Contents
1 Aim
In 2021, the Royal College of Paediatrics and Child Health (RCPCH) reviewed their guidance on perplexing presentations (PP) or fabricated or induced illness (FII) in children. The new guidance provides procedures for safeguarding children who present with PP and FII and offers practical advice on when and how to recognise it, how to assess risk and how to manage these types of presentations in order to obtain better outcomes for children.
The aim of this procedure is to assist staff in fulfilling their statutory duties to safeguard and protect children and young people where there is a concern about PP or FII in children.
For the purpose of this procedure the legal definition of ‘child’, applies to those under 18 years of age. The term ‘children’ applies to children and young people throughout this procedure and is anyone who has not yet reached their 18th birthday. If concerns around PP or FII are raised regarding an adult at risk then multi agency adult safeguarding procedures must be followed.
This procedure provides a framework for earlier intervention to explore the concerns of children, families, and professionals to address the issue of a PP before significant harm has come to the child or young person whilst also outlining when immediate action may be required.
This procedure is supplementary to national and local guidance and should be followed in conjunction with PP and FII in children guidance (RCPCH, 2021).
1.1 Perplexing presentation
Children and young people with perplexing presentations often have a degree of underlying illness, and exaggeration of symptoms is difficult to prove and can be hard for health professionals to manage and treat appropriately. In the absence of clear evidence about risk of immediate serious harm to the child’s health or life, the early recognition of possible FII (not amounting to likely or actual significant harm) is termed Perplexing Presentations. PP requires an active approach by medical professionals and an early collaborative approach with children and families. This differs from the previous advice not to inform families about FII suspicions while investigating. Though in some cases it may still be judged not safe to share concerns with the family at an early stage because of concerns that it may lead to increased risk for the child.
1.2 Fabricated or induced illness
Fabricated or induced illness in children is a situation whereby a child is, or is very likely to be, harmed due to parental behaviour and action, carried out in order to convince doctors that the child’s state of physical and mental health or neurodevelopment is impaired or more impaired than is actually the case. This can involve actions to falsify investigations, or induction of actual illness in a child and can include inadvertent harm caused by medical professionals such as unnecessary invasive investigations and procedures. FII involving deliberate deception of clinical services by the carer in the child is rare but is a serious safeguarding concern and requires immediate attention and action.
2 Scope
This procedure applies to those members of staff that are directly employed by Rotherham Doncaster and South Humber NHS Foundation Trust (RDaSH) and for whom RDaSH has legal responsibility. This procedure is also applicable whilst undertaking duties on behalf of RDaSH or working on RDaSH premises and forms part of their arrangements with NHS commissioners within Doncaster, Rotherham, and North Lincolnshire.
As part of good employment practice, agency workers are also required to abide by RDaSH policies and procedures, as appropriate, to ensure their health, safety, and welfare of those they care for, whilst undertaking work for RDaSH.
3 Link to overarching policy
4 Procedure
Perplexing presentations can be where:
- a child is being presented by a caregiver with symptoms and in some cases signs, that are inexplicable after all appropriate clinical examination and investigations have been carried out and no clinical cause having been found
- the symptom and symptoms complained of only occur in the presence of the caregiver. Despite arrangements for recording for example, seizures, there is usually no objective evidence for the clinician to assess
- the caregiver may also ask for and demand multiple health care referrals
- the symptoms reported are not borne out by the activities of the child as evidenced by others who are not the caregiver
- once a diagnosis has been proven not to be relevant, the caregiver persists in presenting it as an ongoing diagnosis when consulting with new professionals
- there is an exaggeration of symptoms and difficulties
- there may be a history of:
- change of address
- change of doctor and hospitals
- many out of hours attendances
4.1 Actions when FII is identified
Where a practitioner suspects or observes that a child is at immediate risk of or has suffered significant harm particularly by illness induction for example, observed that medication tampered with given or without need, then the Police should be informed using the ‘999’ service and a referral made to children’s social care as per local policy.
The RDaSH children’s safeguarding team should be informed via email: rdash.doncastersafeguardingchildren@nhs.net and a IR1 completed as per RDASH safeguarding procedures.
This is most likely to occur when there is evidence of frank deception, interfering with specimens, unexplained results of investigations suggesting contamination or poisoning or actual illness induction, or concerns that an open discussion with the parent might lead them to harm the child. The safety of siblings also needs to be considered.
All practitioners should be mindful of situations where informing the parents of the referral would place a child at increased risk of harm. In this situation, carers would not be informed of the referral before a multiagency discussion has taken place. This would usually be in the form of a formal strategy discussion.
4.2 Actions when PP is identified
The RDaSH practitioner has made steps to engage with parent, carer or child to determine and provide any early help intervention or support required but PP concerns remain around the health state and functioning of the child or children.
Where a practitioner has reason to suspect PP and further information or exploration is required, then they should first seek support and further advice from the RDaSH Safeguarding team via email: rdash.doncastersafeguardingchildren@nhs.net. The RDaSH Safeguarding team will discuss the concerns with the practitioner and advise of the appropriate actions for the PP pathway.
If the PP pathway is to be initiated the practitioner will inform their manager.
4.3 If PP is identified by CAMHS
The PP pathway will be led by a CAMHS consultant, and they will be the responsible consultant (RC) at this stage.
The responsibility should not be delegated to a more junior member of staff although they may be involved in the process of assessment and subsequent management under the RC supervision.
The RDASH children’s Safeguarding team should be informed via email: rdash.doncastersafeguardingchildren@nhs.net. The RDaSH Safeguarding team will discuss the concerns with the practitioner and advise of the appropriate actions for the PP pathway.
The Safeguarding team will have oversight of all PP and FII cases and will provide support and guidance throughout the process.
The RC must consider whether the parents or carers should be informed of any concerns regarding PP. Unless there is a risk of immediate, serious harm to the child’s health or life, parents or carers should be informed.
With support from the Safeguarding team, the RC must determine all relevant medical services involved with the care of the child (and siblings if appropriate) for example, general practitioners (GP), other consultants, and private doctors.
With support from the Safeguarding team, the RC must request relevant health information by sending a letter with an initial health information template to all involved health professionals, requesting a return within 10 working days of receiving the request (or sooner if necessary) (see appendix B and C).
The RDaSH initial health information template will be completed by the CAMHS Practitioner who identified the PP concerns with support from the RDaSH Safeguarding team.
RDaSH safeguarding team will collate all the returned templates.
The RC must arrange a multi professionals meeting within 28 days (or earlier if the specific case demands an immediate assessment) of initial identification of concerns. All health professionals involved in the child’s care and the designated professionals from the integrated care board for safeguarding children should be invited.
The RC will lead the meeting. Clear terms of reference and records of the meeting must be made at the time and the arrangement for these will be made by the RC.
There may need to be one or more professionals’ meetings to gather information, reach a consensus and develop a rehabilitation plan. Where possible, families should be informed about these meetings and the outcome of discussions if doing so would not place the child at additional risk. Notes from meetings may be made available to parents, on a case-by-case basis and are likely to be released to them should there be a subject access request under the Data Protection Act 2018 for the health records.
The outcome of the meetings will reach a consensus about the child’s state of health. If the meeting concludes that there is reasonable cause to suspect that a child is suffering or likely to suffer significant harm, the RC must ensure that a referral is made to the local authority’s children’s services. Discussions with a senior colleague in children’s services may also be helpful in deciding whether, and when a referral should be made. The police public protection unit must be informed of any referral where FII is suspected as this may also involve the committing of a crime.
If the meeting concludes that there is no reasonable cause to suspect that a child is suffering or likely to suffer significant harm, but the family require ongoing support, this should be considered within the professionals meeting and an ongoing health and education rehabilitation plan formulated.
All discussions and actions from the PP pathway should be recorded in the child’s health record on the safeguarding template so that other clinicians will have access to the information. Parent or carer’s access to the record will need to be restricted, and an alert should be added to reflect this. The terminology should focus on the category of abuse or medical neglect rather than PP and FII.
4.4 If PP is by any other RDaSH service
The PP pathway will be led by the child’s paediatrician or if not under the care of a paediatrician, a request will be made to the GP for a referral to a paediatrician with an overview of the concerns identified (see appendix D).
The RDaSH children’s safeguarding team should be informed via email: rdash.doncastersafeguardingchildren@nhs.net.
The safeguarding team will have oversight of all PP and FII cases and will provide support and guidance throughout the process.
The RDaSH initial health information template will be completed by the practitioner who identified the PP concerns with support from the RDaSH Safeguarding team.
The RDaSH initial health information should be returned to the child’s paediatrician who will be the RC.
The RDaSH safeguarding team will support the medical professional at attendance at the multi professionals meeting where the state of the child’s health will be discussed, and a consensus reached around actions for the family.
All discussions and actions during the PP pathway should be recorded in the child’s health record on the safeguarding template so that other clinicians will have access to the information. Parent or carer’s access to the record will need to be restricted, and an alert should be added to reflect this. The terminology should focus on the category of abuse or medical neglect rather than PP and FII.
A flowchart of the process can be found in appendix A.
5 Appendices
5.1 Appendix A Flowchart
5.1.1 PP concerns identified within CAMHS service
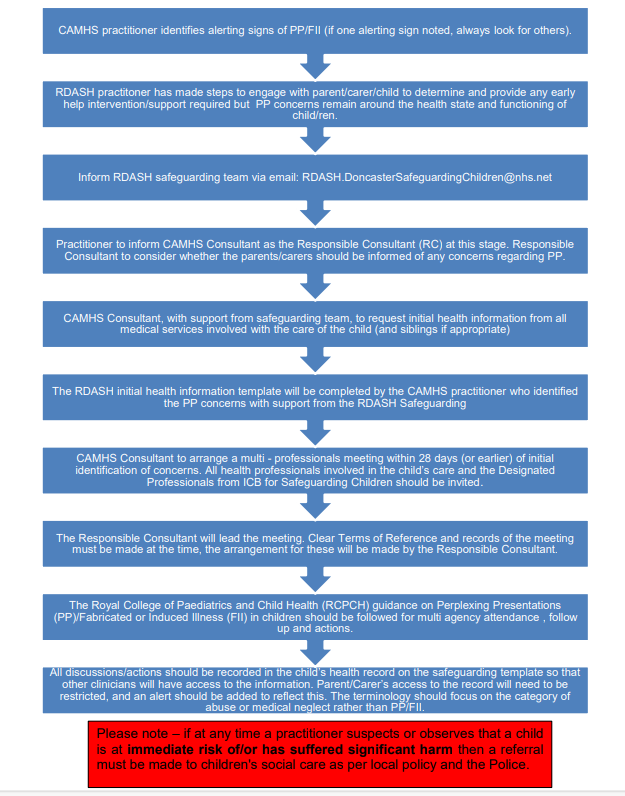
- CAMHS practitioner identifies alerting signs of PP and FII (if one alerting sign noted, always look for others).
- RDaSH practitioner has made steps to engage with parent, carer or child to determine and provide any early help intervention or support required but PP concerns remain around the health state and functioning of child or children.
- Inform RDaSH Safeguarding team via email: rdash.doncastersafeguardingchildren@nhs.net.
- Practitioner to inform CAMHS Consultant as the responsible consultant (RC) at this stage. Responsible consultant to consider whether the parents or carers should be informed of any concerns regarding PP.
- CAMHS consultant, with support from Safeguarding team, to request initial health information from all medical services involved with the care of the child (and siblings if appropriate).
- The RDaSH initial health information template will be completed by the CAMHS practitioner who identified the PP concerns with support from the RDaSH safeguarding.
- CAMHS consultant to arrange a multi professionals meeting within 28 days (or earlier) of initial identification of concerns. All health professionals involved in the child’s care and the designated professionals from ICB for safeguarding children should be invited.
- The responsible consultant will lead the meeting. Clear terms of reference and records of the meeting must be made at the time, the arrangement for these will be made by the responsible consultant.
- The Royal College of Paediatrics and Child Health (RCPCH) guidance on perplexing presentations (PP) and fabricated or induced illness (FII) in children should be followed for multi agency attendance, follow up and actions.
- All discussions and actions should be recorded in the child’s health record on the safeguarding template so that other clinicians will have access to the information. Parent and carer’s access to the record will need to be restricted, and an alert should be added to reflect this. The terminology should focus on the category of abuse or medical neglect rather than PP and FII.
Please note: if at any time a practitioner suspects or observes that a child is at immediate risk of or has suffered significant harm then a referral must be made to children’s social care as per local policy and the police.
5.1.2 PP concerns identified within any other RDaSH service
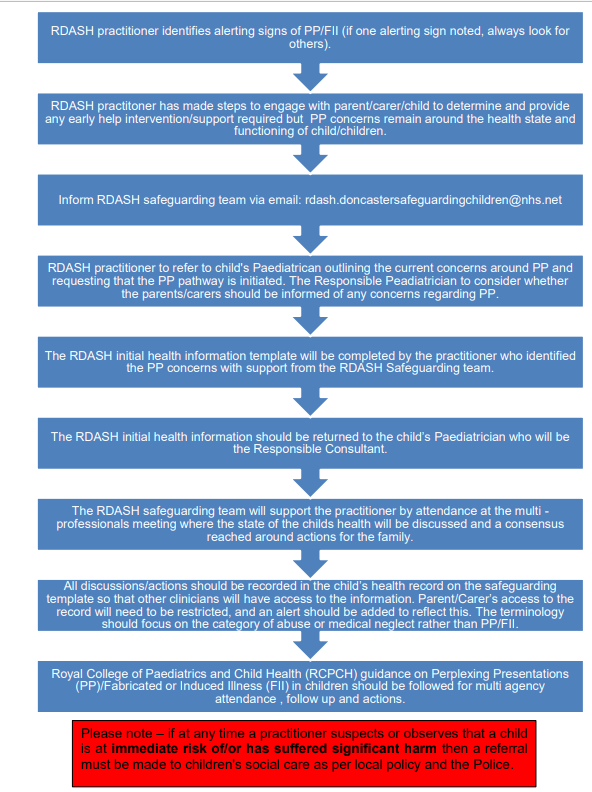
- CAMHS practitioner identifies alerting signs of PP and FII (if one alerting sign noted, always look for others).
- RDaSH practitioner has made steps to engage with parent, carer or child to determine and provide any early help intervention or support required but PP concerns remain around the health state and functioning of child or children.
- Inform RDaSH Safeguarding team via email at rdash.doncastersafeguardingchildren@nhs.net.
- RDaSH practitioner to refer to child’s paediatrician outlining the current concerns around PP and requesting that the PP pathway is initiated. The responsible paediatrician to consider whether
the parents and carers should be informed of any concerns regarding PP - The RDaSH initial health information template will be completed by the CAMHS practitioner who identified the PP concerns with support from the RDaSH Safeguarding team.
- The RDaSH initial health information should be returned to the child’s paediatrician who will be the responsible consultant.
- The RDaSH Safeguarding team will support the practitioner by attendance at the multi professionals meeting where the state of the child’s health will be discussed and a consensus reached around actions for the family.
- All discussions and actions should be recorded in the child’s health record on the safeguarding template so that other clinicians will have access to the information. Parent and carer’s access to the record will need to be restricted, and an alert should be added to reflect this. The terminology should focus on the category of abuse or medical neglect rather than PP and FII.
- Royal College of Paediatrics and Child Health (RCPCH) guidance on perplexing presentations (PP) and fabricated or induced illness (FII) in children should be followed for multi agency attendance, follow up and actions.
Please note, if at any time a practitioner suspects or observes that a child is at immediate risk of or has suffered significant harm then a referral must be made to children’s social care as per local policy and the police.
5.2 Appendix B Draft letter to request health information
5.3 Appendix C Health information template
5.4 Appendix D Draft referral letter
5.5 Definition of key terms
| Term | Definition |
|---|---|
| Fabricated or induced illness (FII) | A clinical situation in which a child is, or is very likely to be, harmed due to parental behaviour and action, carried out in order to convince doctors that the child’s state of physical and mental health or neurodevelopment is impaired or more impaired than is actually the case.
Synonyms:
|
| Perplexing presentations (PP) | Presence of alerting signs when the actual state of the child’s physical and mental health is not yet clear but there is no perceived risk of immediate serious harm to the child’s physical health or life |
| Medically unexplained symptoms (MUS) | The child’s symptoms, of which the child complains, and which are genuinely experienced, are not fully explained by any known pathology but with likely underlying factors in the child (usually of a psychosocial nature), and the parents acknowledge this to be the case. The health professionals and parents work collaboratively to achieve evidence-based therapeutic work in the best interests of the child or young person. MUS can also be described as ‘functional disorders’ and are abnormal bodily sensations which cause pain and disability by affecting the normal functioning of the body.
Synonyms:
|
| Responsible consultant | The responsible consultant has the responsibility for the initial management, including collating of current health involvement. This is either the CAMHS Consultant or the consultant paediatrician who has the main responsibility for the child’s care. If this is in dispute, the named doctor will liaise with the consultants involved to decide who the responsible consultant is to enable them to lead on the child safeguarding issues |
| Named doctor | A statutory role within NHS organisations, this doctor will support all activities necessary to ensure that the organisation meets its responsibilities to safeguard and protect children and young people (Safeguarding children and young people: roles and competencies for healthcare staff, published by the Royal College of Nursing in January 2019) |
| Designated professionals | Are clinical experts and strategic leaders, take a strategic, professional lead on all aspects of the health service contribution to safeguarding children across the area, providing support to all providers, and linking particularly with named child safeguarding health professionals, local authority children’s services, and local safeguarding partnerships, the safeguarding panel of the health and social care trust, and the NHS England |
| Identifying medical professional | The staff member or practitioner who has raised concerns of PP and FII |
| Professionals meeting and consensus meeting | A professionals meeting should include all health professionals involved with the child and family, including GPs, Consultants, private doctors, and other significant professionals who have observations about the child, including education and children’s social care if they have already been involved. The multi-professional meeting is required in order to reach consensus about the child’s state of health |
| Health and education rehabilitation plan (HERP) | Development of the health and education rehabilitation plan requires a coordinated multidisciplinary approach and negotiation with parents and children and usually will involve their attendance as appropriate at the relevant meetings. Consideration needs to be given to what support the family require to help them to work alongside professionals to implement the plan |
Document control
- Version: 1.
- Unique reference number: 1016.
- Ratified by: Clinical policy review and approval group.
- Date ratified: 3 January 2023.
- Name of originator: Named nurse safeguarding children.
- Name of responsible individual: Executive director of nursing and allied health professionals.
- Date issued: 16 January 2023.
- Review date: 31 January 2027.
- Target audience: All clinical staff.
- Description of change: New procedure.
Page last reviewed: April 29, 2024
Next review due: April 29, 2025