Contents
- Introduction
- Scope
- Equality and diversity
- Human Rights Act
- Governance
- Powers to remove to, or keep at, a place of safety
- Places that can be used as a place of safety
- Arrival at places of safety
- Local section 136 suite procedures
- Record keeping
- Complaint’s procedure concerning section 136 assessment process, overcoming assessment barriers
- Information sharing
- Data collection
- Monitoring and audit
- References
- Appendices
1 Introduction
This policy governs the implementation of section 136 of the MHA 1983 and related legislation. It applies to all age groups.
The policy has been prepared to ensure that the use of section 136 can be subject to local agreement but are within an accepted framework, ensuring that agencies with a South Yorkshire wide remit are not subject to individual practices which may be diverse.
This policy refers to registered medical practitioners, which for RDaSH staff means a section 136 will be assessed by a consultant psychiatrist, specialty trainee in psychiatry or a doctor who is section 12(2) approved.
2 Scope
This policy and its procedures apply to all statutory agencies who fulfil a role in the undertakings and requirements of section 136 of the MHA 1983 and who operate within the boundaries of South Yorkshire and North Lincolnshire.
The aim of the policy is to ensure:
- all agencies that are party to this protocol are aware of their roles and responsibilities
- persons detained under section 136 MHA 1983 are treated with respect, without discrimination and are assessed as quickly as practicable
- persons with mental health issues detained for criminal offences, are processed with due regard to the law. A mental disorder whilst correctly taken into consideration is not an automatic bar to due criminal process
- all agencies focus on providing the best possible support for the detained person to enable a quick recovery and return to their place in the community
Interagency co-operation and communication are vital to the effective implementation of this policy.
3 Equality and diversity
This policy aims to ensure that all people detained under section 136 will be offered services that are safe and effective and led by the needs of the person. The standards within the policy will be applied equally to all patients, including those discharged from services and those who discharge themselves against medical advice.
4 Human Rights Act
The Human Rights Act 1998 requires public authorities and their employees to respect the convention rights, to understand those rights and to take them into account when carrying out this policy and the procedures within it. Particular reference is made to article 5, the right to liberty and security.
5 Governance
This policy is owned by the South Yorkshire and Bassetlaw ICS crisis pathways group and Humber Coast and Vale Right care right person group. It has responsibility for ensuring that the guidelines within this policy are followed, for reviewing emerging ‘lessons learnt’ and for monitoring performance.
Any changes to this policy may only be ratified by the South Yorkshire and Bassetlaw ICS crisis pathways group and Humber Coast and Vale right care right person group.
The policy is aligned to the principles within the crisis care concordats.
6 Powers to remove to, or keep at, a place of safety
6.1 Detention under section 136(1)
Under section 136(1) of the MHA 1983, a police officer has the power to remove a person who appears to be suffering from mental disorder and to be in immediate need of care or control:
- to a place of safety within the meaning of section 136
- if the person is already at a place of safety within the meaning of that section, keep the person at that place or remove the person to another place of safety
A person removed to or kept at a place of safety under this section may be detained there for a period not exceeding the permitted period of detention for the purpose of enabling him to be examined by a registered medical practitioner and to be interviewed by an approved mental health professional (AMHP) and of making any necessary arrangements for his treatment or care.
“Permitted period of detention” means:
- the period of 24 hours beginning with:
- in a case where the person is removed to a place of safety, the time when the person arrives at that place
- in a case where the person is kept at a place of safety, the time when the constable decides to keep the person at that place
6.2 Where section 136(1) power can be used
The power of a constable under section 136(1) may be exercised where the person is at any place, other than:
- any house, flat or room where that person, or any other person, is living
- any yard, garden, garage or outhouse that is used in connection with the house, flat or room, other than one that is also used in connection with one or more other houses, flats, or rooms
Section 136(1B) enables a police officer to enter any place in which section 136(1) applies, if necessary, by force, to remove a person.
Section 135 should be used if the person is in private premises (MHA Code of Practice 2015 16.18). Staff should refer to the trust’s section 135 policy for further information.
6.3 Consultation prior to use of section 136
Before deciding that detention under section 136 MHA 1983 may be necessary, unless the person is in immediate danger, the constable must, where practicable, contact and seek advice from a mental health clinician before using the powers to remove a person to, or to keep a person at, a place of safety. Mental health clinicians can be:
- a registered medical practitioner
- a registered nurse
- an approved mental health professional
- an occupational therapist
- a paramedic
The purpose of the consultation is for the police officer, who is considering using their powers under section 136, to obtain timely and relevant mental health information and advice that will support them to decide a course of action that is in the best interests of the person concerned. Advice is usually sought through the Mental Health Crisis team or single point of access.
The police officer retains ultimate responsibility for the decision to use their section 136 powers, having considered the advice given to them as part of any consultation. The police officer should ensure that any consultation is recorded, including who was consulted and the advice they gave.
The police officer should ensure that any decision not to consult before using section 136 powers, and the reason, is recorded.
Where a person is to be removed to, or kept at a place of safety, the police officer detaining the person must ensure that contact is made with the local section 136 suite staff prior to attendance so that all staff can prepare for the arrival.
6.4 Protective searches under section 136
Police officers are now legally able to search a person subject to section 136 if the Officer has reasonable grounds for believing that the person may present a danger to himself or herself or to others and is concealing on his or her person an item that could be used to cause physical injury to himself or herself or to others.
The power to search does not authorise an Officer to require a person to remove any of his or her clothing other than an outer coat, jacket or gloves, but does authorise a search of a person’s mouth.
An Officer searching a person in the exercise of the power to search may seize and retain anything found, if he or she has reasonable grounds for believing that the person searched might use it to cause physical injury to him or herself or to others.
7 Places that can be used as a place of safety
7.1 Places of safety
The act now defines a place of safety as:
- a hospital
- an independent hospital or care home for mentally disordered persons
- a police station
- residential accommodation provided by a local social services authority
- any other suitable place (with consent of a person managing or residing at that place)
7.2 Other suitable places
Any other suitable place will involve the evaluation of a number of factors including, the physical environment, the condition and behaviour of the person, and potentially any relationship between the person and the place. As a minimum a suitable space should be quiet, comfortable and have private space for the person to wait and potential physical risks should be identified and mitigated so far as is possible.
Where consideration is being given to using a private house, flat or room as a place of safety there will need to be authorisation from the occupier or at least one of the occupiers to agree to the place being used as a place of safety.
Where consideration is being given to using other premises other than a private house, flat or room then a person who appears to the police officer to be responsible for managing the place must agree to its use as a place of safety.
The request to use these types of premises as places of safety and the agreement should be recorded.
7.3 Use of a police station
Section 136A(1) states that a police station may not be used as a place of safety for a person under the age of 18, in any circumstances.
A police station may only be used as a place of safety for a person aged 18 and over in the specific circumstances set out in The Mental Health Act 1983 (Places of Safety) Regulations 2017:
- the behaviour of the person poses an imminent risk of serious injury or death to themselves or another person
- because of that risk, no other place of safety in the relevant police area can reasonably be expected to detain them
- so far as reasonably practicable, a healthcare professional will be present at the police station and available to them
An officer of at least the rank of inspector must give authority for the use of a police station in such circumstances.
The healthcare professional will be required to check the welfare of the detained person at least every half hour and any appropriate action be taken for their treatment and care. The details of these checks should be recorded.
The custody officer will be required to review, at least hourly, whether the circumstances continue to exist, for example, that their behaviour poses an imminent risk of serious injury or death to themselves or others, and that because of that risk no place of safety other than a police station in the relevant police area can reasonably be expected to detain them.
In circumstances where the person is sleeping a review may be extended to once every 3 hours provided that the healthcare professional carrying out the half hourly checks has not identified any risk that would require them to be woken more frequently. During this time the half hourly healthcare professional checks should still continue, to assess whether the person is genuinely sleeping, whether such a period of sleep may be beneficial, or whether apparent sleep may be masking other physical symptoms such as a fit or unconsciousness for which urgent medical attention will be required.
The custody officer will be required to arrange for a person to be taken to another place of safety in the following circumstances:
- the requirement that a welfare check be carried out every half hour or that a healthcare professional be present and available throughout the detention are not met
- the criteria for using the police station as a place of safety no longer exist
However, there is an exception to the above requirements, in that, if arrangements have already been made for a mental health assessment to take place at the police station and postponing the assessment would cause distress to the person then transfer need not take place. This may be in circumstances where the AMHP is already on route and the assessment is likely to commence and were transferring the person to another place of safety would be likely to take longer than for the AMHP to arrive at the police station.
7.4 Emergency department (ED) for medical assessment and treatment
The Emergency department legally falls within the definition of a place of safety, but it should only be used as a temporary place of safety if the patient requires medical treatment that could not be otherwise provided by the mental health place of safety or police custody. On arrival at ED detention under section 136 starts.
The police officer accompanying the patient should notify the ED reception that the patient is detained under section 136 of the MHA 1983 in order to secure a priority medical referral pathway and prompt onward transfer to a designated place of safety.
Police officers must complete the section 136 documentation (see appendix G) upon arrival at ED (detailing the time of detention) and relevant documentation will be provided by reception staff upon request.
ED staff should notify the Mental Health Crisis team, single point of access and AMHPs that there is a person detained on a section 136 at ED in order that the AMHPs are sighted on the start time of the 24 hour clock.
While awaiting medical assessment and treatment it will not be appropriate for the patient to be left unsupervised.
In the event that a medical assessment determines that admission is necessary a joint risk assessment and formal handover of responsibility will need to occur before the police officer can be discharged of the responsibility for the custody and care of an individual detained under section 136 of the MHA 1983. The NHS trust will release staff, where the joint risk assessment (see appendix B) permits, and they have agreed to take responsibility for the individual.
If the individual is admitted to a general hospital ward for observation or treatment, the mental health assessment will take place during the 24 hour period. The general hospital ward staff and the police officer will both contact the Mental Health Crisis team, single point of access to advise them that the person has been admitted to a ward and that they require an assessment under section 136. The AMHP will liaise with the ward staff as to when it is appropriate for that assessment to take place.
Suitable arrangements will need to be put in place to ensure that following the assessment, if appropriate, the patient is transferred to the local mental health unit.
7.5 Health based places of safety
The following are the designated health-based places of safety for assessment of people detained under section 136 MHA 1983:
7.5.1 Adults
7.5.1.1 Doncaster
Section 136 Suite
Skelbrooke ward
Tickhill Road Site
Balby
Doncaster
7.5.1.2 Rotherham
Section 136 Suite
Kingfisher Ward
Swallownest Court
Aughton Road
Sheffield
7.5.1.3 North Lincolnshire
Section 136 Suite
Mulberry House
Great Oaks
Ashby High Street
Scunthorpe
Refer to appendix E for contact details.
7.5.2 under 16
7.5.2.1 Doncaster
ED
Doncaster Royal Infirmary
Armthorpe Road
Doncaster
7.5.2.2 Rotherham
ED
Rotherham General Hospital
Moorgate Road
Rotherham
7.5.2.3 North Lincolnshire
ED
Scunthorpe General Hospital
Cliff Gardens
Scunthorpe
Refer to appendix H for contact details.
8. Arrival at places of safety
8.1 Duration of section 136
The maximum period that a person can be detained at a place of safety under section 136 is 24 hours with the possibility of this being extended by a further 12 hours in specific circumstances.
The detention period begins:
- where a person is removed to a place of safety under section 136 at the point when the person physically enters a place of safety
- where a person is kept at a place of safety under section 136 at the point the police officer takes the decision to keep them at that place
The clock will continue to run during any transfers of a person between one place of safety or another.
If a person subject to Section 136 is first taken to an emergency department of a hospital for treatment of an illness or injury (before being removed to another place of safety) the detention period begins at the point when the person arrived at the emergency department (as a hospital is a place of safety).
8.2 Extending the detention period
The registered medical practitioner who is responsible for the examination of a person detained under section 136 may, at any time before the expiry of the period of 24 hours authorise the detention of the person for a further period of 12 hours (beginning immediately at the end of the period of 24 hours) to a maximum of 36 hours, but only in very limited circumstances.
The authorisation may only be given if the registered medical practitioner considers that the extension is necessary because the condition of the person detained (physical or mental) is such that it would not be practicable to complete the assessment before the end of the period of 24 hours. This could, for example, be if the person is too mentally distressed, or is particularly intoxicated with alcohol or drugs and cannot co-operate with the assessment process.
There is no provision to extend the 24 hour period for reasons other than the patient’s condition for example, a delay in attendance of the AMHP or registered medical practitioner or the availability of a bed, is not a valid reason for extending detention.
If the person is detained at a police station, and the assessment would be carried out or completed at the police station, the registered medical practitioner may give an authorisation to extend the maximum detention period but this must be approved by a police officer of the rank of superintendent or above as it would be unusual for a person to continue to meet the criteria to be held at a police station for up to 36 hours.
8.3 Retaking a person who escapes (section 138)
Section 138 deals with the powers to retake a person subject to Section 136 who escapes from custody.
Escape during removal to a place of safety:
- where a person escapes in the course of being removed to a place of safety under section 136(1), they may not be retaken under this provision after a period of 24 hours has expired from the time of that escape
Escape from a place of safety:
- where a person escapes after arrival at a place of safety, they may not be retaken under this provision after the maximum time that they could have been detained. In most cases this will be a total period of 24 hours but if an extension to that period (maximum of 12 hours) has already been authorised by the registered medical practitioner that must be taken into account
8.4 Children and young people under the age of 18
When a child or young person is under 18 years of age and is detained under section 136, the child or young person should not be removed to or kept at or taken to a place of safety that is a police station.
Note: In the case of children under the age of 16 please refer to appendix H for the appropriate designated place of safety.
8.5 Violence, aggression, drink or drug
Intoxication alone will not prohibit use of the local section 136 suite as a place of safety but may necessitate the retention of the escorting police officers to assist with the care and supervision of the person following a joint risk assessment (see appendix B). Delays in the assessment process may occur as a result of intoxication.
Where people are so intoxicated by alcohol or drugs as to present a health risk to themselves, the police officers should follow the normal ‘drunk and incapable’ procedures and ensure they are taken to the local Emergency Department for medical assessment.
Police officers will not be required to remain at the place of safety unless to provide support where increased risk has been identified. Where an individual poses an unmanageable high risk to others, they should be transferred to police custody to enable safe management. In the event that police officers remain at the place of safety to provide support the need for them to remain shall be jointly reviewed on a regular basis.
Staff should not use alcohol screening devices to determine levels of intoxication as a reason for exclusion (Code of Practice 16.44).
There may be some circumstances in which violent behaviour is connected to conditions for which appropriate medical assessment and treatment is required. Where necessary, police officers should work with staff from the receiving service to explore other options such as the assistance of appropriately trained staff to maintain a safe environment for both the patient and staff (section 136 staff should refer to their own trust policy on managing violence and aggression).
In circumstances where a person is excluded from a health based place of safety and taken into police custody as a place of safety, an incident report should be completed including a record of the decision, who made the decision and why (Code of Practice 16.62).
8.6 Conveyance to a place of safety
The MHA 1983 Code of Practice 2015 states that patients should always be conveyed in the manner which is most likely to preserve their dignity and privacy consistent with managing any risk to their health and safety or to other people (see section 17.3 of the MHA 1983 Code of Practice).
Therefore, the Ambulance service will provide transport from the location that the person was detained, to the designated place of safety. It may be necessary for a police officer to travel in the ambulance to assist with the conveyance of an aggressive individual or for ambulance staff to travel within the police vehicle where conveyance by the police is necessary to safely manage risk of violence or absconsion (see section 16.32 of the Code of Practice).
Before conveyance under section 136 of the Mental Health Act can take place, a risk assessment will be undertaken by ambulance staff and the police officer to determine which vehicle (ambulance or police) is the most appropriate means of conveying the patient to the place of safety. Where an ambulance is the most appropriate means of conveyance the police officer is required to follow the ambulance and, or attend the place of safety to enable a formal handover and joint risk assessment to be undertaken.
Section 137 of the MHA 1983 provides that the patient is in lawful custody and protects Ambulance staff by giving them all the powers of a constable.
8.7 Transfer between places of safety
The decision to transfer to another place of safety should always be in the detained person’s best interests (see section 16.53 of the Code of Practice). The mode of transport should be considered within the assessment process and can be arranged by the police or AMHP or a person authorised by them (see section 16.54 of the Code of Practice).
A person may be moved from one place of safety to another before the assessment has begun, whilst it is in progress or after it has been completed and waiting for arrangements to be made (see section 16.55 of the Code of Practice).
The benefit of the move needs to be weighed against any delay the move may cause in the person’s assessment and any distress the journey may cause them.
Unless it is an emergency, a person should not be transferred without the agreement of an AMHP, doctor or another healthcare professional competent to assess whether the transfer would put the person’s health or safety (or that of other people) at risk.
If arrangements have already been made for an AMHP and a section 12 approved doctor to assess a person, they should not be transferred to another place of safety before discussion with those professionals have taken place.
A detained person should never be transferred unless it has been confirmed that the new place of safety is willing and able to accept them (see section 16.58 of the Code of Practice).
9 Local section 136 suite procedures
9.1 Arrival at place of safety
On arrival at the place of safety, the relevant documentation (appendix G) must be completed by the police officers (Humberside police via the paper copy or South Yorkshire police via their electronic mental health portal) accompanying the patient and the patient’s rights and information leaflet (appendix D) administered by the section 136 coordinator or senior mental health nurse.
The request for the section 136 assessment (see appendix E for contact details) will be made at the earliest opportunity and an AMHP and registered medical practitioner informed of the detention so that plans are put in place to enable the assessment to be carried out as soon as practicable.
Any delays will be appropriately logged by the section 136 suite staff on the relevant documentation (appendix G) and systems.
Staff at the section 136 suite are empowered by the MHA 1983 to stop and restrain, (using reasonable force) anyone who is attempting to leave if they have been detained under section 136.
9.2 Joint risk assessment
A joint risk assessment (appendix B) of the patient must be undertaken and documented by the police and section 136 suite staff. This is to ensure that all available information held in police, mental health and medical records is considered as part of that risk assessment in order to determine the risk level and what supervision if any is necessary for the detained person.
Within North Lincolnshire there is an expectation that police officers will be released within 1 hour of arriving at the section 136 suite.
This risk assessment will be jointly reviewed on a regular basis throughout the detention period and negotiation or agreement between the police officer and nursing staff will determine whether the police officer will be required to remain at the place of safety to provide support. Where police officers are required to stay in attendance the need for them to remain shall continue to be jointly reviewed at regular intervals.
Serious consideration must be given to the releasing of police officers to resume policing duties as soon as possible. If it is agreed that police officers are not required, there is an expectation that should there be an escalation of risk that police officers will return to the place of safety to provide support.
The risk assessment documentation should accompany the patient in order that periodic informed risk assessments can take place regarding the patient.
This documentation will be monitored on a monthly basis at scheduled local section 136 liaison meetings against the monthly detentions in order to highlight any operational concerns and difficulties.
9.3 Information and patient rights
Patients detained are entitled under section 132 MHA 1983 to be given information relating to their rights whilst detained under section 136 (see section 4.12 of the Code of Practice). Leaflets will be available in ED and at the section 136 suites (appendix D).
9.4 Assessment
The registered medical practitioner is required to attend the place of safety for the purpose of examining the person and the AMHP must interview the person as soon as is reasonably practicable to do so. However, there may be occasions where the registered medical practitioner is aware that it is necessary or appropriate to delay the assessment process (for example, alcohol or drug intoxication). This assessment should be undertaken as soon as possible from the start time of detention. Good practice recommends that face-to-face contact with the AMHP and the registered medical practitioner should start within 3 hours where clinically appropriate. Where a delay is unavoidable communication should be maintained to advise of the earliest available time for attendance, and the reasons for that delay recorded.
It is preferable for the examination by the registered medical practitioner and the interview by the AMHP to be co-ordinated so that they are performed at the same time. Where this is not possible, the registered medical practitioner may examine and the AMHP may interview the person separately.
If the registered medical practitioner sees the person first and concludes that they have a mental disorder but that admission to hospital is unnecessary, or the person agrees to informal admission, the person must still be interviewed by an AMHP (MHA Code of Practice 2015 16.51).
If the detained person is assessed by the registered medical practitioner as not suffering from a mental disorder as defined by the MHA 1983 then the section 136 power expires and they must be discharged by the registered medical practitioner, even if not seen by an AMHP (MHA Code of Practice 2015 16.50).
Where the outcome of the registered medical practitioner’s examination indicates that an assessment under part II of the MHA 1983 is required, the AMHP will have the responsibility for the co-ordination of such an assessment.
Where the outcome of the registered medical practitioner’s examination indicates that an assessment under the MHA 1983 is not required, the person must be interviewed by the AMHP with regard to the making of any necessary arrangements for his treatment or care. Such arrangements need not necessarily be associated with any specific mental health needs, but also include wider community care needs and provision.
It is desirable for either an AMHP or consultant psychiatrist experienced in working with learning disabled people to be available to advise or assess, where it appears that the detained person has a learning disability.
It is also appropriate in the case of a child or young person to consult with a child psychiatrist and in the case of an older adult for an old age psychiatrist to be available.
Where language is an issue appropriate translation services should be engaged.
Note, if a person is detained under section 136 and it becomes apparent that they are subject to a community treatment order (CTO) the registered medical practitioner, AMHP should follow the recall or revocation procedure within the trust community treatment order policy.
9.5 Permitted extension of time limit
The registered medical practitioner may authorise a further period of detention, not exceeding 12 hours. This can be authorised at any time and begins immediately at the end of the period of 24 hours. This can only occur if the registered medical practitioner considers it necessary:
- because of the condition of the person being detained and it would not be practicable for the assessment to be carried out before the end of the period of 24 hours
- if the assessment began within that period, for it to be completed before the end
The registered medical practitioner should record this decision on form 136B (appendix J).
If the person is detained in police custody the further period can only be used if an officer of the rank of superintendent or above approves it (MHA Section 136B).
9.6 Action following assessment
Where admission to hospital is appropriate the person will either consent to admission (informal) or the person will be detained under the formal provisions within the MHA 1983.
If the person is formally detained under the MHA 1983 in any other place than the section 136 suite, in the first instance contact should be made with the ambulance service to transport the patient to the hospital unit. However, where there is a potential risk to others refer to 8.4 of this policy.
9.7 Discharge from assessment or treatment
Where admission to hospital is inappropriate:
- nursing staff or police officers should assist the person to arrange appropriate transportation to the community, where appropriate, from the place of safety
- relevant referrals should be considered or identified, and any issues or concerns highlighted to relevant agencies (including alcohol and drugs referrals)
- a copy of the outcome plan should be given to the relevant people (see appendix F)
- if the person is known to services, their care coordinator should be notified and where appropriate the care plan reviewed
- formal notification of the detention under section 136 and the outcome will be forwarded to the patient’s GP by the local MHA office
10 Record keeping
A record of the circumstances surrounding the detention, time of detention and arrival at the place of safety must be documented immediately on arrival at the place of safety (see appendix G).
All subsequent contact with and arrival times of the relevant professionals or agencies involved throughout the detention period, must be documented including the outcome of the assessment and end of detention period.
Police officers must include sufficient detail on the documentation to outline their decision-making process and confirm the legality of the detention.
RDaSH doctors must record the assessment in the electronic patient record.
Non-RDaSH doctors should be given the option of recording their assessment and this being able to be scanned into the patient record, by the local MHA office.
11 Complaint’s procedure concerning section 136 assessment process, overcoming assessment barriers
For the initial point of contact where resolution is required to a dispute out of office hours, please refer to appendix I.
12 Information sharing
Information sharing for the protection of life and prevention of crime enables information sharing between all the relevant agencies.
Where a detained person is transferred between the police custody suite and the hospital, written information will accompany them. It will include sufficient detail to identify any risk to themselves or other individuals, details of medication and medical condition. This is to enable the receiving agency to risk assess the further care needs of the individual and ensure staff safety. The police will include the above details on form BQ009 PER (prisoner escort record) and any accompanying police custody healthcare provider medical notes.
13 Data collection
Performance information in relation to section 136 detentions and incidents at mental health establishments should be made available to the South Yorkshire and Bassetlaw ICS crisis pathways group to enable South Yorkshire wide monitoring of this policy and to the right care right person group to enable Humber Coast and Vale monitoring and to enable any lessons to be learnt to be reviewed and improvements made.
Data to be collected:
- use of section 136
- demographics of persons detained
- length of time awaiting assessment
- methods of conveyance
- requests by AMHPs for police assistance
- referrals to health and social care agencies
- measures relating to diversion and multi agency responses
- arrested persons identified with both mental health and the influence of alcohol or drug use, including the number of individuals
- disputes
- outcomes of detention and assessment
- occasions where the place of safety is not available and why
14 Monitoring and audit
The South Yorkshire and Bassetlaw ICS Crisis Pathways Group and the Humber Coast and Vale right care right person group will monitor and audit this policy and will look for ways to further improve partnership working in the field of mental health.
The group will meet on a monthly basis.
The group will promote and encourage positive joint working arrangements regarding the application of mental health legislation with partners.
Key responsibilities include the formulation and implementation of policies and protocols governing multiagency work involving mental health detentions and monitoring of legislative compliance with the MHA 1983 and associated provisions including the Code of Practice.
The group will investigate the difficulties which may arise from working within the legal framework of the MHA 1983 and share good practice issues. It will also provide a forum for the discussion of incidents highlighting concerns.
15 References
This policy is in accordance with and has been formulated with due consideration to the guidance and recommendations contained within:
- The Mental Health Act 1983 (MHA 1983)
- The Mental Health Act 2007 (MHA 2007)
- The Mental Health Act 1983 Code of Practice 2015
- The Mental Capacity Act 2005 (MCA)
- The Police and Criminal Evidence Act 1984 (PACE)
- The Safer Detention and Handling of Persons in Police Custody 2006 (safer detention)
- The Independent Police Complaints Commission (IPCC) report, Police Custody as a ‘Place of Safety’ (2008)
- Royal College of Psychiatrists report, Standards on the use of Section 136 of the Mental Health Act 1983 (CR149 2008)
- The Bradley Report, Lord Bradley’s review of people with mental health problems or learning disabilities in the criminal justice system (2009)
- NPIA (National Police Improvement Agency) guidance on “Responding to People with Mental Ill Health or Learning Disabilities” 2010
- NPIA (National Police Improvement Agency) Protocol for the provision, management and conveyance to places of safety (Section 136 MHA 1983)
- Mental Health Crisis Care Concordat 18 February 2014
- The Mental Health Act 1983 (Places of Safety) Regulations 2017
- Department of Health: Guidance for the implementation of changes to police powers and places of safety provisions in the mental health act 1983 to October 2017
16 Appendices
16.1 Appendix A Agency protocols
16.1.1 Section 136, statement of responsibilities
16.1.1.1 Local authorities
Local social services authorities are responsible for ensuring that sufficient AMHPs are available to carry out their roles under the MHA 1983, including assessing patients to decide whether an application for detention should be made. To fulfil their statutory duty, local social services authorities must have arrangements in place in their area to provide a 24 hour service that can respond to patients’ needs (section 14.35 of the MHA 1983 Code of Practice 2015).
The local social services authorities are committed to providing AMHPs involved in implementing the local response to joint working for section 136 in accordance with the MHA 1983 Code of Practice 2015.
16.1.1.2 South Yorkshire police
South Yorkshire Police will ensure they undertake their responsibilities efficiently and effectively with their primary focus being the care and treatment of the detained person. Custody will only be used as a last resort and not simply as line of least resistance.
Hospital liaison and dealing with disputes will be the responsibility of the duty inspector on a 24 hour basis. Police should have an appointed mental health liaison officer who is available for assistance in respect of mental health related matters during normal working hours.
16.1.1.3 Health trusts
The local clinical commissioning groups, along with the trusts providing mental health services, will ensure sufficient designated places of safety.
Every effort must be made to give the correct support to people detained under section 136, including those under the influence of drugs or alcohol, or displaying aggressive behaviour, thereby helping the police to avoid criminalising people by having to take them into police custody.
Every effort must be made to ensure police officers are not unnecessarily delayed in places of safety.
The registered medical practitioner will attend the relevant place of safety, as soon as practicable, when contacted to provide an assessment under section 136 MHA 1983.
16.1.1.4 Commitment
That all possible steps are taken to ensure that the patient receives appropriate medical and nursing care to alleviate his or her mental disorder and reduce the risk to self and/or others. Where appropriate, aftercare will be provided upon discharge to achieve these aims.
16.2 Appendix B Joint risk assessment
16.3 Appendix C Local information sharing protocol
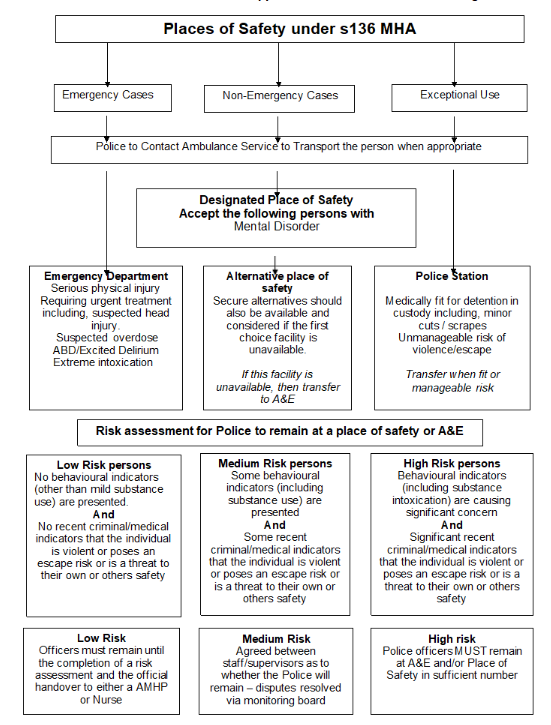
16.3.1 Places of safety under s136 MHA
16.3.1.1 Emergency cases
- Police to contact ambulance service to transport the person when appropriate.
- Emergency department, serious physical injury requiring urgent treatment including, suspected head injury. Suspected overdose ABD or excited delirium extreme intoxication.
16.3.1.2 Non-emergency cases
- Police to contact ambulance service to transport the person when appropriate.
- Designated place of safety accept the following persons with mental disorder.
- Alternatively place of safety, secure alternatives should also be available and considered if the first choice facility is unavailable. If this facility is unavailable, then transfer to A and E.
16.3.1.3 Exceptional use
- Police to contact ambulance service to transport the person when appropriate.
- Police station, medically fit for detention in custody including, minor cuts or scrapes. Unmanageable risk of violence or escape transfer when fit or manageable risk.
16.3.2 Risk assessment for police to remain at a place of safety or A and E
16.3.2.1 Low risk persons
No behavioural indicators (other than mild substance use) are presented and no recent criminal or medical indicators that the individual is violent or poses an escape risk or is a threat to their own or others safety. Officers must remain until the completion of a risk assessment and the official handover to either a AMHP or nurse.
16.3.2.2 Medium risk persons
Some behavioural indicators (including substance use) are presented and some recent criminal or medical indicators that the individual is violent or poses an escape risk or is a threat to their own or others safety. Agreed between staff or supervisors as to whether the police will remain, disputes resolved via monitoring board.
16.3.2.3 High risk persons
Behavioural indicators (including substance intoxication) are causing significant concern and significant recent criminal or medical indicators that the individual is violent or poses an escape risk or is a threat to their own or others safety. Police officers must remain at A and E and place of safety in sufficient number.
16.4 Appendix D Statutory rights leaflet
16.5 Appendix E Useful telephone numbers
16.5.1 Doncaster
- Place of safety: Skelbrooke ward 03000 211174 or 03000 211175
- Doncaster Royal Infirmary Hospital: Switchboard and A and E 01302 366666
- Crisis team: 03000 211288 or 0800 804 8999
- Force incident manager or duty inspector: 101
- Tickhill Road Hospital switchboard: 03000 213000
- Emergency Duty team or out of hours AMHP service via the single point of access (SPA): 03000 211288 or 0800 804 8999
- Police contact number: 101
16.5.2 Rotherham
- Place of safety: Kingfisher ward 03000 215521
- Rotherham General Hospital: Switchboard and A and E 01709 820000
- Crisis team: 0800 804 8999
- Force incident manager or duty inspector: 101
- Tickhill Road Hospital switchboard: 03000 213000
- Emergency Duty team or out of hours AMHP service: 0800 652 9571
- Police contact number: 101
16.5.3 North Lincolnshire
- Place of safety: 03000 216009
- Scunthorpe General Hospital: Switchboard and A and E 01724 282282
- Crisis team: 0800 015 0211
- Force incident manager or duty inspector: 101
- Great Oaks switchboard: 03000 216000
- Emergency Duty team or out of hours AMHP service: via North Lincolnshire Council 01724 297000. Adult Social Care team to speak with an AMHP (approved mental health professional) option 4 (people issues) then option 4 (adult social care), then option 2 (first contact or Safety), hold to be transferred to Out of Hours team.
- Police contact number: 101
16.6 Appendix F Section 136 outcome plan
16.7 Appendix G Section 136 monitoring form
16.8 Appendix H Places of safety, under 16 years of age
The following have been agreed as the principal places of safety within the NHS Trusts (see appendix E for contact details):
16.8.1 Doncaster
The place of safety for a person aged 16 and over is the section 136 suite attached to the psychiatric intensive care unit (Skelbrooke ward) at Tickhill Road Site.
The place of safety for a person under 16 years of age is the emergency department at Doncaster Royal Infirmary which allows subsequent referral to paediatric services which is the designated place of safety in such circumstances.
16.8.2 Rotherham
The place of safety for a person aged 16 and over is the section 136 suite attached to the psychiatric intensive care unit (Kingfisher ward) at Swallownest Court.
The place of safety for a person under 16 years of age is the emergency department at Rotherham General Hospital which allows subsequent referral to paediatric services which is the designated place of safety in such circumstances.
16.8.3 Scunthorpe
The place of safety for a person aged 16 and over is the section 136 suite attached to Mulberry House at Great Oaks.
The place of safety for a person under 16 years of age is the emergency department at Scunthorpe General Hospital which allows subsequent referral to paediatric services which is the designated place of safety in such circumstances.
16.9 Appendix I Section 140 provision for children and young people under the age of 18
RDaSH is not commissioned to provide inpatient services for children and young people under the age of 18.
The commissioned inpatient services for children and young people in Doncaster, Rotherham and South Humber are as follows:
- South Yorkshire ICB, The Becton Centre, Sheffield
- North Yorkshire and Humber ICB, Inspire, Hull
Therefore, all under 18 admissions for the purpose of section 140 should be referred to these services.
16.10 Appendix J Out of hours contact for initial dispute resolution
RDASH:
- on call manager (RDASH) via the Tickhill Road Hospital switchboard on 03000 213000.
SYP:
- district duty inspector or force incident manager on 101.
16.11 Appendix K Record of extension of detention under section 136
16.12 Appendix l Process to be followed in the event of a request to close the RDaSH section 136 suite
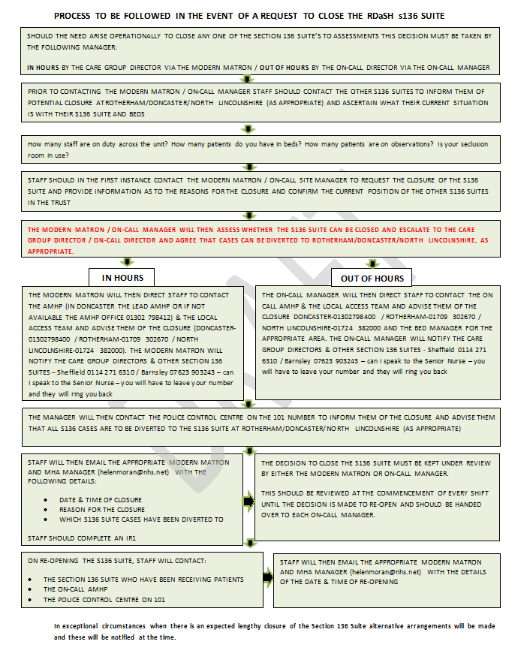
- Should the need arise operationally to close any one of the section 136 suite’s to assessment this decision must be taken by the following manager:
- in hours by the care group director via the modern matron
- out of hours by the on call director via the on call manager
- Prior to contacting the modern matron, on call manager staff should contact the other section 136 suites to inform them of potential closure at Rotherham, Doncaster or North Lincolnshire (as appropriate) and ascertain what their current situation is with their section 136 suite and beds.
- How many staff are on duty across the unit? How many patients do you have in beds? How many patients are on observations? Is your seclusion room in use?
- Staff should in the first instance contact the modern matron or on call site manager to request the closure of the section 136 suite and provide information as to the reasons for the closure and confirm the current position of the other section 136 suites in the trust.
- The modern matron or on call manager will then assess whether the section 136 suite can be closed and escalate to the care group director or on call director and agree that cases can be diverted to Rotherham, Doncaster or North Lincolnshire as appropriate.
- if in hours:
- The modern matron will then direct staff to contact the AMHP (in Doncaster, the lead AMHP or if not available the AMHP office on 01302 798412) and the local Access team and advise them of the closure (Doncaster: 01302798400, Rotherham: 01709302670 or North Lincolnshire: 01724382000). The modern matron will notify the care group directors and other section 136 suites, Sheffield: 0114 271 631 and Barnsley: 07623 90323, can I speak to the senior nurse, you will have to leave your number and they will ring you back
- if out of hours:
- the on call manager will then direct staff to contact the on call AMHP and the local Access team and advise them of the closure, Doncaster: 01302798400, Rotherham: 01709302670 or North Lincolnshire: 01724382000 and the bed manager for the appropriate area. The on call manager will notify the care group directors and other section 136 suites, Sheffield: 0114 271 631 and Barnsley: 07623 90323, can I speak to the senior nurse, you will have to leave your number and they will ring you back
- if in hours:
- The manager will then contact the police control centre on the 101 number to inform them of the closure and advise them that all section 136 cases are to be diverted to the section 136 suite at Rotherham, Doncaster, North Lincolnshire (as appropriate).
- Staff will then email the appropriate modern matron and MHA manager (helenmoran@nhs.net) with the following details:
- date and time of closure
- reason for the closure
- which section 136 suite cases have been diverted to
- staff should complete an IR1
- The decision to close the section 136 suite must be kept under review by either the modern matron or on call manager. This should be reviewed at the commencement of every shift until the decision is made to reopen and should be handed over to each on call manager.
- On reopening the section 136 suite, staff will contact:
- the section 136 suite who have been receiving patients
- the on call AMHP
- the police control centre on 101
Staff will then email the appropriate modern matron and MHA manager (helenmoran@nhs.net with the details of the date and time of reopening.
16.13 Appendix M Assessment and escalation process
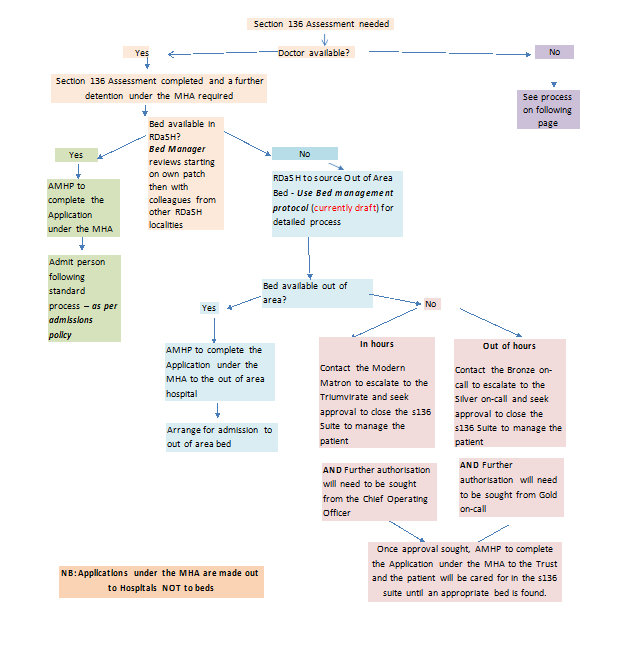
- Section 136 assessment needed
- Doctor available?
- if no, see process when doctor is unavailable
- if yes, section 136 assessment completed and further detention under the MHA required
- bed available in RDaSH? Bed manager reviews starting on own patch then with colleagues from other RDaSH localities
- if yes, AMHP to complete the application under the MHA and then admit person following standard process, as per admissions policy
- if no, RDaSH to source out of area bed, use bed management protocol for detailed process, is bed available out of area?
- if yes, AMHP to complete the application under the MHA to the out of area hospital and arrange for admission to out of area bed
- if no,
- in hours, contact the modern matron to escalate to the triumvirate and seek approval to close the section 136 suite to manage the patient and further authorisation will need to be sought from the chief operating officer.
- if out of hours, contact the bronze on call to escalate to the silver on call and seek approval to close the section 136 suite to manage the patient and further authorisation will need to be sought from gold on call
- once approval sought, AMHP to complete the application under the MHA to the trust and the patient will be cared for in the section 136 suite until an appropriate bed is found
Note, applications under the MHA are made out to hospitals not to beds.
16.13.1 Process when doctor not available for section 136 assessment
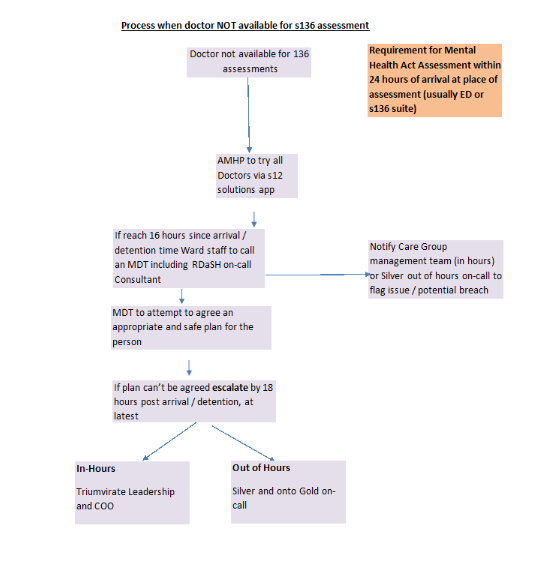
- Doctor not available for section 136 assessment.
- AMHP to try all doctors via s12 solutions app.
- if it reaches 16 hours since arrival or detention time ward staff to call an MDT including RDaSH on call consultant (notify care group management team (in hours) or silver out of hours on call to flag issue or potential breach).
- MDT to attempt to agree an appropriate and safe plan for the person.
- if plan can’t be agreed, escalate by 18 hours post arrival or detention, at latest:
- in hours, triumvirate leadership and COO
- out of hours, silver and onto gold on call
Document control
- Version: 9.3.
- Unique reference number: 94.
- Ratified by: Mental health legislation operational group.
- Date ratified: 23 October 2023.
- Name of originator or author: Mental health act manager.
- Name of responsible individual: South Yorkshire and Bassetlaw ICS crisis pathways group (section 136 task and finish Group) and Humber Coast and Vale right care right person group.
- Date issued: 15 January 2024.
- Review date: November 2024.
- Target audience: All statutory agencies who fulfil a role in the undertakings and requirements of section 136 of the MHA 1983 and who operate within the boundaries of South Yorkshire.
- Description of changes: Amendment, reference in appendix H “preferred place of safety to be removed and replaced with “place of safety” so it is very clear. Additional appendix added, section 140 provision for children and young people under the age of 18, therefore all appendix and page numbers have changed.
Page last reviewed: April 24, 2024
Next review due: April 24, 2025