Contents
1 Introduction
1.1 Background
Evidence of the damage caused to health by smoking tobacco is overwhelming and irrefutable. Smoking is a major cause of disease killing one out of every two smokers. Tobacco use is a significant problem that affects us all. It affects our health, our wealth and our safety. Smoking is the largest cause of preventable death in England. In 2016 there were estimated to be 77,900 deaths attributable to smoking, this represents 16% of all deaths (NHS Digital, 2018). Around one in four people in England experience a mental health condition in any one year, most commonly being anxiety and depression. Although mental health conditions vary widely, there is long-standing evidence that smoking prevalence is substantially higher among most mental health conditions, and increases with the severity of the condition.
Adults with mental health problems, including those who misuse alcohol or drugs, smoke 42% of all the tobacco used in England. Many wish to stop smoking, and can do so with appropriate support (DoH, 2011). The most common diseases caused by smoking include coronary heart disease, lung cancer, chronic bronchitis, emphysema, pneumonia and chronic obstructive pulmonary disease (COPD). It can also cause illnesses including mouth, nose, throat, oesophagus and larynx cancer, strokes, decreased fertility, gangrene leading to amputations, and premature ageing.
As of the 1st July 2007 smoking in England was banned in virtually all enclosed public spaces, workplaces, public vehicles and employer owned vehicles used for work purposes. The law applies to almost all substances that can be smoked, including cigars and herbal cigarettes. In 2013 Department of Health (DoH) and The National Institute for Health and Care Excellence (NICE) recommended that hospitals should be smoke free outside as well as inside. It was also recommended that facilitation of the smoking breaks should no longer be allowed and patients who smoke should be offered treatment.
In line with the guidance PH48 issued by NICE (2013), the Rotherham, Doncaster and North Humber NHS Foundation Trust (trust) will operate a policy that positively promotes a smoke free environment and thereby health and wellbeing for all. The trust will provide support and treatment to smokers who wish to quit and support smokers who do not want to quit to temporarily abstain or reduce harm from tobacco use whilst in trust premises and vehicles used for the purposes of patient transport.
1.2 Legal position
There is a legal duty of care placed on the trust to put in place reasonable arrangements for the improvement of the health of patients and staff and the trust acknowledges that breathing other people’s smoke is both a public health hazard and welfare issue, proven to cause ill health. This policy recognises that second-hand smoke may adversely affect the health of all staff and patients. This policy relates to where a person is smoking and the effect this may have on patients, visitors, trust staff, contractors and other members of the wider health community who may be on trust premises.
Section 2 of the Health and Safety at Work Act 1974 places a duty on employers to:
- ‘…provide and maintain a safe working environment which is, so far as is reasonably practical, safe, without risks to health and adequate as regards facilities and arrangements for welfare at work.’
The Health Act (2006) states that:
- ‘the appropriate national authority may make regulations designating as smoke free any place or description of place that is not smoke-free…”
The trust derives its power from the NHS as an appropriate national authority and thereby makes this Smoke free policy; prohibiting smoking in trust premises for example. buildings, grounds and trust vehicles.
Ban on tobacco products is considered separately from the blanket restriction policy because a range of alternative nicotine containing products is offered to patients and staff to manage withdrawal (see section 5.2).
1.3 Legislation and guidance
This policy reflects the following legislation and guidance:
- Health Act 2006 (opens in new window)
- The Smoke-free (Premises and Enforcement) Regulations 2006 (opens in new window)
- Health matters: smoking and mental health Public Health England guidance 2020 (opens in new window)
- Smoke-free generation: tobacco control plan for England 2017 (opens in new window)
- Tobacco control plan: delivery plan 2017 to 2022 (opens in new window)
- The health effects of exposure to second hand smoke ASH Report (2014) (opens in new window)
- The Care Quality Commission Brief guide for inspection teams: smoke free polices in mental health inpatient services (2017) (opens in new window)
- E-cigarettes: a new foundation for evidence-based policy and practice (2015) (opens in new window)
- Pharmacy Guidance on Smoking and Mental Disorder (2017) (opens in new window)
- Public Health England guidance on use of e-cigarettes in public places and work places: Advice from evidence based policy making (2016) (opens in new window)
- NSCST Smoking Cessation and Mental Health: A briefing for frontline staff (2014) (opens in new window)
- NICE Guidelines. Tobacco: preventing uptake, promoting quitting and treating dependence (in draft as of November 2021) (opens in new window)
2 Purpose
The purpose of this policy is to raise clinical staff awareness, and set out the responsibilities of trust staff to ensure compliance relating to the legislation on smoke free environments. This will:
- enable all staff, patients and visitors to the trust premises to benefit from a sensible approach to a smoke free environment
- protect patients, visitors, staff and others from potential health risks associated with second hand smoke inhalation whilst on trust premises
- protect staff from exposure to smoke when making home visits
- provide opportunities and support to patients and staff who wish to give up smoking
- support inpatient smokers to help them cope and comply with increased restrictions or to stop smoking by providing free nicotine replacement and behavioural support
- give authority to staff as part of implementing this policy to carry out random, routine or dedicated searches aimed at maintaining a smoke free environment, this means that all patients with unescorted access (including informal patients) will on return to the ward may be subject to a rub down search at nurse in charge discretion, please refer to the searching of a person or their property policy
- identify and minimise fire risks within trust premises
In addition this policy seeks to:
- comply with Health Act 2006
- comply with the smoke free regulations which commenced on 1st July 2007
- comply with Health and Safety at Work Act 1974
- provide a safe and healthy working environment and protect the current and future health of staff, patients and visitors
- observe the right of everyone to breathe in air free from tobacco smoke
- raise awareness of the hazards associated with exposure to tobacco smoke
- take account of the needs of those patients who choose to smoke and to support those who wish to stop
3 Scope
This policy applies to all staff, patients who are in an episode of treatment, visitors, and other persons, whilst they are on trust premises.
3.1 Exclusions
The Health Act 2006 states that “The appropriate national authority may make regulations providing for specified descriptions of premises, or specified areas within specified descriptions of premises, not to be smoke-free”.
The trust derives its power from the NHS as an appropriate national authority and thereby allows the premises of St John’s Hospice to be excluded from the smoke free policy when it comes to the in-patients of the service. For patients at the end of life, smoking abstinence or cessation may cause unnecessary distress and may not be worthwhile when balanced against the severity of their clinical condition. At the same time, all patients of the St John’s hospice can access the in-house QUIT smoking cessation service if they wish.
This policy applies to staff and visitors of St John’s hospice, meaning they should not smoke or consume any other tobacco products on the premises.
3.2 Definitions
- Trust, wherever stated, this means Rotherham, Doncaster and South Humber NHS Foundation Trust.
- Patient, means service user, patient and or client.
- Visitor, any individual coming to the trust premises either to visit a patient, use trust facilities or grounds, or working as a contractor.
- Staff, individual employed by RDaSH, including on the part-time, fixed terms and bank bases.
4 Responsibilities, accountabilities and duties
4.1 The chief executive and board of directors
The chief executive and board of directors are responsible for ensuring that the trust has policies and procedures in place to support best practice, the management of associated risks and compliance with all legislation which is applicable to the trust. The chief executive has overall responsibility for the health, safety and welfare arrangements of the trust and compliance with legislation. The director who is accountable with responsibility to ensure implementation of this policy is the chief operating officer.
4.2 Care group directors, modern matrons and deputy care group directors or service managers
The Health Act 2006 section 8 and sub section 1 states that ‘It is the duty of any person who controls or is concerned in the management of smoke free premises to cause a person smoking there to stop smoking’ and therefore directors, care group directors and deputy care group directors managers are responsible for:
- raising clinical staff awareness of this policy and maintain effective communication of the policy to all staff
- ensuring that ward or treatment teams screen every patient within 24 hours of admission or community service registration and record the status on SystmOne
- maintaining a safe, healthy working environment through implementation and compliance with this policy
- address, note and take relevant action regarding concerns raised by staff that individual requirements or circumstances are not being met in relation to this policy
- ensure that necessary risk assessments are completed when staff report that they are being subjected to passive smoking which includes staff who visit patients in their own home or community based residence
- take appropriate action where patients, visitors staff do not comply with this policy
- ensure that patients are aware of and have access to advice and support to either manage their personal smoking habits or to stop smoking
4.3 All trust staff
It is the responsibility of all trust staff to:
- comply with and implement the requirements of this policy. It is of vital importance that all staff see the beneficial aspects of this policy in order to be able to comply with its implementation
- report promptly to their manager any circumstances which have resulted in them being subjected to passive smoking in the course of their duties, which includes visiting patients in their own home or community based residence. Staff should request from patients who are smokers that they have their last cigarettes an hour prior to scheduled visits and appointments. Such an agreement will be recorded as part of the treatment plan
- desist from turning a blind eye when a patient is found smoking on trust premises
- take steps to prevent ignition sources (such as lighters and matches) and smoking paraphernalia being brought into the trust premises
- report any incidents of non-compliance in relation to any aspect of this policy to their line manager and via the trust IR1 incident reporting system
- be aware that non-compliance with any particular element of this policy may amount to active lack of care or negligence, a breach of duty of care and therefore constitute a wilful or intentional failure to obey a lawful and reasonable request and may result in disciplinary action, in accordance with the trust’s disciplinary policy
5 Procedure or implementation
5.1 General approach
All trust staff will promote a smoke free environment and healthy living. The trusts expectation is to promote and develop a culture across all its premises that smoking is unacceptable and that everyone respects this.
NICE (2021) recommends strong leadership and management to ensure that trust premises remain smoke free to help to promote non-smoking as the norm for people using the trust services. Within St. John’s Hospice, where patients are exempt from smoke free legislation Health Act 2006, the management team should reduce, where possible, incidences of staff being exposed to second hand smoke.
It is recommended that where staff approach a patient, or visitor to inform them of the trust policy, this approach must be made only once in order to avoid escalation of conflict. The information provided should be limited and along the lines of ‘can I make you aware that this is a smoke free trust within both the hospital and grounds.’ Breaches can be reported via IR1 system with a brief explanation of the circumstances and outcome (see section 8).
A zero tolerance approach will be applied to any individual who becomes abusive when reminded of the smoke free policy. Staff are expected to adheres to the principles taught in the trust’s conflict resolution and reducing restrictive interventions training courses.
Should the person become aggressive then the member of staff is to distance themselves from the situation (walk away) and seek support from their line-manager. All smoke free policy breaches must be reported as explained in section 8 of this policy.
5.2 Prohibited and permitted items
Patients and visitors on trust premises will be made aware of the smoke free policy through signs, posters, and leaflets as well as conversations with staff. Patients and visitors will be provided with a list of the contraband items in the hospital which includes tobacco, cigarettes, lighters, matches and counterfeit or tampered with electronic cigarettes or their components.
Any visitor who is found to be supplying a patient in hospital with contraband items will be reminded about the relevant policy and asked to support the patient’s treatment plan. Persistent offenders may be banned from visits in the future. The rationale for the smoke free policy will be explained and carers will be offered support to learn more about the harmful effects of tobacco dependence. If appropriate they will be directed towards their local stop smoking service.
This Policy prohibits cigarettes, cigars, pipes, roll-ups, ignition sources and any form of smoking paraphernalia from being kept on the ward by staff or on themselves for the purposes of facilitating smoking for themselves, patients or visitors.
The permitted and prohibited items on the RDaSH premises table summarises permitted and prohibited items. If you are unsure about a specific product, contact the QUIT team on rdash.quit@nhs.net for guidance.
Appendix E provides extended information on managing and risk assessment of the non RDaSH supplied chargeable electronic cigarettes on the inpatient units.
| Items | Inpatients |
|---|---|
| Patches | Yes (product is supplied free of charge by RDaSH for this group, contact rdash.quit@nhs.net) |
| Lozenges and mini-lozenges | Yes (product is supplied free of charge by RDaSH for this group, contact rdash.quit@nhs.net) |
| Tabs and micro-tabs | Yes |
| Inhalators | Yes (subject to risk assessment) (product is supplied free of charge by RDaSH for this group, contact rdash.quit@nhs.net) |
| Gum | No |
| Spray | Yes |
| Disposable electronic cigarettes | Yes (subject to risk assessment) |
| Chargeable electronic cigarettes | Yes (subject to risk assessment) |
| Cigarettes and cigars | No |
| Roll-ups | No |
| Smokeless tobacco (snuff, chewing) | No |
| Shisha and pipe | No |
| Items | Outpatients |
|---|---|
| Patches | Yes (product is supplied free of charge by RDaSH for this group, contact rdash.quit@nhs.net) |
| Lozenges and mini-lozenges | Yes (product is supplied free of charge by RDaSH for this group, contact rdash.quit@nhs.net) |
| Tabs and micro-tabs | Yes (product is supplied free of charge by RDaSH for this group, contact rdash.quit@nhs.net) |
| Inhalators | Yes (subject to risk assessment) (product is supplied free of charge by RDaSH for this group, contact rdash.quit@nhs.net) |
| Gum | Yes (product is supplied free of charge by RDaSH for this group, contact rdash.quit@nhs.net) |
| Spray | Yes (product is supplied free of charge by RDaSH for this group, contact rdash.quit@nhs.net) |
| Disposable electronic cigarettes | Yes |
| Chargeable electronic cigarettes | Yes |
| Cigarettes and cigars | No |
| Roll-ups | No |
| Smokeless tobacco (snuff, chewing) | No |
| Shisha and pipe | No |
| Items | Visitors |
|---|---|
| Patches | Yes |
| Lozenges and mini-lozenges | Yes |
| Tabs and micro-tabs | Yes |
| Inhalators | Yes |
| Gum | Yes |
| Spray | Yes |
| Disposable electronic cigarettes | Yes |
| Chargeable electronic cigarettes | Yes |
| Cigarettes and cigars | No |
| Roll-ups | No |
| Smokeless tobacco (snuff, chewing) | No |
| Shisha and pipe | No |
| Items | Staff |
|---|---|
| Patches | Yes (product is supplied free of charge by RDaSH for this group, contact rdash.quit@nhs.net) |
| Lozenges and mini-lozenges | Yes (product is supplied free of charge by RDaSH for this group, contact rdash.quit@nhs.net) |
| Tabs and micro-tabs | Yes (product is supplied free of charge by RDaSH for this group, contact rdash.quit@nhs.net) |
| Inhalators | Yes (product is supplied free of charge by RDaSH for this group, contact rdash.quit@nhs.net) |
| Gum | Yes (product is supplied free of charge by RDaSH for this group, contact rdash.quit@nhs.net) |
| Spray | Yes (product is supplied free of charge by RDaSH for this group, contact rdash.quit@nhs.net) |
| Disposable electronic cigarettes | Yes (non-work time only) (product is supplied free of charge by RDaSH for this group, contact rdash.quit@nhs.net) |
| Chargeable electronic cigarettes | Yes (non-work time only) |
| Cigarettes and cigars | No |
| Roll-ups | No |
| Smokeless tobacco (snuff, chewing) | No |
| Shisha and pipe | No |
5.3 Community services
5.3.1 Assessment
As part of the initial assessment into a treatment service, patients are to be asked a range of questions on their smoking habits and record of the above is to be made in the patient’s clinical record on SystmOne in the designated RDaSH smoking template, accessible through the RDaSH MH assessment launchpad (see appendix G). The questions on the template cover:
- if they are a tobacco user and, or if they use an e-cigarette
- if they have ever tried to quit smoking or stop using tobacco in the past
- if yes, what methods did they use (for example, NRT, medications or electronic device), how long did they quit for, what prompted them to start smoking or using again
- if they have never tried to quit before ask what has stopped them in the past
- all patients who smoke or use tobacco products are to be referred for in-house smoking cessation support unless they ‘opt-out’
Important notice, all community patients are to be screened on registration or at least annually, including non-smokers.
5.3.2 Referrals and treatment
Throughout their episode of treatment the patient’s smoking status should be reviewed at regular intervals (at least yearly), and for patients subject to a care programme approach (CPA) this review should be done as part of their CPA reviews.
Where available, community staff are to carry a small supply of health promotional material in relation to in house and local smoking cessation services, and inform patients of the fact that the inpatient services are smoke free.
Where the patient is likely to have contact with inpatient services they are to be reminded of the fact that all local hospitals are smoke free and advised that all smokers in our care are now routinely identified, that they will be assessed for their tobacco dependency and will be supported to manage nicotine cravings whilst they are in the care of the trust.
All community patients who smoke should be offered help with smoking cessation. With the patient’s consent, they should be referred to the appropriate smoking cessation service (see section 5.3.2.1).
5.3.2.1 Referral routes for RDaSH community patients who opt into receive smoking cessation support
Doncaster and Rotherham:
- option 1, in-house QUIT service by either:
- using a referral form on SystmOne (see appendix I)
- Email: rdash.quit@nhs.net
- option 2, External Yorkshire Smoke free service by contacting:
- Telephone: 0800 612 0011 or 0330 660 1166
- Email: swy-tr.y-smokefree@nhs.net
- option 2, external Get Healthy Rotherham service by contacting:
- Telephone: 01709 718720
- Email: parkwood.gethealthyrotherham@nhs.net
If option 1 is not available or patient explicitly states they would like to be supported by an external service.
North Lincolnshire:
- North Lincolnshire Healthy Lifestyles Service by contacting:
- Telephone: 01724 298212
- Email: nlc.healthylifestyles@hs.net
5.3.3 Visiting patients who smoke in their own homes
All staff visiting or treating a patient in the patient’s home should make a request that a smoke free environment is provided for the duration of the visit. Where first appointments are provided in writing this request should be made in the text of the appointment and an information leaflet should be sent with the letter (see appendix B). When making appointments by telephone a verbal request is to be made for the patient not to smoke whilst any member of trust staff is working within the patient’s home environment.
If any patient receiving treatment from our trust in their own home struggle to comply with the requirements of this policy consideration needs to be given as to whether or not arrangements need to be put in place such as:
- will they agree that in the hour leading up to their appointment they will smoke in an alternative room to the one being used to for the home visit
- use of nicotine patches prior to and during the consultation or treatment episode
- the need for the patient to attend an alternative venue such as a clinic for their appointments rather than being seen in their own home
Detail of any alternative arrangements will be included in the patients care plan.
For any patients in the community who persistently fail to comply with this policy a review will be undertaken by the clinical team to agree appropriate next steps taking account of the patient’s treatment programme and risk assessment.
5.4 Inpatient services
5.4.1 Admission and assessment
With the exception of the hospice, all of the trust inpatient wards are smoke free. This includes the mental health wards. According to NICE (2013), the episodic nature of mental health conditions can impact on a person’s ability or willingness to stop smoking. However, in a smoke free secondary care environment, mental health patients will be subject to enforced abstinence, even during an acute phase of illness, and will need help to abstain.
Within 24 hours of every admission or-readmission, all patients are to be asked a range of questions on their smoking habits and record of the above is to be made in the patient’s clinical record on SystmOne in the designated RDaSH inpatient smoking screening questionnaire (please note, this is different from the community RDaSH smoking template) accessible from the patient record (see appendix I). The questions on the template cover:
On admission patients are to be informed of the trust’s smoke free policy, and, as part of the initial assessment the admitting or assessing clinician will establish the following:
- if the patient is a smoker or tobacco user and, or uses a E-cigarette
- if they have ever tried to quit smoking or stopped using tobacco in the past in the past
- if yes, what methods did they use, how long did they quit for, what prompted them to start smoking again
- if they have never tried to quit before ask what has stopped them in the past
- all patients who smoke are to be offered abstinence support (NRT or e-burns) and, where available, a referral to the trust’s smoking cessation QUIT service. Until such service is available, patients will be referred to the community service on discharge, as specified in section 6.1
- staff should contact the QUIT programme team on rdash.quit@nhs.net if they are unsure of the appropriate referral pathway
The above discussion is to be recorded in the patient clinical records on SystmOne.
Important notice, all inpatients are to be screened within 24 hours of admission or readmission, including non-smokers.
In all cases of planned inpatient admission, information regarding the trust status as a smoke free organization and banned items list will be given in advance to the patient and their identified next of kin or carers or visitors.
At admission patients are to be asked if they have any cigarettes, tobacco products, rechargeable e-cigarettes, chargers and ignition sources on them. Where found, these are to be removed from the patient and securely stored until the patient is either able to make arrangements for their relatives to remove these items from the ward or is discharged from the ward. In the event of a patient refusing to hand over any of these items that they have with them, staff are to refer to the searching of a person or their property policy.
The use of approved disposable E-cigarettes (e-burns) or Nicotine Replacement Therapy should be offered as part of the admission process. Staff should provide brief advice to patients on a regular basis. Please note that e-cigarettes cannot be used by pregnant women or anyone under the age of 18.
The QUIT approach is to be adopted when discussing smoking with a patient:
- Q, ask the question and record smoking status
- U, understand the level of their addiction (for example use Fagestrom test on assessment)
- I, inform the patient of personal health benefits in quitting
- T, treatment initiation by offering abstinence support and referral to the appropriate services, either within the trust or in the community
Where patients decline this opportunity they must be advised to remain abstinent from smoking tobacco products whilst on trust premises. For all smokers a care plan is to be put in place which details how they will be supported to remain abstinent during their episode of inpatient care.
5.4.2 Referrals and treatment
5.4.2.2 Referral and treatment routes for inpatients
The trust recognises that patients who smoke may need support to comply with this policy. Therefore those patients identified as smokers will be offered nicotine replacement therapy and, or disposable e-cigarettes.
All inpatients in Doncaster and Rotherham care groups will be referred to the inpatient QUIT smoking cessation service on the opt-out basis. Inpatients in the North Lincolnshire can group will be referred to the North Lincolnshire healthy lifestyles service on the opt-in basis.
Below summarises the referral routes for the inpatients in all care groups.
Specialist services (QUIT or another) will provide behavioural support and pharmacotherapy planning for abstinence or smoking cessation. Ward staff remain responsible for the daily management and issuing of the NRT or e-cigarettes during the in-patient stay.
Doncaster (opt-out) and Rotherham (opt-out):
- option 1, in-house QUIT service by either:
- using a referral form on SystmOne (see appendix I)
- Email: rdash.quit@nhs.net
North Lincolnshire (opt-in):
- North Lincolnshire Healthy Lifestyles Service by contacting:
- Telephone: 01724 298212
- Email: nlc.healthylifestyles@hs.net
5.4.2.3 Trust-supplied nicotine replacement therapy
The mainstay of inpatient NRT (nicotine replacement therapy) provision is the regular use of NRT patches to provide a baseline nicotine level with the addition of either PRN (as required) nicotine lozenges, inhalator or mouth spray to manage additional craving. Patients should be assessed to follow either a smoking cessation pathway or a nicotine replacement pathway through the course of their admission.
To facilitate this, nicotine replacement therapy will be available on all inpatient wards to be provided from the earliest appropriate time following admission.
While there is a wide variety of NRT available, due to the practicalities of ward storage and the need for accessibility it has been agreed within the trust that the range will be limited to NRT patches, inhalators, lozenges (2 strengths) and mouth spray.
5.4.2.4 Trust-supplied disposable e-cigarettes
The trust provides a range of disposable e-cigarettes free of charge to the inpatient service users during their stay. These may be different brand (E-burn, Dinner Lady, Logic Pro or another). The brand or type of disposable devices may very between different inpatient units.
Each ward will order e-cigarettes via purchasing. When the stock arrives onto the ward the number of e-cigarettes is to be entered into the stock book.
When an e-cigarette is given to a patient the following details are to be entered onto the patient’s drug card or at least into the stock book:
- date
- patient name
- name and signature of the staff member giving the e- cigarette to the patients
- number of e-cigarettes that remain in the ward stock
As each patient will have been asked at the point of admission how many cigarettes they smoked per day on average staff will know if anyone is over using the e-cigarettes
important note, depending on the level of addiction, a specific combination of NRT products and e-cigarettes will be recommended. All protocols are detailed in the RDaSH guidelines for nicotine management therapy and attached units, available on the intranet (opens in new window) (staff access only).
Or though the QUIT team by contacting rdash.quit@nhs.net.
Section 5.4.3 provides a summary of the processes associated with assessment, smoking cessation and abstinence support at RDaSH.
5.4.3 Ward use of nicotine replacement
5.4.3.1 Patient assessment
Section 136 suite:
- initial assessment of need
- offer following dose
- 21mg per 24 hours if patient smokes more than 10 cigarettes per day
- 14mg per 24 hours if patient smokes less than 10 cigarettes per day
- use recorded on the form PRN Nicotine replacement therapy NRT record of use
Screening by nursing staff within 24 hours and issuing of the NRT or e-cigarettes.
- Initial assessment of smoking status and supply of NRT patch and PRN.
- Daily assessment of need, supply of NRT patch and PRN.
- Full smoking cessation assessment for patient to either cessation pathway or NRT maintenance pathway. Consideration given to problematic medications, extra monitoring requirements to be care planned. Referral to the QUIT service where available.
5.4.3.2 Smoking cessation pathway
- 10 to 12 week cessation program care-planned as per guidance.
- Support by QUIT tobacco treatment advisor’s and, or ward staff until complete cessation cessation.
5.4.3.3 NRT maintenance pathway
- Assessment for regular and, or PRN NRT supplements.
- Support by QUIT tobacco treatment advisor’s and, or ward staff for the duration of the inpatient stay.
5.4.3.4 NRT provision on the ward (products to be securely stored in the treatment room, or nurses’ station)
- Daily NRT patch to be prescribed on drug card and administered.
- Assessment for self-administration:
- self administration not appropriate, use of ward stock on patient request and recorded on the form PRN nicotine replacement therapy NRT record of use
- self, administration appropriate, access to own labelled pack. Level of access determined by patient and ward circumstances. Use recorded on the form PRN nicotine replacement therapy NRT record of use
5.4.3.5 Patient discharged
Patients on problematic medication must be advised of consequences of re-starting smoking and where appropriate additional monitoring arranged and information provided.
Cessation attempt completed:
- no discharge NRT supplied
- patient advised of local smoking cessation service
Cessation attempt incomplete or patient wishing to attempt cessation on discharge:
- 2 weeks TTA NRT to be provided and patient continue to be supported by the QUIT service or referred to local smoking cessation service
Attempted NRT maintenance only (patient intends to re-start smoking once home):
- 2 weeks TTA NRT to be provided and patient advised of local smoking cessation service
5.4.4 Risk Management on inpatient wards
All patients who are identified as smokers should have a smoking risk assessment completed (see appendix A) and a risk management care plan put in place to manage any known risks. Risks that need to be considered include:
- covert smoking, particularly in bed
- banned items such as ignition sources and cigarettes being brought onto the ward by visitors, or following a period of leave
- increased risk of the patient absconding
- the risk that a patient who is using disposable e-cigarettes may ingest the lithium battery as a way of self-harming
Risk management of the chargeable vaping devices is covered in appendix F.
5.4.5 Medication management
Smoking increases the metabolism of different medications, including some antidepressants (tricyclics and mirtazapine), antipsychotics (clozapine, olanzapine and haloperidol), some benzodiazepines and opiates. This can result in significantly lower plasma levels and therefore, larger doses of the medication are required to achieve a similar therapeutic effect as in a non-smoker. Therefore when a person stops smoking the metabolism of some medication can be reduced resulting in higher, sometimes toxic plasma levels developing over a few days. This means that should a patient chose to stop smoking close monitoring will be required and doses of the medications will need to be adjusted within days if a patient choses to stop smoking and by up to 50% within a month of cessation.
For patients who are prescribed Clozapine it is recommended that plasma levels of clozapine should be measured before smoking cessation commences to enable more accurate and timely monitoring and adjustment of medications.
Full overview of the effects of smoking cessation on medicines metabolism and latest guidance on recommended adjustments is available from the specialist pharmacy service (opens in new window) or in RDaSH guidelines for nicotine management therapy and attached units, available on the intranet or though
the QUIT team by contacting rdash.quit@nhs.net.
5.4.6 Patients subject to assessment under section 136
A person who has been brought to one of the trust’s section 136 suites is there for an assessment of their mental health and not formally admitted to the inpatient services. it is recognised that if they are a regular smoker and unable to have a cigarette whilst awaiting assessment it can lead to an increase in their agitation and consequently negatively impact on their assessment.
In view of this staff should offer the patient the option of an approved disposable e-cigarette or the following 24 hour nicotine replacement therapy:
- 21mg per 24 hours if patient smokes more than 10 cigarettes per day.
- 14mg per 24 hours if patient smokes less than 10 cigarettes per day
The use of this is to be recorded on the form PRN Nicotine replacement therapy NRT record of use.
5.4.7 Seclusion
A secluded patient will not be able to smoke cigarettes, cigars, e-cigarettes or roll-ups and so on. for the duration of his or her seclusion and will have to be offered nicotine replacement therapy for the duration of his or her seclusion. Disposable and rechargeable e-cigarettes will be permitted subject to individual risk assessment.
5.4.8 Visitors
This policy applies to all visitors to trust premises. Staff will give advance information in their carer’s information packs to next of kin or visitors regarding the trust’s smoke free status and list of banned items. In cases where this is not possible, every effort will be made to inform the next of kin or visitor on arrival and or on first contact about this situation and request them to cooperate with the trust by not smoking whilst on trust premises. Any smoking paraphernalia they have in their possession is to be stored in one of the available lockers for the duration of their visit.
5.4.9 Environmental management
At the start of each shift a member of staff will be designated to undertake the routine observation of patients and these routine observations will include checking the general ward environment for evidence of none compliance with this policy. Where it has been identified by the ward team that any particular patient(s) is a high risk of non-compliance consideration needs to be given to the need to vary the frequency and times of these routine checks.
5.4.10 Access to information
All wards will have health promotion information on the harmful effects of smoking and smoking cessation support clearly displayed and available on their information or leaflet racks.
5.4.11 Non-compliance
In all cases where a patient persistently breaches the smoke free policy an MDT review should be held to agree what action needs to be taken to manage the situation. The agreed actions will then form part of the patients agreed plan of care, and where the patient has been identified as posing a fire risk due to covert smoking the trust supportive therapeutic observation policy should be implemented. All instances of non-compliance must be reported via Ulysses IR1 system (see section 5.6.1).
5.4.12 Violence and aggression
In cases where a patient is found smoking nicotine based products and refuses or becomes violent when requested to stop or hand over the cigarette or the smoking paraphernalia there is no expectation that the staff member should in anyway put themselves at risk. The action taken will be dependent on a number of factors which although not exhaustive includes:
- the level of perceived risk to the staff member or others if they try to force the issue with the patient
- where the patient is smoking
- the legal status of the patient
De-escalation is always the preferred option but if the situation requires immediate action staff are to follow the reducing restrictive interventions (RRI) policy (formerly PMVA policy).
5.4.13 Section 17 leave
As part of their recovery programme some patients have periods of leave from trust premises which are supported by staff. Whilst escorted leave forms an integral part of the patients recovery programme the smoking of tobacco products is not permitted whilst on escorted leave.
Guidance on managing section 17 leave for clinicians is available in appendix J.
5.4.14 Discharge
As part of discharge planning it should be ascertained if the if patient wishes to maintain their abstinence or quit attempt following discharge. If yes:
- include in discharge care plan
- issue 2 weeks TTA NRT products, this does not apply to the disposable e-cigarettes which are only available on the inpatient units
- notify relevant the RDaSH QUIT team and community staff
- automatically refer or signpost to local smoking cessation service (or continue with in-house support unless the patient ‘opts-out’ of receiving ongoing smoking cessation support)
- where a patient has stopped smoking, ensure that discharge notes make clear that blood plasma levels may be affected and may need to be adjusted
5.5 Breaches and reporting
5.5.1 Smoking-related incidents reporting on Ulysses IR1
All breaches of this policy are to be reported on the trust Ulysses IR1 incident reporting system in accordance with the RDaSH incident management policy. Such reporting will enable the trust to monitor any trends that are arising and take steps to proactively manage these and reduce the likelihood of future reoccurrence.
The following reporting categories should be selected when reporting a smoking-related incident:
| Reporting category | Selection that should be made when logging smoking-related incidents |
|---|---|
| Type of Incident | Security, loss, or damage |
| Cause group | Security, loss, theft, or damage |
| Cause | Smoking policy breach, or concern |
Note, all smoking-related incidents pose a fire hazard. However, where an incident is related to smoking or vaping, it should always be logged under the categories specified above. RDaSH fire safety team regularly monitors smoking-related incidents, alongside other fire incidents.
Similarly, where there is aggression and violence involved in a smoking-related incident, it should be logged under the categories above and not as a violence or aggression incident.
All ward staff with authorised access to Ulysses IR1 system are responsible for logging of the smoking-related incidents they have witnessed. Any problems with capacity and ability to report smoking-related incidents should be highlighted to the ward manager or service manager or modern matron.
Repeated non-adherence is to be reported to the relevant modern matron or service manager. Any complaint relating to this policy from or on behalf of patients should be dealt with by the ward or team manager or matron or service manager. If the issues remain unresolved the concern should be raised with PALS (patient advice and liaison service) or through the trust’s formal complaints procedure.
5.5.2 Sale of tobacco products
No sales of tobacco products will be allowed on trust premises including the provision of vending machines. It is a criminal offence for anyone to sell, transport or possess illegal tobacco products. Penalties for such offences may include imprisonment and, or fines including fines of up to £5000 for any manager allowing their premises to be used for such activities. The selling or storing and dealing in any way of illegal cigarettes and tobacco on trust premises will not be tolerated. Where staff have reasonable suspicion that there is cigarette and or associated paraphernalia in a clinical area, they will take steps including search to identify and remove it from the premises.
The trust will fully co-operate with law enforcement agencies, such as HM Revenue and Customs, in their investigations. Any such illegal activity by a member of staff will be considered as gross misconduct and will result in appropriate disciplinary action.
5.6 Staff support
5.6.1 Smoking cessation support for RDaSH staff
The trust recognises that staff who smoke may need support to comply with this policy, either to stop smoking completely, or staff who may wish to cut down prior to a quit attempt.
QUIT smoking cessation service is available for all individuals employed by RDaSH, including as bank or temporary staff. Colleagues can access up to 12 weeks of smoking cessation pharmacotherapy and behavioural support, up to twice per calendar year. To self-refer, contact rdash.quit@nhs.net.
A staff reward scheme, managed by the RDaSH Wellbeing team, is available for staff who successfully quit smoking. Staff who quit smoking can receive gift vouchers to the value of £20. To sign up:
- Email: rdash.quit@nhs.net
- Email: rdash.healthandwellbeing@nhs.net
5.6.2 Workplace responsibilities
Staff who smoke:
- must not smoke, chew tobacco or vape on hospital grounds, in trust premises or in trust vehicles
- must not smoke, chew tobacco or vape in front of patients, their families or carers
- will not take smoking breaks or vaping breaks during their contractual hours of employment
- can access in-house RDaSH support to quit smoking or community smoking cessation services
- can meet with their line manager to discuss and agree time off work in order to attend a smoking cessation clinic
- must not smoke whilst in uniform, irrespective of whether they are on duty, or on trust premises, when the uniform is identifiable as a Health Worker’s uniform, this principal equally applies to staff wearing an identity badge
- must not smoke in trust owned, leased or hired vehicles, smoking is not permitted in privately owned vehicles while traveling with other trust staff on trust business, smoking is not allowed on trust’s premises in a private vehicle
- must understand that trust disciplinary procedures for continued non-compliance with this policy may apply
5.6.3 Staff breaches
All trust staff are expected to promote a smoke-free environment and healthy living. Staff should avoid condoning, facilitating or advocating tobacco smoking. All trust staff are prohibited from purchasing or providing tobacco products for patients. Staff must not use tobacco as a reward for patients.
If any staff member breaches the policy then in the first instance line managers should discuss the issue with them and ensure they fully understand the smoke free policy. If staff continue to breach the policy then action through the RDaSH disciplinary policy and personal responsibility framework may be appropriate. All members of staff are obliged to support the implementation of the smoke free policy.
If a staff member is seen breaching the policy, this should be reported to their line manager and logged as a smoking-related incident on Ulysses IR1 system.
6 Training implications
Staff will be made aware of the contents of this policy through:
- line manager
- trust weekly bulletin
- team brief
- performance review
- trust intranet
- trust induction
- specialist training
All clinical areas should have suitably trained staff to support patients to stop smoking. It is recommended that all frontline staff in both community and inpatient services will complete the RDaSH very brief advice in smoking cessation training, and the trust’s conflict resolution and reducing restrictive interventions training courses.
Staff issuing pharmacotherapy products must be suitable trained to level 2 standard as a minimum. Staff can access the level 2 training independently though the National Centre for Smoking Cessation and Training (opens in new window) or though the RDaSH QUIT programme by contacting rdash.quit@nhs.net.
As a trust policy, all staff need to be aware of the key points that the policy covers. Staff can be made aware through a variety of means.
7 Monitoring arrangements
7.1 Policy implementation
- How: Incident monitoring via IR1’s as they arise.
- Who by: All managers.
- Reported to: Care Group Quality meetings.
- Frequency: As and when incidents of non-compliance are reported.
7.2 Smoking related fire incidents
- How: Exception report.
- Who by: Safety team.
- Reported to: Health, safety and security forum.
- Frequency: Bi monthly.
7.3 Smoking related (but non-fire) incidents
- How: Exception report.
- Who by: All managers.
- Reported to: Care Group Quality meetings.
- Frequency: Bi monthly.
8 Equality impact assessment screening
To download the equality impact assessment for this policy, please follow this link: Smoke free policy EIA.
8.1 Privacy, dignity and respect
The NHS Constitution states that all patients should feel that their privacy and dignity are respected while they are in hospital. High Quality Care for All (2008), Lord Darzi’s review of the NHS, identifies the need to organise care around the individual, ‘not just clinically but in terms of dignity and respect’.
As a consequence the trust is required to articulate its intent to deliver care with privacy and dignity that treats all service users with respect. Therefore, all procedural documents will be considered, if relevant, to reflect the requirement to treat everyone with privacy, dignity and respect, (when appropriate this should also include how same sex accommodation is provided).
8.1.1 How this will be met
There are no additional requirements in relation to privacy, dignity and respect
8.2 Mental Capacity Act
Central to any aspect of care delivered to adults and young people aged 16 years or over will be the consideration of the individuals capacity to participate in the decision making process. Consequently, no intervention should be carried out without either the individual’s informed consent, or the powers included in a legal framework, or by order of the court.
Therefore, the trust is required to make sure that all staff working with individuals who use our service are familiar with the provisions within the Mental Capacity Act (2005). For this reason all procedural documents will be considered, if relevant to reflect the provisions of the Mental Capacity Act (2005) to ensure that the rights of individual are protected and they are supported to make their own decisions where possible and that any decisions made on their behalf when they lack capacity are made in their best interests and least restrictive of their rights and freedoms.
8.2.1 How this will be met
All individuals involved in the implementation of this policy should do so in accordance with the guiding principles of the Mental Capacity Act (2005) (section 1).
9 Links to any other associated documents
- Physical health policy
- Supportive therapeutic observation policy
- Reducing restrictive interventions (RRI) policy (formerly PMVA policy)
- Searching of a person or their property policy
- Disciplinary policy
- Incident management policy
- Guidelines for nicotine management therapy and attached units (opens in new window) (staff access only)
10 References
- Department of Health and Social Care (2011) No Health Without Mental Health: a cross-government outcomes strategy (opens in new window).
- Department of Health and Social Care (2017) Smoke-free generation: tobacco control plan for England (opens in new window).
- Department of Health and Social Care (2017) Tobacco control plan: delivery plan 2017 to 2022 (opens in new window).
- Harker and Cheeseman (2016) The Stolen Years: Mental Health and Smoking Action Report, Action on Smoking and Health (ASH) (opens in new window).
- Health and Safety Executive (2020) Health and Safety at Work etc Act 1974 (opens in new window).
- Health and Safety Executive (2020) Health Act 2006 (opens in new window).
- NHS Digital (2018) Statistics on Smoking – England, 2018 (opens in new window).
- NICE (2021) Tobacco: preventing uptake, promoting quitting and treating dependence (opens in new window).
- Tobacco: preventing uptake, promoting quitting and treating dependence (opens in new window).
11 Appendices
11.1 Appendix A Smoking risk assessment for inpatient services
11.2 Appendix B Information sheet for community patients
11.2.1 Important information for people receiving home visits
Please consider the needs of our staff and provide them with a smoke free environment. Second hand smoke or passive smoking as it is sometimes called has been found by the government scientific committee on tobacco health to be harmful to people’s health. It can cause heart disease, stroke and lung cancer in adults. Being exposed to second hand smoke even for a short time can cause eye irritation, headache, cough, sore throat, dizziness and nausea.
Employers have a common law duty of care to take reasonable care to protect the health, safety and welfare of employees. The trust is required by the Health and Safety at Work Act 1974 to ensure employees and others are not put at risk.
We therefore ask you and, or you’re relative to provide a smoke free environment on the day when trust staff are due to visit you in your home.
11.2.2 How to protect staff from exposure to second hand smoke
- Avoid smoking inside your house for at least 1 hour before the healthcare worker is due to arrive.
- Open windows and doors to ventilate the room or area where the visit will take place.
- Try to keep one room smoke free at all times to be used for when the healthcare worker visits.
During the visit:
- do not smoke or let anyone else in the house smoke
- whilst the healthcare worker is in the house please ask anyone else in the house who smokes to go outside to smoke
11.2.3 Trust smoking policy
We ask staff to assess whether any environment they enter is safe for them to work in. If a smoke free environment cannot be provided staff will undertake a risk assessment and if necessary you will be offered alternative treatment options. The trust will support staff to leave any environment they consider to be unsafe.
11.2.4 Our undertaking to you
You will be advised of the day our staff will visit you. If the staff member is delayed you will be contacted as soon as possible.
11.3 Appendix C Reference flowchart for managing community and inpatient service users who smoke
11.3.1 Inpatient
- Inform patient of trust smoking policy.
- Assess support in stopping smoking.
- If yes, implement smoking intervention plan. End process.
- If no, advise on use of NRT to manage withdrawal symptoms and offer behavioural support.
- Early offer of support to be documented in intervention plan and next review date.
- Advise that tobacco products, lighters and matches are not to brought to wards. End process.
11.3.2 Community
- Inform patient of trust smoking policy.
- Assess support in stopping smoking.
- If yes, provide smoking cessation intervention if part of locally commissioned service or refer to local stop smoking service. End process.
- If no, advise to quit and encourage benefits of quitting and document in records.
- Advise that tobacco products, lighters and matches are not to brought to wards. End process.
11.4 Appendix D NICE guidance PH48 (2013) key point
11.4.1 Recommendations
This guideline includes recommendations on:
- identifying people who smoke and offering help to stop including intensive support in acute and mental health services, and maternity services
- providing information and advice for carers, family, other household members and hospital visitors
- advising on and providing stop smoking pharmacotherapies, and making these available in hospital
- adjusting drug dosages for people who have stopped smoking
- putting referral systems in place for people who smoke
- developing smoke free policies and commissioning smoke free secondary care services
- supporting staff to stop smoking and providing stop smoking training for frontline staff
11.4.2 Who is it for?
- Health and social care professionals, including clinical leads in secondary care services and managers of clinical services.
- Commissioners, leaders of the local health and care system and trust boards.
- Estate managers and other managers.
- People using secondary care services and their families and carers.
- Community services service users and staff.
Although PH48 guidance is primarily aimed at acute, maternity and mental health secondary services, it recommends ensuring continuity of care by integrating stop smoking support in secondary care with support provided by community-based and primary care services
11.5 Appendix E Smoking or tobacco use dependency calculator (Fagerstrom test)
How soon after you wake up do you smoke your first cigarette or use another tobacco product?
- after 60 minutes, 0
- 31 to 60 minutes, 1
- 6 to 30 minutes, 2
- within 5 minutes, 3
Do you find it difficult to refrain from smoking in places where it is forbidden?
- no, 0
- yes, 1
Which cigarette or smokeless tobacco product would you hate most to give up?
- The first in the morning, 1
- Any other, 0
How many cigarettes or smokeless tobacco products per day do you smoke or chew?
- 10 or less, 0
- 11 to 20, 1
- 21to 30, 2
- 31 or more, 3
Do you smoke more frequently during the first hours after awakening than during the rest of the day?
- no, 0
- yes, 1
Do you smoke or use a smokeless tobacco product even if you are so ill that you are in bed most of the day?
- no, 0
- yes, 1
11.5.1 Scores and dose recommendations
- Under 3, low dependence.
- 4 to 5, moderate dependence.
- 6 to 10, high dependence.
Depending on the level of addiction, a specific combination of NRT products and e-cigarettes will be recommended. All protocols are detailed in the RDaSH guidelines for nicotine management therapy and attached units, available on the intranet or though the QUIT team by contacting rdash.quit@nhs.net.
11.6 Appendix F Electronic cigarettes guidance
11.6.1 A6_1 National guidance
- 1.1, electronic cigarettes (e-cigs) are battery powered devices that deliver nicotine through inhaled vapour (hence the use of e-cigs often being referred to as vaping). E-cigarettes can be nicotine-containing or nicotine-free. E-cigarettes are currently the most popular stop smoking aid in England. There is an opportunity for e-cigarettes to help tackle the high smoking rates among people with mental health problems, particularly in the context of creating smoke free mental health units.
- 1.2, Health England (PHE) advise that encouraging smokers who cannot or do not want to stop smoking to switch to e-cigarettes could help reduce smoking related disease, death and health inequalities (vaping in England: 2021 evidence update summary).
- 1.3, The NHS Long Term Plan (2019) acknowledges the importance of smoking cessation in specialist mental health services for long-term users of specialist mental health, and in learning disability services. This will include the option to switch to e-cigarettes while in inpatient settings. Care Quality Commission (CQC, 2018) also support the use of e-cigarettes in mental health in-patient settings as an alternative to smoking.
11.6.2 A6_2 Health and safety of e-cigarettes
- 2.1, the evidence around e-cigarettes is still developing, including evidence on the long-term health impact. However, an evidence report commissioned by PHE (2015) advises that, whilst not completely risk-free, e-cigarettes are estimated to be at least 95% less harmful to health than smoking.
- 2.2, despite the relative safety of e-cigarettes and vaping when compared to smoking, health professionals are advised to be mindful about potential adverse reactions from the use of e-cigarettes. Use the Yellow Card scheme website (opens in new window) to report any suspected side effects or safety concerns with e-cigarettes and the e-liquids used for vaping accessed
- 2.3, it is currently understood that the risk to the health of bystanders from exposure to e-cigarette vapour is extremely low, although those with asthma and other respiratory conditions may be sensitive to it. PHE advises organisations to take this into account and to make adjustments where appropriate. Although there is no evidence of harm to bystander health in general, people may not wish to inhale it due to personal preference and comfort.
11.6.3 A6_3 Types of e-cigarettes
- 3.1, there is a large number of products available which are different both in appearance and function. The most common types of products are described below (Source: okvape.co.uk)
- 3.2, Cigalikes look similar to tobacco cigarettes. They tend to have small batteries and can be disposable or rechargeable, but aren’t refillable. When the user takes a puff (or presses a button on some models) the device heats a coil which vapourise the e-liquid and creates the vapour that can be inhaled.
- 3.3, pod vapes fall somewhere between a Cigalike and a vape pen kit. They come in a variety of shapes and sizes but are often a flat pen shape, fairly small and designed to fit neatly in the hand. Pod kits consist of a rechargeable battery and a replaceable ‘pod’. The pod incorporates the mouthpiece, coil and tank, pre-filled with e-liquid. Once a pod is empty, the pod is discarded and replaced with a new one. These pod refills are specific to the brand and model of pod device but most are available with a wide variety of flavours and nicotine strengths.
- 3.4, vape pens look less like normal cigarettes and are shaped like a pen or small tube. They are refillable with either pre-filled cartridges or have a tank that can be refilled with e-liquid of varying flavours and strengths. The batteries tend to last longer than Cigalike batteries. Vape pens consist of a long, cylindrical battery section, with an integrated tank. Similar to a pod vape, the tank contains a coil and e liquid tank with a mouthpiece. However, they differ in that the coils are replaceable, the mouthpiece is usually removable and the tank is designed to be filled with e liquid by the user. Some devices also include buttons to change the wattage or voltage output of the device. They also often include an airflow adjustment ring on the tank to increase the amount air flowing through the tank and create a tighter, or airier ‘draw’.
- 3.5, box kits or mods are essentially very similar to vape pen devices, however the battery or mod part of the device is rectangular or box shaped. They are sometimes referred to as personal vapouriser. These can be used with various atomisers, cartomisers and tank systems. These typically use larger batteries and have adjustable power settings, allowing the user to vary the voltage applied to the atomiser. These often come with software to allow users to programme voltage and or monitor their usage patterns.
11.6.4 A6_4 E-cigarettes permitted on RDaSH premises
11.6.4.1 A6_4 .1 Inpatients
- 4.1.1, all inpatient service users at RDaSH who have used any nicotine-containing products in the month prior to admission, are offered a range of nicotine replacement products on admission, including disposable e-cigarettes (E-Burn, Dinner Lady or another brand). Disposable e-cigarettes are available free of charge through the wards’ supply and are issued by the nursing staff, subject to individual risk assessment.
- 4.1.2, wherever possible, inpatients should be encouraged to use trust-supplied disposable e-cigarettes. However, some service users may prefer their personal vaping devices. These must be authentic devices purchased from the reputable retailers, supplied with original charging cables. Ward staff must inspect patients’ vaping devices on admission and can restrict the use of the devices or charges that are suspected to be counterfeit or where there is evidence of mixing of the illegal substances into the vaping liquid.
- 4.1.3, inpatient service users can vape outdoors on the trust grounds and in the court yards. In certain circumstances (for example, extreme weather), vaping can be allowed indoors in the communal areas at the discretion of the ward management. Vaping is not allowed in the kitchen or near fire alarms exhaled e-cigarette vapour may trigger some types of smoke detectors.
- 4.1.4, vapers who are in isolation for health reason, for example, COVID-19, are permitted to vape in their bedroom, subject to the standard risk assessment clearance. Vapers who are in seclusion aa behaviour management intervention may be at risk of self-harm and therefore must be risk-assessed more frequently and only permitted to use vaping devices in seclusion where the risk of harm or misuse is deemed negligible. Alternatively, they must be offered standard NRT products for the period of isolation.
11.6.4.2 A6_4 .2 Community patients, visitors and staff
- 4.2.1, the trust currently does not supply free e-cigarettes to the community patients. Community patients can use their personal vaping devices in the outdoor areas. Community patients should be referred, with their consent, to the QUIT service who can offer nicotine dependency treatment or make an onward referral. Contact rdash.quit@nhs.net if you would like to refer a community patient or have any questions.
- 4.2.2, RDaSH visitors can use personal vaping devices in the outdoor areas. Visitors much not charge their devices on RDaSH premises.
- 4.2.3, RDaSH staff can use personal vaping devices during non-work time in the outdoor areas. They must not be used within vehicles owned or leased by the trust. Any member of staff can self-refer to the trust’s QUIT team and receive free and confidential nicotine dependency treatment by contacting rdash.quit@nhs.net.
11.6.5 A6_5 E-cigarettes and fire safety
- 5.1, although fires cause by e-cigarettes are very rare compared to those caused by smoking materials, the root cause of such fires is likely to be due to a malfunctioning lithium battery (National Fire Chiefs Council (NFCC), 2018).
- 5.2, the risks associated with charging e-cigarettes should be considered alongside the risks of charging any other rechargeable personal electronic devices, such as mobile phones and laptops etc. National Fire Chiefs Council (2018) issued some key messages around the safe charging of e-cigarettes.
- 5.3, e-cigarettes should be kept away from any source of ignition and accelerants such as flammable objects and liquids, oxygen rich environments or oxygen supply systems or cylinders, sparks from electrical equipment etc.
- 5.4, based on the NFCC guidance, RDaSH staff on the inpatient units should follow the principles below:
- only use chargers designed for use with the specific device, some chargers may overcharge the product, leading to an increased risk of fire
- staff can refuse charging of the devices where they have grounds to believe that the vaping device or the charging cable are counterfeit, incompatible or tampered with, in counterfeit devices batteries and, or chargers are unlikely to have overcurrent protection and could lead to batteries exploding
- when the charge is complete, disconnect battery and remove charger from USB port or socket, this is usually indicated by a light on the device
- never leave an electronic cigarette charging unattended
- never leave them charging overnight
- store batteries and chargers in a cool dry place at normal room temperature, do not leave them in hot places such as direct sunlight
- do not immerse batteries or chargers in water or otherwise get them wet
- never use damaged equipment or batteries
- never carry batteries, keys or coins in the same pocket or bag
- never use a vaping device close to medical oxygen, flammable emollient creams or airflow mattresses
- never modify or adapt e-cigarettes and their associated kit
- contact the estates team if you require additional sockets installation to facilitate the charging
11.6.6 A6_6 Self-harm and ligature risks
- 6.1, service users are permitted to use any e-cigarette to support them in remaining smoke free on trust sites providing that an individual risk assessment is conducted by staff prior to use or recharging commencing. Staff must ensure that service users are competent and able to use their device and any accompanying accessories such as chargers and oils or e-liquids safely.
- 6.2, if it is deemed inappropriate for a service user to keep their e-cigarette and accessories with them due to safety concerns, they should be stored centrally by the ward and may be used under supervision if appropriate.
- 6.3, some types of e-cigarette require refilling periodically with e-liquid or e-juice. It is important to note that this e-liquid can be harmful if ingested. Therefore use of such liquids by service users should be risk assessed on an individual basis, particularly where service users are at risk of self-harm or substance misuse.
- 6.4, charging cable present a ligature risk. For this reason, patients will be informed on admission that charging cables will be stored by the ward staff. Staff are to facilitate opportunities for supervised charging of devices in designated areas (for example, staff room or charging lockers). If a staff room is empty for a prolonged period of time (for example, overnight), vaping devices should not be left there charging unattended. Patients must not charge vaping devices in their bedroom.
11.6.7 A6_7 Risk assessment and general management
- 7.1, on admission, staff are asked to risk assess the safety of the electronic cigarettes by using the following checklist:
- look out for the CE mark that indicates chargers comply with European Safety standards
- check that the plug is not damaged and that the cable is properly secured with no internal wires visible
- check the electrical cable is not damaged and has not been repaired with insulating tape or an unsuitable connector
- check that the outer cover of the equipment is not damaged in a way that could lead to hazards
- check for burn marks or staining that suggests the equipment is overheating
- if you have any concerns about the above, contact the QUIT team on rdash.quit@nhs.net who can help with the inspection of the device, offer NRT products and trust-supplied e-cigarettes to the patient in the meantime
- 7.2, faulty or damaged e-cigarettes and associated accessories should be disposed of appropriately. Any disposal of e-cigarettes and, or their batteries should be in line with guidance for the disposal of waste electronic and electrical equipment within the trust waste policy.
- 7.3, charging of the vaping devices must take place in the designated areas, for example, staff rooms or secure lockers, where available. Charging should not take place in the service users’ bedrooms to prevent the risk of ligature.
- 7.4, devices are only to be charged via mains adaptor and are not charged through trust property (for example, USB to trust computer). E-cigarettes are not to be left unattended whilst charging or left charging overnight. The device should be unplugged once charging is complete.
- 7.5, e-cigarettes and the associated batteries and chargers should be kept dry, should not be immersed in water, and should be stored in a cool dry place.
- 7.6, if staff find that a service user’s device does not comply with the above then it should not be permitted for use and should be stored by staff until the service users discharge or returned to a family member or carer.
- 7.7, any incidents involving e-cigarettes should be reported on the IR1 system under the following categories:
- type of incident, security, loss, or damage
- cause group, security, theft, loss, or damage
- cause, smoking policy breach, or concern
11.6.8 A6_8 Risks associated with lithium batteries
- 8.1, disposable vaping devices use lithium batteries that are a powerful source of energy and used in many products including mobile phones and key fobs. Swallowing is a potential danger and immediate medical attention is necessary if this happens. Appropriate risk assessment is therefore important. If there is a risk of a patient ingesting batteries from the electronic cigarettes, they should be issues with an alternative NRT product.
- 8.2, if a battery is damaged or a fault develops for any reason, it will be evident from the high emission of heat. In this situation the device should be placed on a dry hard surface (concrete floor or dinner plate will be ideal) and allowed to discharge. Device manufacturer should be contacted to report the malfunction.
11.7 Appendix G Location of the RDaSH smoking template for screening of the mental health community services patients
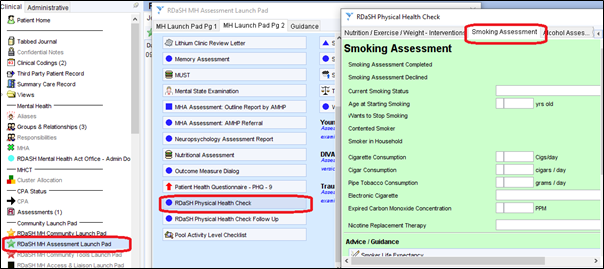
To find the location of the RDaSH smoking template for screening of the mental health community services patients, find RDaSH MH “Assessment Launch Pad” under the clinical section, then underneath “Community Launch Pad” category.
Then navigate to “RDaSH Physical Health Check”, and then “Smoking Assessment”.
11.8 Appendix H QUIT referral form on SystmOne
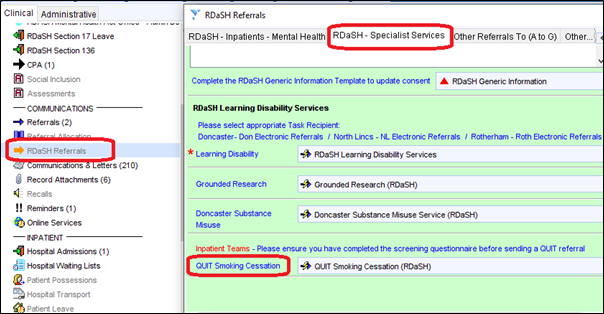
To find the location of the QUIT referral form on SystmOne, find “RDaSH Referrals” under the clinical section, then underneath the “Communications” category.
Then navigate to “RDaSH Specialist services” on the top navigation pane, then click “QUIT Smoking Cessation”.
11.9 Appendix I RDaSH Inpatient smoking screening questionnaire for inpatient services
Full training on using of the inpatient smoking screening questionnaire is available on RDaSH staff intranet (staff access only) (opens in new window).
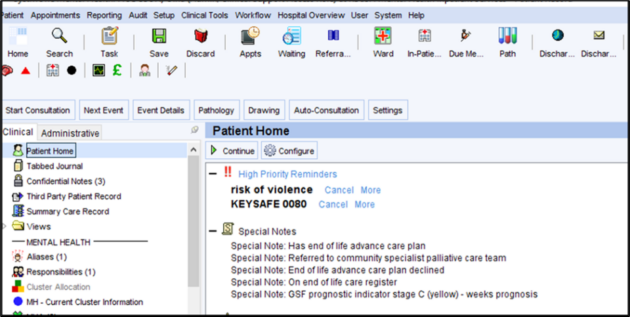
To find the smoking screening questionnaire click the icon of a smoking cigarette on the top navigation panel.
11.10 Appendix J Section 17 leave guidance for clinicians
11.10.1 Section 17 leave
For detained patients receiving care and treatment within inpatient mental health services, periods of leave from the ward play an important part in their treatment plan, particularly in relation to discharge planning. The decision to grant leave of absence from hospital has to balance the contribution that leave makes to the patient’s rehabilitation against considerations for the safety of both the patient and others.
Studies have shown that section 17 leave has been granted to specifically enable smoking by patients, including leave escorted by staff. However, section 17 was not designed to facilitate smoking breaks.
11.10.2 What’s the issue with granting section 17 escorted leave for smoking?
The trust position as outlined in the smoke free policy is that smoking of tobacco products is not permitted whilst on escorted leave.
Granting escorted section 17 leave to permit smoking:
- undermines trust policy
- provides an inconsistent message about our approach to health promotion and reducing the harm from tobacco addiction
- places staff at risk from second-hand smoke exposure
- reduces staff time for the completion of other essential duties, tasks and therapies
- perpetuates stigmatising views that mental health patients have little else to enjoy and are unlikely to succeed at reduction or cessation
- can cause more frustration for patients when leave cannot be facilitated and
- can increase symptoms of withdrawal due to intermittent smoking
11.10.3 What can I do differently?
- Discuss escorted leave plans in advance with agreement of the therapeutic goal.
- Ensure that the patient is aware that they will not be permitted to smoke in the company of the escort.
- Agree a plan for managing tobacco addiction during leave.
- Ensure the patient is referred to the in-house QUIT service and involve tobacco treatment advisors in multidisciplinary team discussions.
- Review breaches to leave care plans with the team.
- Continue with behaviour intervention.
Document control
- Version: 6.2.
- Unique reference number: 32.
- Ratified by: Clinical policies review and approval group.
- Date ratified: 29 January 2024.
- Name of originator or author: Deputy director of nursing and quality.
- Name of responsible individual: Executive director of nursing and allied health professionals.
- Date issued: 7 February 2024.
- Review date: October 2024.
- Target audience: All trust staff.
Page last reviewed: April 26, 2024
Next review due: April 26, 2025