1 Introduction
Falls are the most reported type of patient safety incident in healthcare. The human cost of falling includes distress, pain, injury, loss of confidence, loss of independence and mortality. Up to 90% of older patients who fracture their neck of femur may fail to recover their previous level of mobility or independence (NPSA 2007). Falling also affects the family members and carers of people who fall.
People aged 65 and older have the highest risk of falling. Around 30% of adults who are over 65 and living at home will experience at least 1 fall a year (approximately 2.5 million people in England). This rises to 50% of adults over 80 who are either at home or in residential care. The risk increases in-patients with cognitive impairment and dementia.
Higher falls risk groups include:
- older people, those suffering from dementia are particularly vulnerable to falling because of cognitive impairment and associated difficulties such as loss of spatial awareness, side effects from medication, or problems with their balance, strength, or mobility
- people with cardiac, neurological, muscular-skeletal conditions, continence problems, and sensory losses and difficulties
- people with learning disabilities, who may have a combination of physical, sensory and cognitive problems
On the 17th April 2015 the trust launched the implementation of FallSafe, the Royal College of Physicians’ (RCP, 2012) endorsed approach to falls prevention for in-patients in the trust. This provided a framework for a comprehensive trust wide approach to falls for vulnerable in-patients.
FallSafe is utilised widely across the NHS and its tools and resources are highly regarded. The FallSafe approach involves educating, and supporting inpatient multi-disciplinary teams (MDT) to deliver multifactorial assessments and interventions through a care bundle approach (a care bundle comprises components which are all evidenced-based falls prevention assessments or interventions; they are introduced in phases and progress of their implementation is measured and reviewed in an approach involving all ward colleagues).
2 Purpose
The purpose of this manual is to:
- ensure an integrated multi-professional approach is adopted for the care and management of patients who are at risk of falling or have fallen
- set out the arrangements for managing risks to patients associated with slips, trips and falls
- raise awareness amongst colleagues about the need for risk identification, assessment, risk management, post fall interventions, incident reporting and learning from falls
- raise awareness amongst clinical colleagues with particular regard to service users who are in ‘high risk groups’
- reduce the risk of falls by carrying out multi-factorial falls assessment; thus recognising factors leading to falls and implementing appropriate interventions for prevention and mitigation of injury when a likelihood of falling is present
- raise awareness about Bone Health and about how osteoporosis increases the risk of harmful falls
- raise awareness of environmental issues which lead to patient slips, trips and falls
3 Scope
This is a trust wide manual which is applicable to all patients under the care of the trust. It focuses in particularly on the needs of those patients who are in the higher falls risk groups or who already have a history of falls (over 65’s and, or patients with pre-existing health conditions which means they are at a higher risk of falling).
For further information about responsibilities, accountabilities and duties of all employees, please see appendix A.
4 Definitions
| Term | Definition |
|---|---|
| Slip | A slip is to slide accidentally causing the person to lose their balance; this is either corrected or causes a person to fall. |
| Trip | A trip is to stumble accidentally often over an obstacle causing an individual to lose their balance, this is either corrected or causes an individual to fall. |
| Fall | A fall is an event which results in the person or a body part of the person coming to rest inadvertently on the ground floor or other surface lower than the person, whether an injury is sustained. |
| Near miss | A near miss occurs when someone starts to fall but either they or someone else manages to prevent them falling. It is more than being unsteady, wobbly, thinking they are going to fall. If they did not grab something or someone holds them then they would have fallen. |
5 Procedures
- Falls risk assessment procedure
- Environmental risks procedure
- Falls interventions procedure
- Medication management and falls procedure
- Falls prevention and footwear procedure
- Post fall procedure
- Mobility aid and gait training procedure
- Learning disabilities slips, trips and falls procedure (adults and children)
- Supportive falls intervention procedure
- Manual handling of the falling or fallen person procedure
- Medical assessment and management of falls procedure (including hip fracture, spinal injury and head injury)
6 Training implications
The awareness and management of slips, trips and falls is delivered by the Manual Handing team and key trainers as part of mandatory training for clinical colleagues. It includes the principles of effective risk assessment and post fall management.
There are 3 levels of training available for colleagues (ESR will state which level is required according to job role):
- level 1, falls awareness leaflet provided for all colleagues new to the trust as part of induction (clinical and non-clinical colleagues)
- level 2, an online falls training package
- level 3, face to face slips, trips and falls training delivered as part of the complex patient manual handling training.
This patient falls manual is one of the many resources available to colleagues which informs them of their roles and responsibilities with respect to falls prevention and management. Other available resources include:
- mandatory training and yearly updates
- trust wide emails or internal communications
- team meetings
- posters or leaflets or booklets
- one to one meetings or supervision, useful for de-briefing following a fall or near miss incident.
- practice development days or key trainer sessions
- local induction or e-learning packages
- falls leads, there are named falls leads in each care group
- the strategic falls lead for the trust
7 Equality impact assessment screening
To access the equality impact assessment for this policy, please email rdash.equalityanddiversity@nhs.net to request the document.
7.1 Privacy, dignity and respect
The NHS Constitution states that all patients should feel that their privacy and dignity are respected while they are in hospital. High Quality Care for All (2008), Lord Darzi’s review of the NHS, identifies the need to organise care around the individual, “not just clinically but in terms of dignity and respect”.
As a consequence the trust is required to articulate its intent to deliver care with privacy and dignity that treats all service users with respect. Therefore, all procedural documents will be considered, if relevant, to reflect the requirement to treat everyone with privacy, dignity and respect, (when appropriate this should also include how same sex accommodation is provided).
7.1.1 How this will be met
No issues have been identified in relation to this manual.
7.2 Mental Capacity Act (2005)
Central to any aspect of care delivered to adults and young people aged 16 years or over will be the consideration of the individuals’ capacity to participate in the decision-making process. Consequently, no intervention should be carried out without either the individual’s informed consent, or the powers included in a legal framework, or by order of the court.
Therefore, the trust is required to make sure that all staff working with individuals who use our service are familiar with the provisions within the Mental Capacity Act (2005). For this reason all procedural documents will be considered, if relevant to reflect the provisions of the Mental Capacity Act (2005) to ensure that the rights of individual are protected and they are supported to make their own decisions where possible and that any decisions made on their behalf when they lack capacity are made in their best interests and least restrictive of their rights and freedoms.
7.2.1 How this will be met
All individuals involved in the implementation of this policy should do so in accordance with the guiding principles of the Mental Capacity Act (2005).
8 Links to any other associated documents
- Slips, trips and falls for staff and visitors, prevention and management policy
- Medical devices management policy
- Incident management policy
- Safeguarding adults policy
- MCA Mental Capacity Act 2005 policy
- MCA deprivation of liberty (DoL) policy
- Risk management framework
- Safe and secure handling of medicines manual
- Admission, transfer and discharge manual including patient flow and out of hours (OOH) procedures
- Infection prevention and control manual
- Resuscitation manual
- Rapid tranquillisation policy and guidelines (pharmacological management of violence)
- Care of informal patients who require care in local acute hospital
- Mental health units (use of force) policy
- Vision based patient monitoring system (VBPMS) (non-contact technology) policy
- Consent to care and treatment policy
9 References
- Cochrane (2014) Hip protectors for preventing hip fractures in older people
- Cochrane (2022) Hip protectors: can they help break your fall and not your hip?
- Department of Elderly Medicine 2004. Bed Sensors Reduce In-Patient Falls. University Hospital Nottingham.
- Department of Health (2014) Positive and Proactive Care: reducing the need for restrictive interventions
- Gov.Uk, (2019, Preventing falls in people with learning disabilities: making reasonable adjustments
- Lord Darzi, Department of Health (2008) High quality care for all
- Mental Capacity Act (2005)
- National Audit of Inpatient Falls (2021) Interim Report Spring 2021
- National Patient Safety Agency (2007) Slips, trips and falls in hospital
- National Patient Safety Agency (2009) Patient safety guide: how to guide 2009
- National Patient Safety Agency (2011) Essential care after an in-patient fall
- National Patient Safety Agency (2011) The safe use of ultra-low beds, signal
- NICE (2011) CG124: National costing report: Hip fracture
- NICE (2012 updated 2017) QS16 Hip Fracture in adults
- NICE (2013) CG161 Falls in Older People: assessing risk and prevention
- NICE (2015) QS86 Falls in Older People
- NICE (2019) CG176 Head injury: assessment and early management
- NICE (2017) QS149 Osteoporosis and CG146 Osteoporosis: assessing the risk of fragility fracture
- NPSA 2007 Slips, trips and falls in hospitals Royal College of physicians (2012) FallSafe
- Royal College of Physicians (2010) Falling standards, broken promises: report of the national audit of falls and bone health
- Royal College of Physicians (2019) National Hip Fracture Database (NHFD) annual report
- Royal College of Physicians (2016) Falls and Fragility Fracture Audit Programme (FFFAP) ; National Hip Fracture Database annual report
- Royal College of Physicians (2022) Supporting best and safe practice in post fall management in inpatient settings
9.1 Further information or resources
- NHS falls fragility fractures pathway
- Falls and fractures consensus statement
- Falls and fractures consensus statement resource pack
- Chartered Society of Physiotherapy: avoid trips and falls
- Chartered Society of Physiotherapy: physiotherapy works, falls community approach
10 Appendices
10.1 Appendix A roles and responsibilities
10.1.1 The trust board directors
The trust board directors have overall responsibility for the management of health and safety and to ensure this manual is implemented in trust services.
10.1.2 The chief executive
The chief executive has specific responsibility to ensure that responsibilities for health and safety are effectively assigned, accepted and managed at all levels within the structure consistent with good practice throughout the trust.
10.1.3 The care group director
The care group director is responsible for overseeing the monitoring of the effectiveness of this manual through the relevant care group quality meetings.
10.1.4 Service managers or modern matrons, ward managers and team managers
- Make arrangements for the effective implementation and monitoring of the manual.
- Promote a positive reporting and learning culture to facilitate continuous safety improvement with regard to slips, trips, and falls. (NPSA Patient safety first falls, how to guide 2009).
- Ensure that risk assessments and risk management plans are developed and implemented.
- Support the development and delivery of training. Colleagues will need protected time to attend.
- Ensure that the working environment is safe and well maintained.
- Ensure reporting of all slips, trips and falls events via incident reporting systems.
- Ensure local monitoring and learning through theme and trend analysis and cascading of lessons learnt in their own work areas.
10.1.5 Head of patient safety or trust strategic falls lead
- Update the falls manual and associated practices and implemented in line with guidance, legislation and evidence.
- Provide advice and support to directors, and managers to facilitate effective implementation and monitoring of the manual
- Produce management reports which provide thematic and trend analysis of slips, trips and falls incident data, to inform practice development and organisational learning. The rate of harmful falls per thousand bed days is a recommended outcome measure in terms of measuring (NPSA Patient safety first falls, how to guides, 2009); also in FallSafe).
- Cascade lessons learnt from incidents.
10.1.6 Colleagues
- Undertake appropriate falls training dependent on their role.
- Be aware of service user groups who are at increased risk of falls.
- Ensure physical observations or neurological observations are completed post fall or head injury.
- Participate in the identification of environmental and clinical slip, trip and fall hazards. Report any incidents or concerns, seek advice as required and implement policies and agreed measures to manage risks.
- Wear appropriate footwear to minimise slips. Colleagues should refer and adhere to any specific dress codes in their area of work. See trust uniform and appearance at work and dress code policy.
10.1.7 The trust falls harm reduction group
- The trust falls harm reduction group will monitor a trust wide approach and action plans for falls prevention relating to patients, based on national guidance. It will provide assurance via the trust governance structure.
10.2 Appendix B monitoring arrangements
10.2.1 Analysis of incidents and actions taken or learning from incident reports
- How: Live’ visual review of a sample of IR1s via online system. Any issues related to standard of reporting and quality of actions taken subsequently feedback verbally or via e-mail.
- Who by: Head of patient safety or trust falls lead and other individuals designated by them and by senior managers.
- Reported to: Service managers or modern matrons or senior managers.
- Frequency: Information received by reviewers as it is entered on the system; review takes place asap but with minimum standard of fortnightly.
10.2.2 Analysis of incidents and actions taken or learning from incident reports
- How: Trend’ Information sharing and action planning: Sample of ‘Live’ info analysed and where trends observed this info feedback.
- Who by: Head of patient safety or trust falls lead.
- Reported to: Service managers or modern matrons or senior managers.
- Frequency: Quarterly, or sooner if issues of concern merit this.
10.2.3 Prevention and management of falls
- How: Falls paper covering performance, themes and trends regarding frequency of falls, incident reporting and risk assessment compliance submitted.
- Who by: Strategic falls lead.
- Reported to: Quality committee.
- Frequency: Bi-annually.
10.3 Appendix C post falls clinical decision-making flow chart
Please note this procedure is applicable to patients, colleagues and carers alike who sustain a fall whilst under the care of RDaSH services.
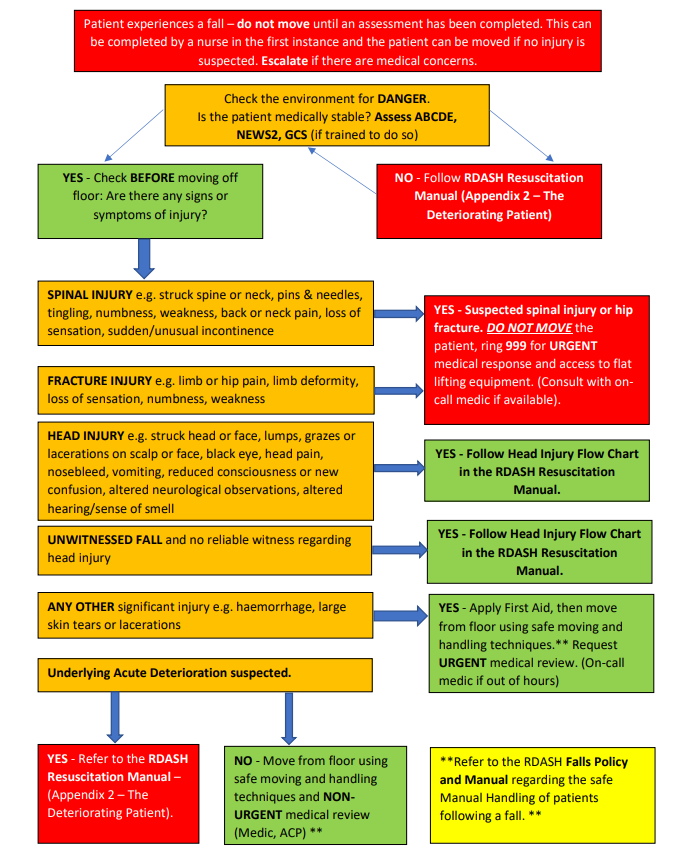
- Patient experiences a fall, do not move until an assessment has been completed. This can be completed by a nurse in the first instance and the patient can be moved if no injury is suspected. Escalate if there are medical concerns.
- Check the environment for danger. Is the patient medically stable? Assess ABCDE, NEWS2, GCS (if trained to do so).
- no, follow RDASH resuscitation manual (appendix B the deteriorating patient)
- Yes, check before moving off floor, are there any signs or symptoms of injury?
- spinal injury, for example, struck spine or neck, pins and needles, tingling, numbness, weakness, back or neck pain, loss of sensation, sudden or unusual incontinence:
- yes, suspected spinal injury or hip fracture. Do not move the patient, ring 999 for urgent medical response and access to flat lifting equipment (consult with on call medic if available)
- fracture injury, for example, limb or hip pain, limb deformity,
loss of sensation, numbness, weakness:- yes, suspected spinal injury or hip fracture. Do not move the patient, ring 999 for urgent medical response and access to flat lifting equipment (consult with on call medic if available)
- head injury, for example, struck head or face, lumps, grazes or lacerations on scalp or face, black eye, head pain, nosebleed, vomiting, reduced consciousness or new confusion, altered neurological observations, altered hearing or sense of smell:
- yes, follow head injury flow chart in the RDASH resuscitation manual
- unwitnessed fall and no reliable witness regarding head injury:
- yes, follow head injury flow chart in the RDASH resuscitation manual
- any other significant injury, for example, haemorrhage, large skin tears or lacerations:
- yes, apply first aid, then move from floor using safe moving and handling techniques (refer to the RDASH falls policy and manual regarding the safe manual handling of patients following a fall). Request urgent medical review (on-call medic if out of hours)
- Underlying acute deterioration suspected:
- yes, refer to the RDASH resuscitation manual (appendix B the deteriorating patient)
- no, move from floor using safe moving and handling techniques and nonurgent medical review (medic, ACP) (refer to the RDASH falls policy and manual regarding the safe manual handling of patients following a fall)
- spinal injury, for example, struck spine or neck, pins and needles, tingling, numbness, weakness, back or neck pain, loss of sensation, sudden or unusual incontinence:
10.4 Appendix D post falls incident reporting process
- Patient fall.
- Immediately, post-fall clinical decision-making flow chart is followed.
- Within 24 hours of the incident, IR1 incident report completed by the person who witnessed or managed the fall.
- 10 days, moderate harm incident or above, falls review to be completed by person who witnessed the fall with support from senior clinician (B6 and above). Follow section 10.4.1.
- 4 to 6 weeks, witness, senior clinician and falls lead attend falls panel to present falls review. If lapse in care, SI process initiated at this stage. Follow section 10.4.1.
- Next ward or care group meeting, any actions, learning from falls panel shared at ward, care group, trust wide level.
- Quarterly falls leads report, falls report reflecting the outcome from the incident and any actions or learning. End process.
10.4.1 Reporting and incident reporting process
Escalation to service manager or senior leadership team.
Duty of candour process is commenced. Letter drafted to the patient or patients’ family apologising for the harm incident and advising them of the investigation process. This must be completed within 10 days of the incident.
Following falls panel, the outcome will be shared with family as part of the DOC process. If there have been significant lapses in care, this means informing the patient.
10.5 Appendix E list of medications and their impacts on falls
Refer to appendix E: list of medications and their impacts on falls (staff access only).
10.6 Appendix F Falls equipment and locations within the trust
Woodlands Rotherham (shared between Glades and Brambles ward):
- Raizer
- ELK
- hoist
Swallownest Rotherham (shared between wards):
- ELK
- hoist
Great Oakes, Scunthorpe (shared between Laurel and Mulberry wards):
- Raizer
- ELK
- hoist
Magnolia Ward, Doncaster:
- Raizer (stored on Hazel)
- hoist
- ELK
Hazel or Hawthorn, Doncaster:
- Raizer
- hoist
St Johns Hospice, Doncaster:
- ELK
- hoist
- Raizer
Rapid response or unplanned team Doncaster:
- ELK
Skelbrooke, Doncaster
- ELK
Windermere or Brodsworth or Cusworth Doncaster:
- ELK
- Raizer
- hoist
Maintenance of the above equipment is the responsibility of the individual ward or service area.
10.7 Appendix G FallSafe audit
Refer to appendix G: FallSafe audit (staff access only).
10.8 Appendix H medical considerations
On some inpatient units there will not always be a doctor on site especially out of hours. However some patients will need urgent medical examination and arrangements must be made accordingly. For patients with no obvious need to be urgently examined, examination needs to take place within a reasonable timescale.
Medical examination is important not only to detect injury but because falls are often a ‘red flag’ for changes in the patient’s underlying medical condition. If the patient has been immobilised as a precautionary measure, access to investigation and treatment must be speedy to avoid the risk of prolonged immobilisation and associated complications.
Despite the difficulty in taking a reliable history in some patients, an attempt should always be made to find the cause of the fall. Hypotension is often an aetiological factor, exacerbated by medication such as diuretics, beta-blockers and sedatives. The Parkinsonian patient is at particular risk due to postural instability and orthostatic hypotension. The diabetic patient is also prone to falls due to poor vision, peripheral and autonomic neuropathy and hypoglycaemia.
Hip fracture may be the first presentation of osteoporosis or the patient’s osteoporotic treatment not effective or Paget’s disease or Metastatic bone disease, when fracture may follow minimal trauma, with the fall resulting from the fracture rather than the other way round. Cancers that commonly metastasise to bone are those arising in bronchus, breast, kidney, and prostate.
10.8.1 Medical assessment must include
10.8.1.1 Subjective assessment
- History of patient including whether they have a diagnosis or high risk of osteoporosis.
- Mechanism of injury.
- Whether the patient is on coagulation therapy.
- Is the patient an insulin dependent diabetes mellitus (IDDM).
- Any changes in NEWS or patient observations as reported by nursing colleagues.
- Predisposing factors, sudden collapse or dizziness or chest pain.
- Complaints of pain (neck and back for spinal injury, groin or hip region for femoral fracture).
- For patients with cognitive impairment, pain assessment should be made through the use of a rating scale such as the Abbey pain score if the patient is unable to report pain. This can be found in SystmOne.
- Any changes in the patient’s presentation, for example, increased agitation, consciousness level (brain injury or concussion).
10.8.1.2 Objective assessment
- Suspicion of injuries, spinal injury, head injury or fracture or dislocation.
- Examination cardiovascular, respiratory, orthopaedic and Neurological systems.
- Examine the position of the leg and foot for signs of shortening or rotation of limb. Note, impacted, un-displaced fractures may present diagnostic difficulty and there may be no shortening or rotation.
- Inability to move affected limb or weight bear.
- Unable to walk or changes in gait pattern.
- Inspect the skin or cuts or abrasions or bruising, over the greater trochanter for suspected hip fracture.
- Gently palpate to identify area of bony tenderness.
- Check if patient has sensation to the sole of the foot and palpate pedal pulse.
- Advise nursing colleagues on monitor blood pressure (BP), pulse and respirations for signs of hypovolemia.
- Request nursing colleagues record core temperature.
10.8.2 Further observations to be taken when appropriate and possible following head injury
10.8.2.1 AVPU scale
Alert, verbal, pain, unresponsive, to add section.
10.8.2.2 Glasgow coma scale (GCS)
The preferred measure of central nervous system (CNS) state is the AVPU score as discussed previously. In most cases a person’s consciousness will have deteriorated before observations start to alter, therefore any change in a person’s AVPU score will mean action is required. Within RDASH the GCS score will be calculated by the attending paramedic or doctor unless carried out in area where colleagues are competent in its use.
In clinical areas where the GCS is used frequently, such as the neuro rehabilitation unit and the colleagues are competent in its use, then the GCS should be used as part of the post head injury observations.
10.8.2.3 Temperature
The hypothalamus is the thermo-regulator in the brain, any raised inter cranial pressure will affect the ability to regulate the temperature and therefore there may be a fluctuating temperature.
10.8.2.4 Blood pressure
After a head injury the blood pressure may rise in an attempt to perfuse the brain or fall as a result of a slowed pulse rate. Medical advice and care planning to be in place regarding the blood pressure parameters for individual patients.
10.8.2.5 Pulse
After a head injury the pulse may slow as the body attempts to compensate for an increase in intracranial pressure.
10.8.2.6 Pupil response
A change in the pupil size and reaction can be an indication of raised inter cranial pressure and therefore the compression of the optic nerve after head injury.
10.8.2.7 Notes for completing pupil checks
- Each pupil should be recorded separately.
- Are the pupils of equal size.
- Assess the pupils for their size and shape using a measure of 1 to 9 see the diagram on the observation chart.
- Reaction to light, rapid constriction to light is recorded as a positive reaction; no constriction is recorded as a negative reaction. A slow reaction should be recorded as sluggish.
- Move a light from the outer aspect of the eye directly over the pupil, the pupil should constrict quickly and dilate again when the light is moved away. Both eyes should constrict when a light is shone into one eye.
- In a patient with slight swelling an attempt should be made to open the eye if at all possible.
- If a person refuses to open their eyes document refused to open eyes. If this is a change from their normal behaviour it should be documented as this is a change to presentation after head injury, but if this is normal behaviour document refusal as normal behaviour.
10.8.2.8 Limb movement or motor function
When checking motor function we must be aware of the person’s normal function and record if needed.
Check the limbs for:
- normal power, usually the patient will be able to push against or squeeze with no difficulty
- mild weakness, a change or reduction, usually they will be able to push against but will be over come easily
- spastic flexion, bending or flexing the limb that is not the usual, if this is the person’s normal function they would score for normal presentation
- extension, straightening or extending that is not the normal function, if this is the person’s normal function they would score for normal presentation
- no response, again a change from normal presentation
The response should be checked by giving simple commands, squeeze my hands, lift your legs etc. If there is no response to commands and this is a change from normal behaviour, painful stimuli should be used to re-asses. Suborbital pressure can be used, rub finger along bony rim above eye, or trapezius squeeze, use the thumb and 2 fingers to squeeze the muscle.
Always record all possible observations after head injury on a neuro observation chart, with any additional observations noted clearly within the electronic patient record.
If working in an area where physical observations are not carried out as a matter of course, ensure person is closely ‘watched’ and the advice on when to call an ambulance or doctor is followed. It must be considered good practice to always record, as a minimum, a person’s consciousness level and at least, depth and rate of breathing.
Document control
- Version: 10.1.
- Approved by: Clinical policies review and approval group.
- Date approved: 1 August 2023.
- Name of originator or author: Clinical team leader.
- Name of responsible committee or individual: Executive director of nursing and allied health professionals.
- Date issued: 23 August 2023 (minor amendment).
- Review date: 31 August 2026.
- Target audience: Clinical staff.
- Description of changes: New manual.
Page last reviewed: June 25, 2025
Next review due: June 25, 2026
Problem with this page?
Please tell us about any problems you have found with this web page.
Report a problem