (1997) Junior Doctors Training in the Theory and Practice of Electroconvulsive Therapy. Psychiatric Bulletin 21, 563 to 565.
- Duffett R and Lelliott P (1998) Auditing Electroconvulsive Therapy. British Journal of Psychiatry. 172, 401 to 405.
- Duffy, Grosz and Beatson (1999) A Guide to the Human Rights Act 1998.
- Sweet and Maxwell. Jones R (2009) Mental Health Act Manual 12th Edition Sweet and Maxwell.
- Heller T, Reynolds J, Gomm R, Huston R, Pattison S (1996) Mental Health Matters. Open University publication.
- Lester and Pannick (1999) Human Rights Law and Practice. Butterworths Pippard J and Ellam L (1981) Electroconvulsive Therapy in Great Britain. British Journal of Psychiatry 139, 563 to 568.
- NICE (2003), Guidance on the use of electroconvulsive therapy, Technology appraisal 59. DoH; London.
- NICE (2009). Depression in Adults (Update). Depression: The Treatment and Management of Depression in Adults. National Clinical Practice Guideline 90. DoH; London.
- Pippard J (1992) Audit of ECT in Two NHS Service Regions. British Journal of Psychiatry 160, 621 to 637.
- Robertson C and Ferguson G (1996) Electroconvulsive Therapy Machines. Advances in Psychiatry Treatment 2, 24 to 31.
- Royal College of Psychiatrists (1977). The Royal College of Psychiatrists Memorandum on the use of Electroconvulsive Therapy. British Journal of Psychiatry 131, 261 to 272.
- Royal College of Psychiatrists (1989). The Practical Administration of
- Electroconvulsive Therapy. London: Gaskell Royal College of Psychiatrists (1994) Electroconvulsive Therapy: The Official Training Video.
- Royal College of Psychiatrists (1995). The ECT Handbook: The second report of the Royal College of Psychiatrists Special Committee on ECT. Council Report CR39.
- Swage. Thoreya (2001) Clinical Governance in Health Care Practice. Butterworth. Heinemann.
10.1 Websites
- RCN Home Royal College of Nursing (opens in new window)
- NICE The National Institute for Health and Care Excellence (opens in new window)
11 Appendices
11.1 Appendix A Protocol 1, maintenance or continuation of ECT
11.1.1 Maintenance
ECT NICE (2003; 2009) recommend that ECT should not be used as a long-term treatment to prevent recurrence of depressive illness, apart from in exceptional circumstances as the evidence of its efficacy is limited and that it should not be used in the general management of schizophrenia.
Maintenance ECT may be prescribed if the patient has capacity or is consenting and is in agreement with the consultant psychiatrist to go ahead. The above must be clearly documented in the patient’s notes.
11.1.2 Continuation ECT
NICE (2003; 2009) recommended that more than one course of ECT should only be considered for someone who is experiencing an episode of severe depressive illness, catatonia or mania and who has not responded to a course of ECT but has responded well previously to ECT. The appropriate consent or Mental Health Act paperwork must be obtained.
Patients receiving either continuation or maintenance ECT should be reviewed by their consultant psychiatrist on a regular basis, the frequency of this will depend on the frequency of treatment. The clinical status of the patient, cognitive functioning (including MMSE, retrograde amnesia and assessment of subjective memory impairment) and side effects should be considered when deciding whether it is appropriate to continue with such treatment.
11.2 Appendix B Protocol 2, nursing protocols for running the ECT suite
11.2.1 Nursing protocols for running the ECT suite
Contact all wards by telephone, Doncaster Wards (Brodsworth, Cusworth and psychiatric intensive care unit), Scunthorpe wards (Mulberry and Laurel ward).
All telephone numbers are in the ECT information on the ECT desk.
If Scunthorpe or Doncaster have not contacted the ECT suite, ring and ask for their referrals. If both sites are requiring treatment on the same day, then Scunthorpe staff need to be informed that their patients must be at the Suite by 8.30am in order to allow pre-treatment checks to be completed before the team arrives.
Doncaster should arrive after Scunthorpe patients, and may wait in the Woodlands seating area until the first patient has gone into the pre-treatment area, to protect confidentially.
Swallownest Court acute wards will be informed the day before treatment of what time they are to arrive.
The Brambles and Glade wards should be telephoned on the day of treatment and are to arrive at the Suite when the last outpatient is in treatment.
11.2.2 Treatment day, preparation
8.00am, collect any supplies from the Brambles, for example, bread, milk margarine, any medications that have been ordered (2 pints of milk are ordered to arrive on the breakfast trolley every Tuesday and Friday) the keys for the ECT suite are kept in the Brambles safe.
Unlock the entire ECT suite and turn on all the lights.
Set up the ECT suite:
- firstly, by placing the required medications on the tray ready for the anaesthetist; ensure there is adequate stock and that the medications are in date. The medication to place on the tray is thiopentone, diazepam injection, atropine, cyclizine, lidocaine, atropine, ranitidine, water for injections and sodium chloride
- unlock the ECT fridge to allow access to the suxamethonium by the anaesthetist (it must remain in the fridge until it is required)
- place the tray on the work surface ready for the anaesthetist to use
- get 2ml and 10ml syringes out and place next to a brown injection tray
- get the ECG electrodes out of the cupboard under the Thymatron for the EEG reading and ECG monitoring
- check the emergency equipment is in working order including the suction machine (X4) and the defibrillator, and that there is adequate oxygen in the emergency tank
- make the four bed chairs ready for treatment by putting a continence sheet on the chair bed and covering them with a folded sheet and putting a pillow and blanket in place
- ensure there are alcohol wipes and electrode gel out for treatment and the Thymatron has been switched on and has completed its self-test
- also check there is enough paper in the EEG box
- to check the settings on the Thymatron press the Flexidial, then turn the dial till programmes is shown press the Flexidial again; the last set programme should be flashing, if this is not DGX then turn the dial until DGX shows. Press the start or stop button on the ECG to fix the settings, a printout will confirm the DGX setting with a pulse width of 1.00ms. The Thymatron is now ready
- tape an orange bag to the unit and get the gags out and place on the side ready for the anaesthetist to use
8.30 patients may be arriving from Doncaster, ask them to take a seat in the waiting area.
Ensure the wards have followed the escort policy, there should be one escort per patient this does not include bank staff or students. If the ward area is transporting more than one patient for treatment, then there should be one qualified staff member per patient. It is not safe to treat patients without this level of support and the anaesthetist may refuse treatment.
Check that all appropriate documentation has been checked on SystmOne which includes:
- the ECT prescription including mental state, cognitive functioning and capacity
- the medication chart
- Mental Health Act documentation section papers and the relevant consent form T4 or T6 or a 62
- general health notes and the ECT prescription is completed including the blood results
- ensure they are wearing a patient identification wrist band and they have been starved from 3am
- also ensure that they have taken the appropriate medications prior to treatment, inform the anaesthetist if they have not been given
Treatment must not commence till all the following have arrived:
- consultant psychiatrist
- anaesthetist
- ODA or ODP
- recovery nurse
- 2 ECT trained staff. Prioritise all patients due to physical health (for example, diabetes or potential anaesthetic risk)
11.2.3 Treatment
There will be 2 ECT staff present; one should complete the patient’s checklists and help in both waiting rooms and post recovery, the other member of staff (must be qualified) should assist in the treatment room.
Once the last person from Doncaster is waiting for treatment any patients from Swallownest court should be arriving, give them as much notice as possible of the quantity of patients you are treating, preferably the day before so they can organise transport. The same escort and treatment protocols apply.
In the pre-treatment room:
- make the patient comfortable on the identified ECT chair
- ensure the patient is wearing their wrist band
- introduce yourself to the patient, make sure they have adequate understanding of the treatment, and answer any questions the patient may have
- complete the check list in the care record ensuring the patient has had nothing to eat or drink, has taken all their appropriate medications, they have removed, or taped jewellery, and items are removed from their pockets
- at this stage dentures need to be removed and given to the escort nurse with the patients’ name written on the denture pot. If the patient does not have dentures then ask them of any dental problems, loose teeth, caps or crowns to which the anaesthetist must be informed of prior to treatment starting
- the escort for each patient should remain with the patient throughout the process and offer reassurance. They may also be required to answer any questions the anaesthetist has in the treatment room and report what normal behaviour is when in recovery (for example, mute or speaking agitation, confusion)
The ECT nurse not in the treatment room should:
- also check on the post recovery and waiting areas that there are no problems. This would also include changing the ECT chair and moving them into the pre-treatment room for the next patient
The staff in pre-treatment room should:
- receive a handover from the checking staff (if not the same person, one staff could follow a patient through the process) and discuss any issues with the anaesthetist or consultant psychiatrist
- the patient should be introduced to all members of the team
- explain what is happening then begin to place the monitoring EEG electrodes on the forehead and behind the ears on the mastoid bone (red on the forehead and green in the middle)
- place a small amount of contact gel on to the area of the patient where the paddles will be placed (this improves contact)
- meanwhile the ODA and the anaesthetist will be applying monitoring, oxygen, and sighting an intravenous cannula
- ask the patient to lie still and close their eyes while you test the EEG this is done by pressing start or stop on the Thymatron
- check with the consultant that the reading is okay
- the anaesthetist will check everyone is ready and induce anaesthesia; the staff should be quiet at this point as hearing is heightened for the patient as they fall asleep. The patient will also be given the muscle relaxant suxamethonium, staff should observe for this taking effect, it will produce fasciculation (a twitching of the muscles). This should have stopped before treatment begins. The anaesthetist should also place either a gag or an airway in the patient’s mouth before treatment commences
The consultant psychiatrist may also be teaching the foundation 2 doctors, in which case the ECT nurse will be responsible for pressing the treatment button whilst the foundation 2 doctor observes the consultant holding the Thymatron electrode paddles. The ECT nurse should only press the treatment button if the consultant has set and checked the Thymatron and given clear instructions. When you are performing this role, you should verbally confirm the treatment dose before pressing the treatment button. In a normal treatment session, the foundation 2 doctor will hold the Thymatron electrode paddles whilst being observed by the consultant psychiatrist.
- Ensure the person holding the Thymatron paddles has placed gel onto each side of the head to ensure good contact.
- The impedance will be checked once the paddles are in contact with the patient by pressing the impedance button on the Thymatron.
- Impedance must flash less than 3000 for there to be adequate contact.
- Once impedance is correct the consultant psychiatrist will verbally confirm the treatment dose.
- The nurse in treatment should place their hands over the patient’s limbs (not holding the patient down).
- The seizure is timed from the end of the electrical stimulation.
- The seizure is timed by the electroencephalogram monitoring (EEG).
- The clinical team need to record the visible seizure duration as EEG monitoring method is vulnerable to technical problems.
- Timing by the nurse should stop when the observed physical seizure is over.
- The consultant psychiatrist will decide when the seizure is over from the EEG reading.
- Once treatment is complete the anaesthetist will assist the patient to breath independently again and when satisfied will move the patient into the recovery area.
- If in the event that the seizure duration is prolonged (2 minutes) or the heart rate is slow, the anaesthetist may administer further medication, it is not the responsibility of the ECT nurse to draw up or administer any of these medications, they should be on the tray ready or in the drug cupboard and will be given by the anaesthetist or the operating department practitioner (ODP).
11.2.4 Recovery
The anaesthetists will hand over to the recovery nurse and check that they are satisfied with the patient’s condition. The escort nurse will remain with the patient in recovery and provide any assistance needed, including reassuring the patient as they wake up. The recovery nurse will decide when the patient is fit to transfer into post recovery room with their escort. If the escort is concerned about their patient, they should ask the recovery nurse or the ECT nurse (in pre-treatment) for assistance. Once the patient has rested and is fully conscious the escort can assist them to walk through to the final lounge, where the escort can make them a drink and offer some diet. Only the ECT nurse or recovery nurse may authorise for patients and escorts to leave the department (please bear in mind transport may take some time to arrive for Doncaster patients and patients from Swallownest court. The escort nurse and the patient may utilize the Woodlands Café while they wait for their transport to arrive.
11.2.5 Responsibilities after treatment is finished
All stock levels should be checked before the recovery nurse leaves the building as they will order the theatre supplies for the following treatment day. This includes airways, oxygen tubing and masks, cannulas, syringes and needles. Other stock should be ordered from Lloyds Pharmacy allow adequate time for the supplies to arrive.
The medication stock should be checked that none are near expiry dates and that there are adequate supplies for at least 2 treatments (a drugs list is on the inside of the drug cupboard).
The drug keys for the ECT department are to be kept in the locked controlled drug cabinet on the Brambles ward in the treatment room.
11.2.6 Cancellations
If treatment is cancelled the following people should be informed:
- consultant psychiatrist
- anaesthetist
- recovery staff and, or ODP
- rostered foundation 2 on call that day
- ECT staff
- all wards
11.2.7 Electronic record for documentation and inputting for ECT
- all patients receiving ECT need to be on the electronic system, prior to their treatment, during treatment, and discharging when treatment is completed
- please see and follow instructions for inputting this data on the electronic system
11.3 Appendix C Protocol 3, ECT protocol for choice of laterality of treatment
Bilateral or unilateral? and frequency?
All the advice here is taken directly from the Royal College of Psychiatrists ECT Handbook, second edition 2005. It is recommended that ECT is administered by a constant current, brief-pulse ECT machine with a wide output range and a facility for electroencephalography. The optimal frequency is said to be twice a week. Studies have shown no advantage with treatment given three times a week. There is no evidence that daily ECT leads to a more rapid response and memory impairment is severe.
Bilateral ECT (BECT) is thought overall to be better. Unilateral ECT (UECT) should be considered when:
- speed of response is less important
- there has been a previous good response to UECT
- minimising memory impairment is particularly important, for example, outpatient ECT
Bilateral ECT should be used when:
- speed and completeness of response have a priority
- unilateral ECT has failed
- previous bilateral ECT has produced a good response without undue short-term memory impairment
The choice of electrode placement should be a part of the consent process and discussed with the patient where possible.
11.3.1 Electrode positioning
For bilateral ECT, draw an imaginary line from the external auditory meatus to the lateral angle at the eye. Measuring 4cm above the midpoint of this line will give you the electrode positioning point. For unilateral ECT one of the electrodes is positioned as per bilateral and another in an arc 18 cm behind the first electrode.
Please note that electrode placements are often inaccurate. Placements tend to drift too far anterior or posterior. A too low placement is also a common mistake which would not give a passage of current across the brain. A conscious effort must be made on each occasion to ensure accurate electrode placement.
11.4 Appendix D Protocol 4, reference to ECT and consent
11.4.1 Prescribing ECT
All patients prescribed ECT must be under the care of a consultant psychiatrist. The initial decision to prescribe ECT and the assessment of capacity should be made by the consultant psychiatrist and documented in the patient’s clinical notes and the first section of the care record (page 3) (by the consultant psychiatrist). It is the responsibility of the consultant psychiatrist to ensure that the capacity status of their patient is properly assessed. This can be delegated to another section 12 approved practitioner. The capacity assessment must be documented in the patient’s notes and in the relevant sections of the ECT care record.
The following prescription parts and physical assessments may be completed and signed on behalf of the consultant by his or her medical team. This will include the section for consent to ECT, but this part should only be completed by the nominated deputy if the patient is deemed to have capacity and is informal. The RMO will need to consent the patient if detained (and give the patient Mental Health Act Commission leaflet no. 3) as a form T4 will be required if consenting, and if there is no consent (only where there is no capacity) the appropriate actions may be taken by the RMO (SOAD referral, form T6 or section 62 or form 4). During the consenting stage the patient should (except in an emergency) be given at least 24 hours to reflect on the information given regarding ECT and have time to discuss it with others. The prescription of ECT should also fall within NICE guidelines (2003; 2009) if this is not the case it should be clearly indicated within the case notes and the patient should understand this.
11.4.2 Patient referral system
Patients are usually referred to the ECT unit initially by telephone (by either ward staff or nominated deputy). It is recommended that the department is informed of possible referrals as early as possible to ensure that the offer of an ECT nurse or link nurse visit to the patient can be facilitated and any potential difficulties (including if the list is full or an anaesthetic assessment is required). Other than treatment days, messages can be left on the answer machine and staff will respond as soon as possible. In an emergency the lead clinician is available on a mobile phone and staff should contact Brambles Ward (01709 447002) for the number.
ECT treatment prescribing and documentation packs can be obtained via SystmOne. Once a treatment start date has been agreed between the referrer and ECT staff they may be booked into a treatment session by the ward staff.
See below for flow chart of referral and consent.
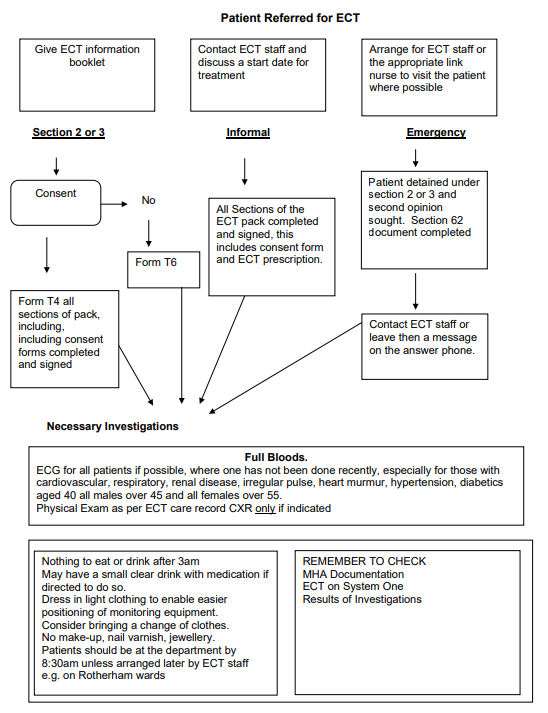
11.4.2 Flowchart patient referred for ECT
- Give ECT information booklet.
- Contact ECT staff and discuss a start date for treatment.
- Arrange for ECT staff or the appropriate link nurse to visit the patient where possible.
- Move on to section 11.4.2.4.
11.4.2.1 Section 2 or 3
- Consent, form T4 all sections of pack, including, including consent forms completed and signed.
- No consent, form T6.
- Move on to section 11.4.2.4.
11.4.2.2 Informal
- All sections of the ECT pack completed and signed, this includes consent form and ECT prescription.
- Move on to section 11.4.2.4.
11.4.2.3 Emergency
- Patient detained under section 2 or 3 and second opinion sought. Section 62 document completed.
- Contact ECT staff or leave then a message on the answer phone.
- Move on to section 11.4.2.4.
11.4.2.4 Necessary investigations
11.4.2.4.1 Full bloods
ECG for all patients if possible, where one has not been done recently, especially for those with cardiovascular, respiratory, renal disease, irregular pulse, heart murmur, hypertension, diabetics aged 40 all males over 45 and all females over 55. Physical exam as per ECT care record CXR only if indicated.
Nothing to eat or drink after 3am may have a small clear drink with medication if directed to do so. Dress in light clothing to enable easier positioning of monitoring equipment. Consider bringing a change of clothes. No make-up, nail varnish, jewellery. Patients should be at the department by 8.30am unless arranged later by ECT staff, for example, on Rotherham wards.
Remember to check:
- MHA documentation
- ECT on SystmOne
- results of investigations
11.5 Appendix E Protocol 5, preparation of patient for treatment
- All patients should have a full physical examination and any significant findings documented on the ECT care record.
- All patients should have a full blood tests including urea and electrolytes. A sickle cell test is required for all Afro-Caribbean, middle eastern, Asian and eastern Mediterranean patients, unless status is already known. LFTs are required for patients with cachexia, a history of alcoholism, drug abuse or recent overdose. If blood investigations have been done prior to the decision to give ECT then the prescribing doctor will need to use clinical judgement to determine whether the results should be repeated. Hepatitis B status to be identified where indicated, and the above test results documented in ‘other’ tests ‘, for example, sickle cell, Hep B, LFT’.
- If advice is required contact the ECT department.
- An ECG is required for all patients with cardiovascular, respiratory, renal disease, irregular pulse, heart murmur, hypertension, diabetics aged over 40, all males over 45 and all females over 55. It is therefore safe practice to give all patients an ECG if possible and they have not had one recently.
- Chest x-ray should be done if there is known or suspected lung disease, cardiac failure or any other medical indications. It specifically should not be done routinely, and only if there are indications.
- Any other investigations should be done as clinically appropriate. For example, blood sugar (BM stick) in diabetes, pregnancy testing (See care record for list of indicated health issues).
- It is very important that all medical investigations and results are documented on SystmOne prior to treatment.
- If there are any concerns at all about a patient’s fitness to have a general anaesthetic for electro-convulsive therapy then the case should be discussed with the lead anaesthetist.
- The Lead Anaesthetist can be contacted via Decphone 7939, via the anaesthetic secretary at Rotherham Foundation Trust Hospital on extension 4550, or via the ECT department.
- If the patient has in the past received ECT treatment, the previous integrated care pathway document ICP should be brought for the patient’s first treatment.
- All patients should be fasted from both food and fluids from 3am. In the morning patients may be given medication, which will not compromise treatment (for example hypotensive medication may be given) with sips of water. It may be agreed that a patient can have a glass of water at 6 am if they are having treatment later but this should be discussed with the ECT team. Patients who are taking cardiac medications, anti-hypertensive or beta-blockers routinely should continue and be administered the medication several hours before treatment with a sip of water.
- The patient should be asked to remove make up, nail varnish, contact lenses, body piercing etc. prior to treatment and requested to wear loose fitting clothing.
- Staff are advised to bring a change of clothes for the patient, as there are occasions where incontinence occurs.
- The patient should be given an identity bracelet by the ward nursing staff, on which should be the patient’s name, date of birth, patient number and consultant psychiatrist’s name. Allergy status should also be identified on the patient bracelet. if a patient has a known allergy the word ‘ALLERGY’ should be written in red pen on the bracelet, and the details of it written on the care record page 6.
11.6 Appendix F Protocol 6, patient’s medication during and after treatment
11.6.1 Concurrent medication
Concurrent therapy can be considered under 2 headings: general medication and specific psychiatric medication. Both have the potential to modify seizure thresholds.
Anticonvulsants, hypnotics and membrane stabilisers tend to raise the seizure threshold, while preparations containing theophyllines can have the opposite effect.
Patient’s concurrent medication is usually of a protective nature, such as antihypertensive, anti-anginal, anti-dysrhythmic, bronchodilator and, or antacid or anti-reflux therapy. These should be maintained and can usually be given safely, up to 2 hours before ECT, with sips of water if necessary. Those receiving long term steroids may need supplementary doses and those on ant cholinesterase therapy for glaucoma may require modification of the choice of muscle relaxant. Patients with diabetes who require insulin should attend early and should have medication withheld until after recovery. H² receptor antagonists and antacids should be prescribed for those at risk of oesophageal reflux. Concurrent psychiatric medication can have significant effects upon ECT. See table:
| Drug group | Effect | Action |
|---|---|---|
| Benzodiazepines | Anticonvulsant | Avoid high doses if possible |
| Tricyclics | Tend to be pro-convulsant | Not detrimental to ECT |
| SSRIs | Reduces seizure threshold | May give prolonged seizures |
| Fluoxetine | Long half-life | ECT may be commenced at a low dosage |
| MAOIs | Increases seizure threshold and BP Anaesthetist | Must be made aware |
| Lithium | Reduces seizure threshold | Levels checked and kept within a moderate range (0.4-1 mmol/l) |
Selective inhibitors of the reuptake of serotonin and noradrenaline can reduce seizure threshold and cause hypertension. Neuroleptics tend to be pro-convulsant at low dosage but increase seizure thresholds at higher dosage.
11.6.2 Recommendations for post ECT drug therapy
- Continuation treatment with doses of medication known to be therapeutic is essential for at least 6 months after successful ECT.
- Many patients who have suffered from recurrent episodes of illness will be candidates for longer-term prophylactic or maintenance treatment to reduce the likelihood of new episodes of illness.
11.7 Appendix G Protocol 7, dealing with potentially violent or very disturbed or agitated patients and patients who are deemed high risk
11.7.1 Potentially violent or very disturbed or agitated patients
Due to the presenting behaviour of some patients, it may not be desirable for them to be in the ECT department whilst other patients are undergoing treatment. If a risk is felt to be posed to other patients this should be discussed by the ward team with the nurse in charge of ECT so that special arrangements can be made.
Options to be considered are:
- treatments being administered early before other patients arrive within the department
- treatment to be given on alternative days when other patients are not within the department
- treatment to be given at the end of the session when all other patients have left the department
The option which best suits the needs of the patient should be selected in consultation with the ECT team, ward staff, anaesthetist and the patients’ consultant.
It may also be necessary for more than one nurse to accompany the patient from the ward to ensure safe movement of the patient between the ward and the ECT department.
Note, he patient should not be sedated prior to treatment unless it is under instructions of the patients’ consultant and the anaesthetist. Such sedation is not to be prescribed by a junior doctor.
11.7.2 Doncaster, Scunthorpe and Swallownest patients
It may not be possible or practical to follow the above guidelines whilst transporting a patient from Doncaster to Rotherham for ECT. In this case it should be discussed with the lead consultant for ECT whether it is necessary to transfer the patient to a Rotherham ward in preparation for ECT. This must be arranged between the consultants before a patient is sent.
11.7.3 High risk patients
If a patient has co-existing physical illness their treatment should be discussed with the lead anaesthetists, if they are unavailable the anaesthetist due to attend treatment, the rota is available in the ECT office). The ECT staff can facilitate this discussion or she can be contacted through the anaesthetic’s secretary (ext. 4550).
If the patient is deemed high risk, treatment will be arranged to be completed in the theatre recovery area (on B level), so that rapid intervention may occur should complications occur.
The ECT nurse should arrange this once the anaesthetist has made the decision by ensuring the other theatre staff are aware (the anaesthetist may inform them) and the ward staff where the patient is due to attend treatment from. High risk patients are usually treated first on the list for that day, but this may be negotiated with the anaesthetist, other patients and the wards should be informed that the start of treatment may be delayed and stagger arrival times appropriately.
Patients should be transported to theatres either on a bed or in a wheelchair (the bed should have a removable headboard and be able to be lowered rapidly, ECT chair beds can be used if appropriate) with the appropriate escort and paperwork. If there are difficulties in finding an appropriate bed the moving and handling coordinator from Rotherham General NHS Trust can be contacted for assistance on 4314 or bleep 153. The ECT nurse will need to bring the trolley from the ECT suite with the following on it; Thymatron IV, ECG pads, contact gel, mouth gag, spare paper for the Thymatron. The medications and cannula should be available in the theatre recovery area. If treating in theatres only one ECT nurse is required to attend as a patient should be fully recovered prior to treating another patient in that area, the other ECT nurse may wait in the department as patients may arrive early to be treated in the ECT suite. The treatment will commence in the same way as conducted in the ECT suite, although the equipment checks will be completed by the theatre staff.
11.8 Appendix H Protocol 8, ECT protocol for stimulus dosing for Thymatron machine, the quality and timing of a seizure, EEG monitoring and re-stimulation following a brief or missing seizure
11.8.1 General Aims
- An operational definition of the seizure threshold is ‘the minimum amount of electrical charge (as a %) that will induce a classical generalised tonic-clonic convulsion at the first or second treatment in a course of ECT
- The aim is for the dose of electrical charge in subsequent treatments to be clearly supra-threshold.
- The only exception to these general aims is where treatment is started to save life. It is recommended that, in these cases, the seizure threshold be estimated and treat with a supra-threshold dose for maximum effect. If possible, discuss with lead ECT consultant.
11.8.2 Titration of seizure threshold
11.8.2.1 Patients not taking anti-epileptic drugs
The first stimulation at the first treatment will routinely be 10%. If the necessary convulsion is not induced after 20s, stimulation will be repeated with a dose of 15%. If the necessary convulsion is not induced after the second stimulation, the third stimulation should be increased to 35%. Assuming that 35% led to the necessary convulsion at the first treatment, the titration procedure can be continued at the second treatment session by applying 20% at the first stimulation, and, if the necessary convulsion is not induced, increasing the dose to 25% at the second stimulation. If the necessary convulsion is still not induced, then the third stimulation should be 45% for bilateral ECT and 120% for unilateral ECT (the seizure threshold must be at least 30 %.) See the worked example below.
11.8.2.2 Patients taking anti-epileptic drugs
The absolute values and range of stimulation at the first treatment should be higher than those applicable to patients not taking such drugs: that is, 20%, 40% and 60%. At the second treatment, the titration process can continue between the lower stimulation that did not lead to a convulsion and the higher stimulation that did.
11.8.2.3 Calculation of the seizure threshold
Ideally, the dose that did not induce the necessary convulsion will be only 5% less than the dose that did. Although the actual seizure threshold will lie between these two values, it is sufficient to take the upper value as the seizure threshold (see note 2).
11.8.2.4 Dosing strategy
Once the seizure threshold has been established at the first or second treatment, then the dose must be increased at the next treatment session to exceed the threshold as follows:
- for bilateral ECT, the dose should exceed the seizure threshold by 1.5 times the seizure threshold
- for unilateral ECT, the dose should be 4 times the seizure threshold
- the only exception to these general rules is the patient who displayed the necessary convulsion with only 10% and is to be treated by unilateral ECT. It will be sufficient to increase the dose by only 3 times
11.8.2.5 Adjusting the dose throughout a course of treatment
This may be indicated for the following reasons:
- repeated ECT can lead to a rise in the seizure threshold, and a dose that initially induced the necessary seizure may fail to do so later in the course. A higher dose will therefore be required. It is sometimes said that a progressive shortening in convulsion length means that the seizure threshold is rising; this is not invariable. In such circumstances it is vital that the ECT team finds out from the referring team how well the patient is progressing; if improvement is absent or slight, then it may be entirely reasonable to increase the dose
- the initial dosing strategy brings about only slight or no clinical improvement. Doses of up to 2.5 times the seizure threshold may be indicated in bilateral. ECT and doses up to 6 times seizure threshold in unilateral ECT
- significant treatment emergent cognitive side-effects may be an indication to reduce the electrical dose. Please discuss with ECT lead psychiatrist (see note 3)
11.8.3 Failure to induce a convulsion
During a course of treatment, stimulation may fail to induce a convulsion if there has been a marked rise in the seizure threshold (see above) or because of a change in a variable that independently alters the seizure threshold (for example, Use of anti-epileptics or change in anaesthetic technique). It is essential to repeat stimulation with a higher dose. If it is desirable to establish the new, higher, seizure threshold, then a small increase in dose is appropriate, for example, 5 or 10%. (Thymatron doses) But if the patient is severely ill, it is not desirable to treat with a dose close to threshold; it is better to estimate that the new seizure threshold is 5 or 10% higher (Thymatron doses) dose that did not lead to a convulsion, and then use this estimate to calculate the dose for re-stimulation as per the dosing strategy above.
11.8.3.1 Note 1
The question is sometimes asked how best to proceed when a patient has been treated previously by ECT. The following protocol is suggested:
- 3 or more months since last treatment, titrate as above
- 2 weeks to 3 months since last treatment, titrate as for patients on anti-epileptic drugs
- 2 weeks or less since last treatment, dosing should continue as if no break had occurred
11.8.3.2 Note 2
Before deciding how to dose the patient, you must ask yourself what you believe the patient’s seizure threshold to be on that day and before you stimulate the patient. It may be helpful to record the seizure threshold on the treatment record (for example, ST equals 20%) 40.
11.8.3.3 Note 3
Both inadequate clinical improvement and treatment-emergent cognitive side effects may affect the choice of electrode placement. Patients who do not recover from depressive illness with high dose unilateral ECT may subsequently recover with moderate-dose bilateral ECT. Prolonged disorientation is much less of a risk in unilateral ECT.
11.8.3.4 Note 4
The quality of a seizure is determined by direct observations of the fit and EEG record. Good seizure should be generalised, and EEG record shows 3 spikes and wave pattern per second. Current evidence suggests that the duration of seizure is no longer crucial once there is a demonstrable generalised seizure (as above).
| Level | % | Convulsion | Threshold |
|---|---|---|---|
| 1 | 10% 15% 35% | 0 0 41s Generalised convulsion | The seizure threshold lies between 15% and 35% |
| 2 | 20% | 19s Generalised convulsion | The seizure threshold lies between 15% and 20%, Taken as 20% |
| 3 | 30% | 45s Generalised convulsion | Dose = seizure threshold +50%. The convulsion induced by supra-threshold stimulation is longer |
| 4 | 30% | 43s Generalised convulsion | Content |
| 5 | 30% | 38s Generalised convulsion | Content |
| 6 | 30% | 19s Generalised Convulsion | Content |
Note reduction in length of convulsion at sixth treatment. Discuss with referring team whether or not there is an indication to increase dose.
Scott, Allan I.F. (2005) an example of a stimulus dosing protocol. The ECT Handbook. 2nd Edition. Royal College of Psychiatrists. London. Treatment Stimulation Convulsion Comments.
| Suggested start point | Level | % | mC |
|---|---|---|---|
| Female Uni or Male or Female under 40 | 1 | 5 | 25 |
| Female Bi or Male Uni | 2 | 10 | 50 |
| Male Bi | 3 | 15 | 76 |
| 4 | 20 | 101 | |
| 5 | 30 | 151 | |
| 6 | 50 | 252 | |
| 7 | 70 | 353 | |
| 8 | 100 | 504 | |
| 9 | 150 | 756 | |
| 10 | 225 | 1008 |
Bilateral, treatment dose 1 level higher.
Unilateral, treatment dose 3 levels higher.
The seizure will be monitored by the EEG on the Thymatron, the ECT nurse is responsible for ensuring that the monitoring is in place and there is sufficient paper in the machine. The ECT nurse should also time the observed seizure using a clock or watch with a second hand and report this to the consultant psychiatrist for documentation. Timing will begin at the end of the treatment sound from the Thymatron. The consultant psychiatrist will also document the quality of a seizure on the care record treatment sheet.
11.9 Appendix I Protocol 9, management of a prolonged or Tardive seizure
This is classed as a seizure lasting more than two minutes. The seizure should be terminated by either intravenous Diazepam or more anaesthetic agent. The anaesthetist will administer these drugs if so required. The ECT nurse should inform the anaesthetists at 90 seconds that action may be required in order to allow time to draw up the appropriate medications.
11.10 Appendix J Protocol 10, monitoring patients immediately after ECT and discharge criteria
11.10.1 Recovery
The anaesthetist will hand over the patient to the recovery nurse and check that they are satisfied with the patient’s condition (this will include documenting physical observations and any problems on the care record, as indicated). The escort nurse will remain with the patient in recovery and provide any assistance needed, including reassuring the patient as they wake up. The recovery nurse will decide when the patient is fit to transfer into the post recovery room with their escort. If the escort is concerned about their patient, they should ask the recovery nurse or ECT nurse (in pre-treatment) for assistance. Once the patient has rested and is fully conscious the escort can assist them to walk through to the final lounge, where the escort can make them a drink and some toast. Only the ECT nurse or recovery nurse may authorise for patients and escorts to leave the department (please bear in mind transport may take some time to arrive for Doncaster and Scunthorpe patients).
11.10.2 Discharge criteria
The following discharge criteria are in accordance with the guidelines from the British Association of day surgery handbook, the ECT department recommends that all inpatients remain at least 1 hour in the department following treatment. The patient will be assessed as to their fitness for discharge from the department by one of the lead ECT nurses using the following criteria:
- stable blood pressure and pulse for at least 1 hour
- no breathing problems
- fully awake and aware of their surroundings
- minimal nausea, vomiting, dizziness or headache
- can walk to ward or transport without feeling faint (wheelchair to be used only if used for arrival)
- has at least taken oral fluids but ideally food too
- accompanied by own escort (not a student)
If these criteria cannot be met, then the patient must be retained in the ECT suite and the consultant anaesthetist contacted to decide an appropriate course of action. Either the recovery nurse or ECT nurse can make the decision that the above criteria are met, and patients are fit for discharge from the ECT suite.
11.11 Appendix K Protocol 11, day or outpatient ECT
Anyone who is prescribed ECT as an outpatient must be referred by the consultant to the ECT department in the usual way but to also point out the escort arrangements (CPN) and supervision (member of family or carer at home 24 hours post treatment) and make arrangements for the doctor to assess the patient post treatment must also be discussed.
As with inpatients all pre-treatment investigation must be carried out, and the patient consented. Please see hyperlink in protocol 18 for the Royal College of Psychiatry updated patient information leaflet regarding ECT. The prescribing consultant will give the outpatient information leaflet to the patient and contact the nurse in charge of ECT to arrange for them to meet with the patient before treatment commences. This leaflet should also be given to and signed by the patient or their carer prior to every treatment. Anyone receiving treatment as an outpatient must be informed of the following verbally by the nurse in charge of the ECT suite as well as receiving it on the information sheet.
- Not to have anything to eat or drink from 3 am on the morning of treatment.
- Not to take any medication on the morning of treatment, but to bring them and hand them to the nurse who will ensure they receive them following treatment.
- To report any physical illness, they may develop prior to treatment such as migraine or severe cold. If this is the case, they should contact the ECT suite and seek advice.
- They should not attend for treatment by driving themselves to the unit. If they are coming by car someone else should drive them there and back.
- They should discuss with their doctor and inform the DVLA of their mental state in order to assess their ability to drive.
- They must not return home alone to an empty house, so arrangements should be made for someone to be with them for 24 hours following treatment, for example, relative, friend, or neighbour.
- They should not sign any legal documents in the 24 hours following ECT.
- They are to arrive at the ECT department at 9am (unless other arrangements made by the ECT team).
- That on the day of treatment it is advisable that they wear loose fitting clothing and not to have on make up or jewellery.
When the patient arrives in the department, they will be greeted by the nurse in charge who will:
- check that the patient has had no diet or fluids since 3 am
- check the arrangements with the escort nurse for the patient’s return home, and transport is booked
- monitor and record the patient’s blood pressure, pulse, temperature and respiration
- advise the patient to empty their bladder and bowels prior to treatment
All the other procedures are to be followed as for inpatients.
Following treatment, the patient is not to be allowed to leave the department unless both the anaesthetist and doctor are satisfied that they are recovered enough to leave, and the doctor has assessed (or plans to on their return to a ward prior to returning home) their mental state and suicide risk. The ECT staff must ensure that the patient has a copy of the ECT information and agreement and has the relevant contact details of the ECT suite, GP and NHS direct. The crisis team telephone number may also be given if appropriate.
11.12 Appendix L Protocol 12, discontinuation of ECT and follow-up arrangements
11.12.1 Policy for discontinuation if there is no response
A set number of ECT treatments should not be prescribed at the start of a course of ECT as it is not possible to predict reliably how many treatments will be required in a course of ECT. The need for further treatment should be assessed after each individual treatment.
If no clinical improvement at all is seen after 6 properly given bilateral treatments, then it is highly unlikely that more treatments will bring about either significant improvement or eventual recovery hence the course should be abandoned (ECT Handbook, 2nd edition).
It may be worth continuing up to 12 bilateral treatments before abandoning ECT in patients who have shown definite but slight or temporary improvement with early treatments. There are some patients with depression who do not respond to high-dose right unilateral ECT, but who subsequently respond to bilateral ECT. The ineffective unilateral treatments should be disregarded in the assessment of need for further bilateral treatments. (ECT Handbook, 2nd edition).
It is essentially the patients’ consultant psychiatrist who makes the decision to discontinue treatment. However, if there are concerns regarding the patients’ mental state, physical state or level of side effects the nominated deputy may suspend treatment pending a review. The ECT Consultants may also do this, or feedback to the team any concerns regarding further treatment in the patients’ notes or via telephone. The reason why treatment has been discontinued should be documented on the care record (page 26) and in the patients’ notes. The patients’ orientation and memory should be assessed and documented in a clinical interview and the outcome of treatment recorded at the end of treatment.
11.12.2 Follow up arrangements
The patient should be re-assessed by the consultant psychiatrist or nominated deputy at 3, 6 and 12-months post treatment, including clinical status, memory and cognitive functioning. Ideally there should also be a record of the patients’ subjective experience of treatment side effects and objective side effects at such intervals, for example, through the use of a memory diary.
11.13 Appendix M Protocol 13, treatment of elderly patients
When ECT is considered for an elderly person, all coexisting medical and surgical conditions should be assessed and, where possible, stabilised or treated prior to ECT.
As there is an increased likelihood of high seizure thresholds among elderly people, the anaesthetist needs to take this and other age-related factors into account in the choice of anaesthetic agent. The seizure-shortening effect of Propofol and its effect on seizure threshold will need to be taken into account in the choice of an anaesthetic agent.
The medical and nursing staff need to closely monitor older people who are receiving ECT. This monitoring should include paying close attention to possible changes in their physical state and cognitive function during a course of treatment. There should be regular routine exchange of information between the team caring for the patient who is being treated with ECT and the ECT team.
The ECT technique should be modified as necessary to minimise any cognitive adverse effects during ECT
11.14 Appendix N Protocol 14, treatment of children and young people
11.14.1 Introduction
Although ECT for patients under 18 is extremely rare, there have been occasions when ECT has been given to such patients in this country. The essential indications are the same as for adults.
The Mental Health Act (1983) (DoH, 2008) indicates that ECT for a person under the age of 18 should be given ECT under section 58A, requiring the approval of a second opinion appointed doctor (SOAD), whether they are detained or not. That is that a SOAD must certify that treatment is appropriate. Unless it is an emergency, no child or young person under the age of 18 may be given ECT without the approval of an SOAD, even if they have consented to it.
Capacity should also be certified by the SOAD, if a person is capable of consenting, they cannot be given treatment without such consent, unless it is an emergency. The above also applies to young people of 16 or 17 who are not detained and lack the ability to consent for themselves, except where the MCA may be used to provide the necessary authority, however a SOAD certificate will still be required. For children and young people under the age of 18, a SOAD certificate by itself is not sufficient to authorise the treatment, unless they are detained. Clinicians must have the patients’ own consent or some other legal authority.
Please note, “there is nothing in the act itself to prevent a person with parental responsibility consenting to ECT on behalf of a child or a young person who lacks the ability to consent for themselves and who is neither detained nor an SCT patient. However, although there is no case law at present directly on this point, it would not be prudent to rely on such consent, because it is likely to lie outside the parental zone of control. Therefore, if a child under 16 who is not detained or an SCT patient needs ECT, court authorisation should be sought, unless an emergency. This should be done before a SOAD is asked to approve the treatment.” (DoH, 2008, page 341, 36.59 to 36.60).
11.14.2 Dosage settings
The first stimulus should be given with the minimum dosage, which should be 5%. The principles in the “stimulus dosing protocol” should then be followed. If ECT treatment is to be given to a patient under 18 years old, then the lead consultant for ECT should be involved at the earliest opportunity. The treatment will also need to be arranged with the ECT team to occur separately from session involving adults.
11.15 Appendix O Protocol 15, consultation between the ECT consultant and the referring psychiatrist in situations where ECT is prescribed outside of NICE guidelines
Every effort should be made to prescribe ECT within NICE guidelines (2003; 2009) as health professionals are expected to take NICE guidance fully into account when exercising their clinical judgement.
Divergence from NICE guidance would require:
- a detailed documented assessment of potential risks and benefits of treatment to which a valid consent has been obtained
- obtaining a second opinion from an independent psychiatrist when the indication for ECT is potentially controversial or where any variance from NICE guidance is being considered. The patient may also be able to express a clear view about the perceived severity of the illness and the role of ECT in its treatment and this should be documented
- it would be prudent to be particularly careful to discuss the topic of retrograde amnesia, particularly for personal memories, and to document this discussion
- where appropriate the treatment should be discussed with the patient’s guardian or carer and this should be documented
The consideration for prescribing ECT outside NICE guidance should be discussed with ECT consultant or associate ECT consultant. During the course of treatment, the patient’s response to treatment and side effects should be rigorously assessed at least weekly.
The prescribing consultant and the ECT consultant or associate ECT consultant should discuss fortnightly the patient’s progress or side effects and need to continue treatment. This should be done either by face-to-face discussion where practicable or by phone. The discussion should be clearly documented
11.16 Appendix P Protocol 16, storage of Dantrolene
A box of Dantrolene is stored in the locked medicine cupboard in ECT. This should be checked for expiry as the weekly checks are completed by the ECT nurse.
If the Dantrolene is damaged in any way the nearest supply is in theatres on B level, staff can telephone them and request a supply be brought to the department in an emergency.
11.17 Appendix Q Protocol 17, equipment list
11.17.1 Equipment list
11.17.1.1 Pre-treatment room
- PACS and PAS computer (serial, 21370, IT 04647).
11.17.1.2 Treatment room
- Thymatron System 4 (DRI serial, 5390).
- 1 double flaw meter plus suction.
- Welch Allyn Propaq (serial, 094 168).
- Micro-stream portable capnograph (serial, 093656).
- Medication storage fridge.
- Eschman suction machine VP45 (serial, 034771).
11.17.1.3 Recovery room
- Welch Allyn Propaq CS (serial, 094168).
- Datascope Accutor plus.
- Suction unit X2 (serial, 218 376).
- Power Heart G5 cardiac science G5S 02PO.
- Codemaster defibrillation machine (serial, 18284).
- 1 double flow meter and suction.
- 2x size oxygen
11.17.1.4 Post recovery
- Head surgery chair x4 (serial, 218377, 218471, 218555, 218622).
- Eschman suction machine VP45 (serial, 031364).
- Eschman suction machine VP45 (serial, 031364.
- 1 flow meter oxygen.
11.18 Appendix R Protocol 18, patient Information checklist
Document control
- Version: 6.
- Unique reference number: 383.
- Approved by: Clinical policy review and approval group.
- Date approved: 6 April 2021.
- Name of originator or author: Lead ECT consultant or ECT lead clinician associate or lead ECT consultant or lead ECT anaesthetist or lead ECT recovery nurse or lead ECT operating department practitioner.
- Name of responsible individual: Rotherham care group director.
- Date issued: 24 May 2021.
- Review date: April 2024.
- Target audience: Clinical staff who work within the ECT department, including staff from the Rotherham older peoples services who provide cover through a service level agreement and any staff responsible for escorting patients to receive ECT treatment.
Page last reviewed: April 22, 2024
Next review due: April 22, 2025