Contents
1 Policy summary
This policy details the trust approach and expected standards in the use of a vision based patient monitoring system (VBPMS). This assistive tool enables colleagues to enhance and support patient safety in inpatient services by delivering noncontact measurement of physiological parameters such as pulse and breathing rate, some degree of patient location, activity or behaviour data and some form of contextual video information (which may be blurred) either in real time or through subsequent reviews. The use of this system is intended to compliment clinical practice and not replace the need for good nursing interventions.
VBPMS must be prescribed in a person-centred way and supported by clear and frequent communication, regular reviews by the Multidisciplinary team (MDT), clear and collaborative care planning, and therapeutic engagement with the clinical team.
Data captured by VBPMS is used by Rotherham, Doncaster and South Humber Trust (RDaSH) to enhance patient safety and activity monitoring regimes.
2 Introduction
RDaSH is utilising VBPMS to enhance the delivery of safe and effective mental health care by introducing solutions to proactively manage and prevent incidents.
The trust has considered the National recommendations, guidance and best practice On safe use Of VBPMS (opens in new window) in the development of this policy.
This policy details the processes to be followed when using VBPMS. The use of the system will align to and compliment traditional working practices and relevant RDaSH policies.
VBPMS does not replace positive and therapeutic engagement with patients and the visible presence of colleagues within inpatient settings. Colleagues must remain responsible for the patient and clinical judgement must always be used.
3 Purpose
The purpose of this document is to provide colleagues with clear guidance on VBPMS, to help plan, review and optimise treatment for patients whilst making the best use of resources.
The trust currently deliver VBPMS via Oxevision which uses an optical sensor (camera and infrared illumination in a secure housing on the wall and is operational 24 hours a day, 7 days a week) supporting colleagues to:
- take cardio-respiratory measurements remotely
- access cardio-respiratory trends from the last 24 hours to understand if a resting patient’s physical health may be deteriorating
- receive real time alerts to high risk activity, prompting a safety check
- view objective patient activity reports to support clinical decision making
The technology is not closed circuit television (CCTV), and colleagues should not attempt to use it in this way. Colleagues should refer to the trust security policy for further information on CCTV.
4 Scope
This document is intended for use by colleagues where Oxevision is deployed. Please refer to the Oxevision intranet page for further details of where and how Oxevision is deployed across the trust.
The policy should be read in conjunction with:
- supportive therapeutic observation policy
- physical health policy
- patient falls manual (prevention and management)
- resuscitation manual
- consent to care and treatment policy
- healthcare record keeping policy
- Mental Capacity Act policy
5 Procedure or implementation
Oxevision is available for use in patient and seclusion rooms across all adult and older adult mental health inpatient services to enhance and support patient safety.
5.1 Quick guide
5.1.1 Competency and training
- Oxevision champions (confirmed by each ward) who have completed train the trainer education will train further colleagues.
- Colleagues must be trained by a Oxehealth champion before using Oxevision, including reading the trust vision based patient monitoring system policy before signing appendix E.
5.1.2 Patient Information
- Colleagues must ensure that patients and family, carers and visitors are informed on admission that the trust utilise Oxevision to promote safety.
- An information pack should be provided to patients on admission detailing what, when and how patient activity and pulse and respiration rates are monitored.
5.1.3 Consent and capacity
- Patients should be able to discuss queries or concerns they may have about Oxevision with the clinical team including objecting to it use.
- If capacity is doubted a MCA 1 form should be undertaken. If a patient is accessed as lacking capacity a best interest’s decision should be made including family or carer’s view and evidenced on MCA 2.
5.1.4 Physical observation
- Oxevision can be used to monitor pulse and respiration rates only.
- Where a patient requires regular physical observations, it is expected that he pulse and respiration are taken manually alongside other identified physical observations, not a combination of Oxevision and manual.
5.1.5 Therapeutic observations
- Where deemed clinically appropriate, Oxevision enables the patient to be monitored without having to physically enter their room to undertake the observation. This could promote sleep at night or reduce agitation.
5.1.6 Seclusion
- Oxevision must never be paused in the seclusion environment.
5.1.7 Incidents
- Any request for video footage must be directly linked to a patient related incident.
- Request for data can be made by all registered professionals of the MDT to support@oxehealth.com or by contacting customer services on 08000 306781. Full guidance can be read in 6.10.
5.2 General guidance and principles of use
- All patients and their family, carers and visitors must be informed on admission that the trust utilise Oxevision to promote safety.
- Any decision to use Oxevision should be made on a case-by-case basis in a person centred way.
- The use of Oxevision should be on the basis that there is a legitimate and proportionate aim that is both lawful and fair and it should not be assumed by colleagues that it is to be implemented for each patient in a blanket way.
- Where a decision has been made to use or not use Oxevision, the discussion with the patient and other relevant people where appropriate, such as carer or family, other members of the MDT etc., as well as the intended aims of use should be recorded in the clinical record.
- All patients must have an Oxevision care plan in place reflecting their decision. Colleagues must use and personalise the standard Oxevision care plan in SystmOne.
- It is the responsibility of the nurse in charge to ensure that Oxevision is used only by colleagues who are suitably trained. Please refer to section 6 training implications for further guidance.
- When undertaking an observation, it is important that a patient’s privacy and dignity is adequately considered and protected. There may be instances when it is not appropriate to continue with an observation, for example:
- if a patient is in a state of undress
- patient is engaging in sexual activity (masturbation)
- if a patient is privately observing religious beliefs
- An observation should be cancelled immediately in these circumstances if no risk is evident and reattempted later.
- When an alert is received or a check is performed, colleagues will see a live stream of the patient for 15 seconds only, alerts are blurred images.
- All incidents observed or highlighted via Oxevision must be reported in line with the trust incident management policy and recorded in the EPR in line with appendix F recording Oxevision incidents in SystmOne
5.3 System functionality
Oxevision has 3 core functions that can be used independently or collectively to support therapeutic and physical health observations:
- observations
- vital signs
- alerts
On admission and where appropriate thereafter, colleagues and subsequently the MDT should consider the clinical benefits of each function, and if they should be offered and, or used to support the patient.
Colleagues should refer and adhere to the respective polices relating to observations to ensure appropriate clinical considerations and decision making is undertaken.
The patient record must reflect the decisions to use the varying functionality, including the clinical rational. Where a decision to use Oxevision as an alternative to manual or in person observations in reached, this must be clearly rationalised, documented and should be reflected in the patient care plan.
A useful flowchart on assisted observations can be found in appendix C.
5.3.1 Observations
Oxevision may be a helpful addition to support in person observations:
- if entering the patient’s bedroom causes them to become more agitated and distressed
- informing whether another patient has entered the room through a room entry alert
Oxevision allows for the patient to be monitored without having to physically enter their room to undertake the observation. Colleagues can only rely on the use of the Oxevision to support these observations, with visual assurance that the patient is either awake and alert, or asleep with clear signs of breathing via the video functionality, in addition to taking a pulse and respiration reading. This functionality should not be routinely used during the day where colleagues should continue to undertake in person visual checks. If there are any concerns regarding the patient’s presentation or any uncertainty regarding the patient’s health via the camera or pulse and respiration reading, colleagues must complete an in-person assessment.
5.3.2 Physical health observations (vital signs)
Oxevision records the basic health observations of pulse and respiration. If additional physical health readings are required, such as blood pressure and oxygen saturation levels, this should be completed in line with relevant trust process. When physical health observations are taken, colleagues will see a live stream of the patient for 15 seconds only.
Where a patient requires regular physical observations, it is expected that the pulse and respiration rates are taken manually alongside other identified physical observations, not a combination of Oxevision and manual.
Oxevision does not measure pulse and respiration rate when a patient is moving. Upon observation, if the patient is moving, record their position and reattempt when the patient is still.
Colleagues can make two attempts to establish a patient’s breathing rate via Oxevision before physically locating the patient and manually measuring their breathing rate.
If colleagues have any concerns about the patient’s physical state, they must escalate as per the trust’s physical health policy. If a reading (pulse or respiration rate) is abnormal, colleagues should confirm the reading manually before escalating unless there are clear visual signs of deterioration.
Oxevision vital signs is a certified medical device, however, if there are any concerns when using the system, patients should be assessed in person.
Emergency intervention does not need to be delayed by first checking Oxevision. Clinical judgement should be exercised to determine the most appropriate response for each situation.
5.3.3 Alerts
Oxevision provides information and notifications to colleagues about a patient’s location in their room.
When an alert is sounded, colleagues can initially view the alert through an anonymised (blurred) image and assess if a physical check is necessary to maintain patient safety.
Colleagues have the option to temporarily pause these alerts for up to 30 minutes while they are delivering personal care to individual patients.
The replay last alert function enables colleagues to view an anonymised (blurred) clip of the last alert that was triggered in a patient room. The clip will show 5 minutes before and after the alert, allowing colleagues to review why the alert was triggered and help determine the appropriate course of action they should take. Only the last alert triggered is viewable within a 24 hour period.
Colleagues should also consider the need to preserve data longer term for further investigation and should refer to section 6.10 requesting and approving data for investigation for further guidance.
5.4 Seclusion
Oxevision is intended to enhance the visual and physical observation detailed in the seclusion policy, it cannot replace the need for constant observation but offers additional intelligence and may enable colleagues to monitor the patient’s physical health more frequently and without having to enter the seclusion room where such action may increase risk or distress.
Oxevision should not be paused in the seclusion environment as it is an additional aid to support a patient who is already subject to constant observation.
A mobile Oxevision tablet will be located within seclusion areas and should be activated on admittance of a patient, enabling colleagues to monitor the patient in line with this policy.
5.5 Falls
Oxevision can be used to assist with falls prevention and management by:
Alerting colleagues when the patient is in the process of exiting the bed;
- alerting colleagues when the patient is out of their bed through an out of bed alert
- notifying colleagues when the patient enters the bathroom
- viewing footage after a patient has fallen to check for any contributing factors so subsequent mitigations can be applied
5.6 Changes to room layout
Oxevision can automatically detect when a bed is moved slightly, for example, for cleaning, and when a bed is raised and lowered.
However, Oxevision cannot automatically detect when a bed is moved significantly, for example: to the other side of the room or rotated by 90 degrees. This could affect the accuracy of “in bed” room states and some alerts, particularly leaving bed and out of bed alerts.
If a bed has been moved significantly from its original position, colleagues must inform Oxehealth as soon as possible via the Feedback button within the app or via the 24 hours a day, 7 days a week support line (0800 030 6781) so appropriate adjustments can be made. Oxehealth must also be informed if the furniture within a room has moved, for example, wardrobes or other large items, so they can ensure the optical sensor is not obscured.
5.7 Patient information
On admission, and where appropriate thereafter, colleagues will discuss the purpose of Oxevision with the patient, including, how it works in relation to patient activity, pulse and respiration rates and issues of privacy, which may be compromised when an observation is attempted. This discussion will be supported by written information and must include a patient leaflet (staff access only) (opens in new window).
There are also options available to the patient regarding how Oxevision can be implemented, including the alert system alone being utilised (for example, colleagues not accessing the camera or vital signs functionality unless triggered by an alert).
Patients should be encouraged to explore any queries or concerns they have, and colleagues should address these where possible or escalate where support is required. Colleagues should utilise the wider resource available on the Oxehealth intranet page (opens in new window) to support these conversations.
The outcome of this discussion should capture the patient’s choice regarding the use of Oxevision and must be recorded in the EPR.
If Oxevision is to be used, further exploration regarding privacy should determine what the patient would like to happen if a compromise occurs. This may include informing the patient regarding what was observed, or simply a polite reminder that Oxevision is in operation. The steps agreed must be detailed in the care plan.
Oxevision signage showing the use of the equipment must be displayed clearly in public areas. Colleagues should refer to the Oxehealth intranet page (opens in new window) to access and print the patient poster.
Information around Oxevision should be shared with the patient’s family, carers, and visitors at the earliest opportunity.
More information about how the trust uses data is outlined in the trust’s privacy notice or by contacting the data protection officer (DPO) or the Information Governance team.
5.8 Making a decision regarding the use of Oxevision
On admission the admitting nurse will consult with the MDT and consider the clinical appropriateness of Oxevision, taking into account the best interest of the patient, balancing individual preference, safety, risk management and alternative options, just as they would other treatment approaches. Support should be requested from senior colleagues where appropriate, including on call support structures out of hours.
Where Oxevision is deemed clinically appropriate to support care, and the patient objects at any point during admission, consideration should first be given to their capacity to make a decision about the use of Oxevision. If there are no concerns regarding capacity, the decision should be respected if clinically appropriate.
If capacity to consent regarding Oxevision is doubted, an assessment of capacity must be undertaken. If the patient lacks capacity to make the decision, a decision must be made by the MDT in the patient’s best interests. Colleagues should refer to the trust’s Mental Capacity Act policy for further guidance. This process should be followed for both informal and detained patients.
All decisions relating to the use or withdrawal of Oxevision, including best interest decisions, must be reviewed by the responsible clinician (RC), consultant in charge, approved clinician (AC), consultant on call and the MDT as soon as is practicable within 24 hours. As these decisions are not medical emergencies, the MDT discussions should ordinarily take place during the day shift hours.
This approach needs open and honest communication with the patient and their representatives. Patients should be supported where appropriate to approach Advocacy Services.
All decisions relating to the use or withdrawal of Oxevision must be reflected in the care plan to ensure the MDT retain oversight and tailor treatment accordingly. Decisions should be reviewed weekly, in line with relevant legislation or where there is a significant change in presentation.
A quick glance decision making flow chart can be found in appendix C.
Please note: If the system is switched off for an individual room, it must be manually switched back on again when required. An Oxehealth check should be performed for each admission to ensure the system is active and working correctly.
5.9 Functionality development approval process
To submit a change request regarding functionality, colleagues must follow the steps below:
- complete Oxehealth feedback form via the Oxehealth system, Oxehealth to acknowledge receipt and seek clarity where required
- Oxehealth to seek approval from RDaSH head of patient safety (patient safety specialist) or deputy director of organisational learning and inquests
- Oxehealth to consider viability of request and advise on challenges or blockers
- Oxehealth to action change and confirm with trust
5.10 Requesting and approving data for investigation
Oxehealth data can be used to support investigations and must be requested and provided by Oxehealth as described in the process below. Any request for data should be directly linked to a patient related incident.
Video footage is available in clear and anonymised (blurred) formats depending on how quickly data is requested. Clear video footage is only available for 24 hours from the point of recording.
- Requests for data can be made by all registered professionals of the MDT to support@oxehealth.com or by contacting customer services on 0800 030 6781. The Incident Report (IR1) number must be referenced in the request to support the authoriser in the decision to release footage.
- Oxehealth will save the data and request permission to release it to the trust from the head of patient safety (patient safety specialist) or deputy director of organisational learning and inquests. Requests should be sent to RDASH.PatientSafetyTeam@nhs.net.
- Once approved, Oxehealth will save the data to a universal serial (USB), issue a password and arrange for the USB to be delivered to the respective modern matron, the head of patient safety (patient safety specialist) or deputy director of organisational learning and inquests within 72 hours.
- The modern matron, head of patient safety (patient safety specialist) or deputy director of organisational learning and inquests will contact the server and storage specialist in IT services or the IT service desk to log a call, inform of a new incident and request that a new top level digital folder is created in the trust’s secure video folder (R:\Secure Video).
- The IR1 number for the respective incident will determine the folder name (for example, IR1.134508).
- The modern matron, head of patient safety (patient safety specialist) or deputy director of organisational learning and inquests will:
- have permission to store and save footage into the sub folders
- create a sub folder for each incident which should be named in reference to the incident date and location for example, 20210810_Woodlands
- determine appropriate access and add permissions accordingly
- upload the video footage and ensure it can be viewed in full from the new location
- retain the USB in safe storage until any associated investigation is concluded. At which point the USB content should be erased and the USB sent to the trust IT department for safe disposal
- Outside of normal working hours, where there is a clinical need to view footage urgently, the nurse in charge should seek approval from the on-call manager. Footage should be viewed directly from the USB and standard process should resume for saving, retention and deletion.
Where there are data protection queries or a request to use video footage outside of its original purpose, colleagues should liaise with the DPO for advice and guidance.
The lead investigator should consider how colleagues will be supported and debriefed when viewing footage.
5.11 Data retention and deletion
Footage stored on the trust’s secure video folder (R:\Secure Video) must be retained in line with NHS record code of practice (opens in new window). Retention timescales may vary depending on the original reason for storage.
5.12 Oversight
The partnership board meets quarterly and provides the trust and Oxehealth with the opportunity to discuss overall use of the system, developments and highlight any issues that need to be resolved.
The digital community of practice meets bimonthly and provides an opportunity for clinicians and front-end users of the system to reflect on practice, raise issues for discussion and action directly with Oxehealth, it also provides an opportunity for Oxehealth to share developments directly with RDaSH colleagues.
5.13 Business continuity plan
If for any reason there is a technical failure or malfunction of Oxevision, then colleagues must revert to the manual taking and recording of observations and ensure that the appropriate supporting clinical policies and any local working instructions or agreements are followed.
All faults should be reported to Oxehealth. Any connection issues need to be reported to both Oxehealth and RDaSH IT service desk.
Please also refer to your local business continuity plan.
6.14 Escalations
Concerns regarding Oxevision functionality should be escalated to the ward manager and Oxehealth.
Concerns regarding consent, privacy and information governance should be escalated to the mental capacity lead and head of information governance respectively.
Concerns regarding safety should be raised with line managers and the Patient Safety team or via freedom to speak up (staff access only) (opens in new window).
6 Training implications
Training for Oxevision is delivered through a train the trainer model.
Each ward Unit will have several Oxevision champions who have completed train the trainer Education and who are responsible for training further colleagues.
It is the responsibility of each matron to ensure they have sufficient Oxehealth champions to deliver training to the wider team.
Colleagues must be trained by a Oxehealth champion, read the trust vision based patient monitoring system policy and sign appendix E before using the system.
Oxehealth offer a variety of ongoing support which is accessible through different formats:
- annual visits to each ward which includes refresher training sessions
- monthly online global training session where colleagues can book sessions that suit their working schedule
- an online learning platform called OxeAcademy offering refresher training and user guides. Colleagues can sign up with their trust email, and by selecting RDaSH from the ‘organisation name’ drop down
It is important that colleagues using the system provide regular feedback (sent via the monitor) to support troubleshooting.
Additional technical support will be provided by Oxehealth via:
- Email: support@oxehealth.com
- Customer service phone line for urgent technical issues: 0800 030 6781
Most technical issues will be resolved remotely. Where onsite support is required from Oxehealth, attendance will be between 24 and 72 hours provided access can be facilitated.
7 Equality impact assessment screening
The completed equality impact assessment for this policy has been published on this policy’s webpage on the trust policy library or archive website. Link to overarching EIA.
7.1 Privacy, dignity and respect
The NHS Constitution states that all patients should feel that their privacy and dignity are respected while they are in hospital. High Quality Care for All (2008), Lord Darzi’s review of the NHS, identifies the need to organise care around the individual, ‘not just clinically but in terms of dignity and respect’.
As a consequence the trust is required to articulate its intent to deliver care with privacy and dignity that treats all service users with respect. Therefore, all procedural documents will be considered, if relevant, to reflect the requirement to treat everyone with privacy, dignity and respect, (when appropriate this should also include how same sex accommodation is provided).
7.1.1 How this will be met
All colleagues, contractors and partner organisations working on behalf of the trust must follow the requirements of this policy and other related policies, particularly those relating to information governance. All health professionals must also meet their own professional codes of conduct in relation to confidentiality.
7.2 Mental Capacity Act 2005
Central to any aspect of care delivered to adults and young people aged 16 years or over will be the consideration of the individuals capacity to participate in the decision making process. Consequently, no intervention should be carried out without either the individual’s informed consent, or the powers included in a legal framework, or by order of the court.
Therefore, the trust is required to make sure that all staff working with individuals who use our service are familiar with the provisions within the Mental Capacity Act (2005). For this reason all procedural documents will be considered, if relevant to reflect the provisions of the Mental Capacity Act (2005)to ensure for that the rights of individual are protected and they are supported to make their own decisions where possible and that any decisions made on their behalf when they lack capacity are made in their best interests and least restrictive of their rights and freedoms.
7.2.1 How this will be met
All individuals involved in the implementation of this policy should do so in accordance with the guiding principles of the mental capacity Act 2005.
8 Links to any other associated documents
- Supportive therapeutic observation policy
- Physical health policy
- Patient falls manual (prevention and management)
- Resuscitation manual
- Consent to care and treatment policy
- Healthcare record keeping policy
- Mental Capacity Act policy
- Oxevision (opens in new window)
- Trust incident management policy
- Trust’s privacy notice
- Information Governance team
- Security policy
- Advocacy services
- NHS record code of practice (opens in new window)
- Freedom to speak up (staff access only) (opens in new window)
9 References
10 Appendices
10.1 Appendix A Responsibilities, accountabilities and duties
The trust has a duty of care to ensure that all aspects of patient safety are properly managed and where appropriate the trust has the correct assistive tools in place to enhance and support patient safety. The trust must adhere to the legislative, statutory, and good practice guidance.
The chief executive has overall accountability and responsibility for patient safety within the trust. This function is delegated to the executive medical director and the executive director of nursing and allied health professionals, who are responsible for driving high quality safety standards ensuring that the correct infrastructures and systems are in place.
The trust’s executive medical director and the executive director of nursing and allied health professionals are responsible for driving high quality safety standards ensuring that the correct infrastructures and systems are in place.
Caldicott guardian is responsible for protecting the confidentiality of patient and service user information and enabling appropriate information sharing.
Senior information risk owner (SIRO) is an executive board member with allocated lead responsibility for the organisation’s information risks.
Data protection officer is responsible for ensuring the organisation processes, the personal data of its colleagues, customers, providers or any other individuals (also referred to as data subjects) in compliance with the applicable data protection rules.
The chief nursing information officer and clinical safety officer is responsible for ensuring that assistive tools are clinically appropriate and adhere to clinical safety guidelines.
The deputy director of organisational learning and inquests and head of patient safety (patient safety specialist) are responsible for oversight of the Oxehealth contract, developments to the system and authorising release of secure data.
Senior managers of the trust are responsible for ensuring that assistive tools are appropriately deployed and used in their clinical areas.
Ward managers are responsible for ensuring assistive tools are used appropriately within their ward environments including monitoring colleagues training and compliance and requesting developments to the system and secure data for patient safety incidents.
The nurse in charge is responsible for ensuring appropriately trained colleagues use the system.
Oxehealth champions are responsible for completing the train the trainer education programme and ensuring identified colleagues are trained competently. Oxehealth champions should also remain engaged with Oxehealth regarding refresher training and product updates.
Ward based colleagues are responsible for using the system in line with this policy and training.
The MDT is responsible for the use or non use and review of Oxevision supported by the responsible clinician.
10.2 Appendix B Monitoring arrangement
10.2.1 Incidents
All incidents must be reported using the trust’s safeguard incident reporting system (IR1). When recording an incident involving the Oxevision system, colleagues should indicate this on the incident form using the appropriate tick box.
Incidents will be subject to review by the matron for the service, the head of patient safety (patient safety specialist) or deputy director of organisational learning and inquests.
10.2.2 Documentation
Ward managers will monitor compliance with policy, care plans and MCA assessments through localised documentation audits and RePortal report.
Matrons will oversee compliance through the trust RePortal and oversight and escalation of ward audits.
10.3 Appendix C Assisted observations process flowchart
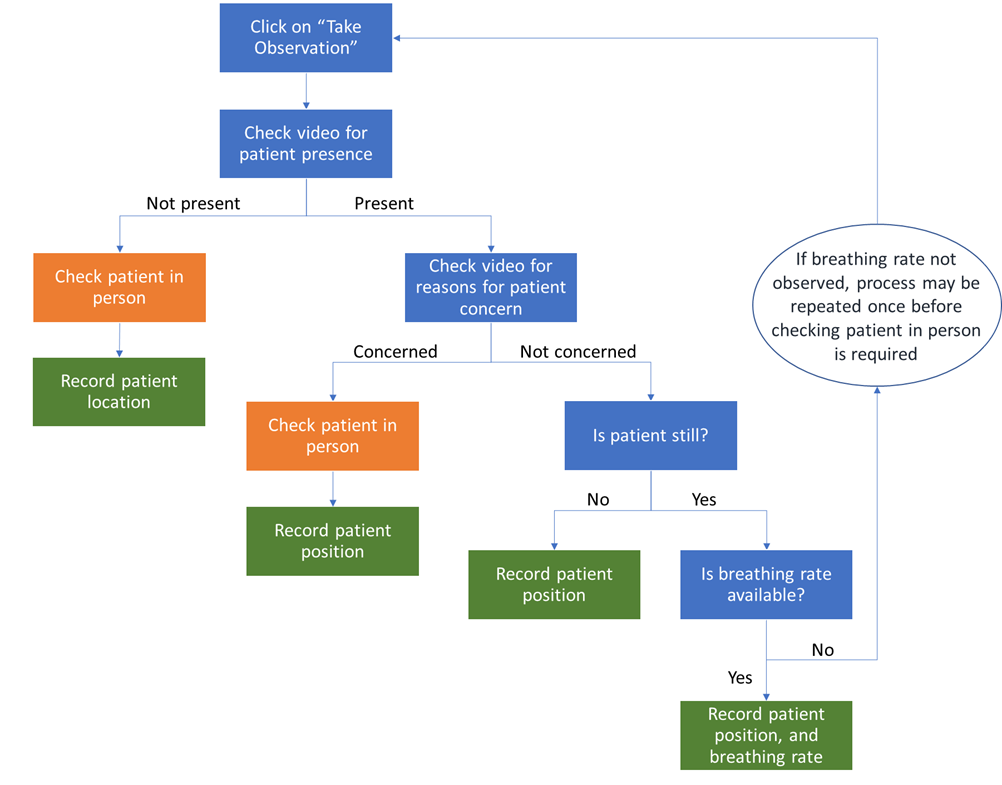
- Click on “Take Observation”
- Check video for patient presence:
- not present, check patient in person
- record patient location. End process
- Check video for reasons for patient concern:
- concerned, check patient in person
- record patient location. End process
- Not concerned, is patient still?
- no, record patient location. End process
- Yes, is breathing rate available?
- yes, record patient position, and breathing rate
- No, go to step 1.
10.4 Appendix D Quick glance decision making flowchart
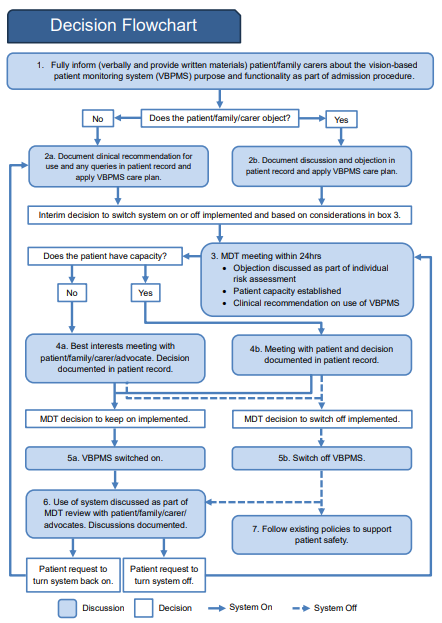
10.4.1 Flowchart description
- Fully inform: make use of materials contained within the resource pack. These materials should be made available in all accessible formats for example, different languages, video, easy read, Braille and so on.
- Document discussion in patient record and make an interim decision regarding use of the system.
- Multidisciplinary team (MDT) meeting should reach a clinical decision regarding the use of the VBPMS considering the risk of patient harm and, if relevant, the particular risk of re-traumatisation based on patient history. MDT meeting should also consider whether the patient is admitted informally or formally (subject to the Mental Health Act). The risk(s) and rationale for the decision should be documented in the patient record.
- The best interests meeting will involve patients, family, carers or advocates to discuss the clinical recommendation and rationale and to ensure all views have been considered. A final decision confirmed about whether the system is kept on or switched off will be made.
- Decision to keep VBPMS on or off should be documented in the patient record.
- The use of the VBPMS should be discussed weekly with the patient, family or carers as part of their MDT care review, or where there is a significant change in presentation. If a consenting patient subsequently objects, the provider should discuss this at the MDT meeting and follow the process from step 3.
- If the system is switched off, relevant policies and procedures should be followed.
10.5 Appendix E Training record and signature sheet
10.6 Appendix F Recording Oxevision incidents in SystmOne
Colleagues must record in SystmOne when Oxevision notifies them of a potential incident.
- Select the RDaSH intervention and de-escalation tab from the RRI node on the clinical tree.
- Left click on the icon on the view to launch the template.
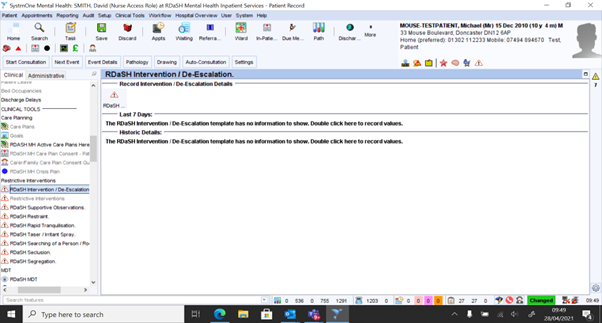
- Complete the date and time field at the top of the template to indicate when Oxevision made the notification.
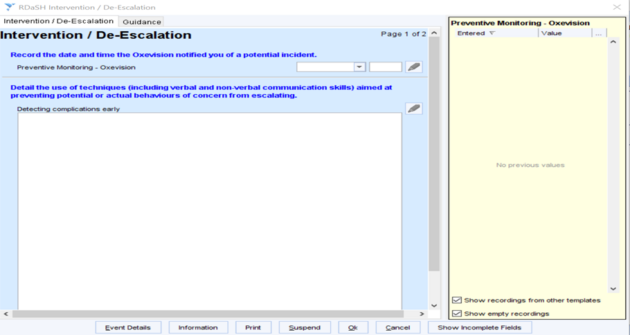
- Complete the remainder of the template as appropriate.
- Save the record.
Document control
- Version: 1.3.
- Unique reference number: 1071.
- Approved by: Clinical policies review and approvals group.
- Date approved: 28 November 2023.
- Name of originator or author: Head of information quality or information quality manager.
- Name of responsible individual: Executive director of nursing and AHP.
- Date issued: 22 April 2024.
- Review date: 31 December 2026.
- Target audience: All colleagues including bank and agency working across RDaSH mental health inpatient services.
Page last reviewed: April 22, 2024
Next review due: April 22, 2025