Contents
1 Introduction
Rotherham Doncaster and South Humber NHS Foundation Trust (RDaSH) is a diverse organisation providing both physical and mental health services. The trust recognises that admission, transfer and discharge from hospital should take place in a planned and structured way regardless of speciality. It should be equitable and patient centred, with patients, families and carers feeling well orientated and secure in their environment.
Because discharge planning often begins at admission, these processes regularly require a multidisciplinary and multi-agency approach. For this reason, good communication is seen as essential in ensuring there is a seamless process where all involved, the patient and where possible and appropriate, their family or carers, feel they have received high quality care, risks are managed and they are able to contribute fully to the discharge process.
The trust recognises the contribution that effective discharge or transfer care planning makes to high quality service provision, continuity of care and the recovery journey. Hospital discharge may not be the point of discharge from care, but a transfer in the location of delivery of care.
Guidance in relation to additional admission arrangements:
- Amber Lodge, all admissions are agreed through NHS England commissioning arrangements
- Emerald Lodge is a stand-alone unit. Patients should be admitted in a pre-planned and organised way with no out of hours admissions. All those being admitted should have an up-to-date risk and needs assessment reflecting appropriateness of the environment
- St Johns Hospice, patients will be triaged and assessed prior to admission and patient needs will be determined in line with policies and clinical judgement relating to patient need
- New Beginnings, admissions are elective and as such are organised in advance with the appropriate team
1.1 Children admitted to inpatient wards
Whilst it is accepted that patients under the age of 18 should not be admitted to an RDaSH inpatient ward as the trust is not commissioned to provide these services, there may be exceptional circumstances in cases for patients between the ages of 16 to 18 of urgent necessity and the absence of satisfactory immediate alternatives where in the short term, this may need to occur.
There should be no circumstance in which a patient under the age of 16 will be admitted to an RDaSH inpatient ward.
The legal framework governing the admission to hospital and treatment of children and young people under the age of 18 is complex, and those responsible for their care in hospital should be familiar with the relevant legislation as outlined within the Mental Health Act 1983, Mental Health Act Code of Practice 2015, Children Act 1989 and the Mental Capacity Act 2005. Information in regard to this can be found in the following policies:
- care and treatment of children under the age of 18 on adult acute mental health inpatient areas policy
- assessment and care of children and young people with mental health needs who are placed in an acute general hospital ward policy
2 Purpose
The purpose of this policy is to:
- provide a unified admission, transfer and discharge process identifying and outlining how the core components of effective practice are to be delivered across diverse services and geographical areas and to provide an overarching framework to support local standard operating procedures (SOPs) and, or Procedural documents
- ensure patients families and carers are directly involved with decisions and choices to be made about their care
- to ensure discharge is planned at the earliest opportunity and considered from admission onwards
- to support compliance with national and local guidance, ensuring all necessary health and social care needs are met
The policy addresses aspects of orientation, assessment and discharge planning which can result in a safe and effective patient stay.
2.1 Definition
Inpatient mental health and forensic LD services at RDaSH provide assessment, care and treatment for people whose presenting need cannot be safely managed in the community or setting they are currently residing at. Any admission to inpatient services should take into consideration the guiding principles of the MHA (1983) the Mental Capacity Act (MCA) and the least restrictive options available to support the person whilst balancing this against levels of complexity and risk to self or risk to others.
A person is defined as an inpatient either:
- when they are able to give valid consent to the admission (Informal status, mental health services)
- are formally admitted under the Mental Health Act (1983) (MHA) (detained status, always for forensic LD services)
- are admitted under a best interest decision under the Mental Capacity Act 2005 and ensure the assessment and decision is evidenced in line with trust MCA Mental Capacity Act 2005 policy
And they have arrived on the ward, have been clerked in and admitted onto the electronic patient record into an available bed by an admitting professional, so the admission or assessment process can commence.
Any person brought to our hospital-based place of safety (section 136 suite) under section 136 of the MHA (1983) for assessment are not deemed inpatients and therefore are outside the scope of this manual. Please see the section 136 of the mental health act 1983 policy for details.
All other Inpatient services which include New Beginnings drug and alcohol, St Johns Hospice, Magnolia (neuro-rehabilitation) Hazel and Hawthorne have their own process and criteria for Inpatient admission and colleagues should follow the SOPs contained within this manual.
3 Scope
This document will apply to all healthcare colleagues working in the trust’s in-patient areas, including managers, nurses, doctors and allied health professionals or whichever professional first makes contact with the patient and initiates assessment of their needs. This includes when assessment begins prior to the actual admission to the hospital.
The trust provides a diverse range of in-patient services as outlined below:
- St John’s hospice
- neuro rehabilitation services
- intermediate care services
- forensic services
- all age mental health services
- drug and alcohol rehabilitation (New Beginnings)
4 Procedure or implementation
- Patient flow procedure
- Admission to adult and older persons mental health service inpatient wards procedure
- Safe discharge or transfer of patients from adult and older persons mental health service inpatient wards procedure
- Discharge or transfer St John’s hospice inpatient service procedure
- Discharge or transfer of in-patients from Hawthorn and Hazel wards procedure
- Children and young people’s mental health service (CAMHS) out of hours service procedure
- Safe transportation of patients and staff (adult and older person’s mental health and learning disability)
5 Training implications
There are no specific training needs in relation to this policy, but the following colleagues will need to be familiar with its contents and any other individual or group with a responsibility for implementing the contents of this policy.
As a trust policy, all colleagues need to be aware of the key points that the policy covers. Colleagues can be made aware through:
- one to one meetings or supervision
- continuous professional development sessions
- posters
- practice development days
- team meetings
- local induction
6 Equality impact assessment screening
Link to manual equality impact assessment: Admission transfer and discharge manual policy EIA.
6.1 Privacy, dignity and respect
The NHS Constitution states that all patients should feel that their privacy and dignity are respected while they are in hospital. High Quality Care for All (2008), Lord Darzi’s review of the NHS, identifies the need to organise care around the individual, ‘not just clinically but in terms of dignity and respect’.
As a consequence the trust is required to articulate its intent to deliver care with privacy and dignity that treats all service users with respect. Therefore, all procedural documents will be considered, if relevant, to reflect the requirement to treat everyone with privacy, dignity and respect, (when appropriate this should also include how same sex accommodation is provided).
6.1.1 How this will be met
All employees, contractors and partner organisations working on behalf of the trust must follow the requirements of this policy and other related policies, particularly those relating to information governance. All health employees must also meet their own professional codes of conduct in relation to confidentiality.
6.2 Mental Capacity Act
Central to any aspect of care delivered to adults and young people aged 16 years or over will be the consideration of the individuals capacity to participate in the decision making process. Consequently, no intervention should be carried out without either the individual’s informed consent, or the powers included in a legal framework, or by order of the court.
Therefore, the trust is required to make sure that all staff working with individuals who use our service are familiar with the provisions within the Mental Capacity Act (2005). For this reason all procedural documents will be considered, if relevant to reflect the provisions of the Mental Capacity Act (2005) to ensure that the rights of individual are protected and they are supported to make their own decisions where possible and that any decisions made on their behalf when they lack capacity are made in their best interests and least restrictive of their rights and freedoms.
6.2.1 How this will be met
All individuals involved in the implementation of this policy should do so in accordance with the guiding principles of the Mental Capacity Act (2005).
7 Links to any other associated documents
- Infection prevention and control manual
- MCA Mental Capacity Act 2005 policy
- Section 135 mental health act 1983 policy
- MCA deprivation of liberty (DoL) policy
- Advance statements and advance decisions to refuse treatment policy
- Patient identification policy
- Interpreters policy (provision, access and use of, for patients, service users and carers)
- Safe and secure handling of medicines manual
- Resuscitation manual
- Care programme approach (CPA) policy
- Clinical risk assessment and management policy
- Section 136 of the mental health act 1983 policy
- Care and treatment of children under the age of 18 on adult acute mental health inpatient areas policy
- Assessment and care of children and young people with mental health needs who are placed in an acute general hospital ward policy
8 References
- Home to the Unknown, Getting hospital discharge right (2019) British Red Cross.
- NICE Guidance Medicines optimisation: the safe and effective use of medicines to enable the best possible outcomes (NG5).
- NICE Guidance (2015): Transition between inpatient hospital settings and community or care home settings for adults with social care needs (NG27).
9 Appendices
11.1 Appendix A Responsibilities, accountabilities and duties
11.1.1 Board of directors
Board of directors is responsible for ensuring that the organisation consistently follows the principles of good governance applicable to NHS organisations. This includes the development of systems and processes for admission, transfer, and discharge of patients.
11.1.2 Chief executive
The board of directors delegates to the chief executive the overall responsibility for effective risk management in the trust, meeting all statutory requirements and adhering to guidance issued.
11.1.3 Care group directors and care group nurse directors
Care group directors and care group nurse directors are the designated leads with responsibility for the implementation of this policy and national and local guidance.
- Disseminating, implementing and monitoring this policy and the local standard operating procedure within their services.
- Facilitating collaborative working between in-patient and community services in order to provide high quality patient care.
- Monitoring any trends, themes or concerns raised during the admission process and taking action as appropriate to reduce or prevent risks and to improve the patient experience.
11.1.4 Lead clinician
Depending on the inpatient area the responsible person could be a doctor, a nurse or an allied health professional. It is their responsibility to ensure:
- they are involved in the admission, discharge, or transfer of the patient in consultation with carer(s) and the multi-disciplinary team
- that admissions, transfer and discharges are carried out in line with the relevant service’s standard operating procedure or local procedural documents
- that all required information is shared with appropriate healthcare professionals, for example, general practitioner (GP) as detailed in the local service SOP. As a minimum the following information must be shared:
- medication
- patient discharge against medical advice
- a copy of the patient’s discharge or transfer letter
- the local security management specialist (LSMS) is informed at the earliest opportunity of the admission of a formal or informal active prisoner
11.1.5 Ward managers
Ward managers or modern matrons or service managers are responsible for:
- informing the local security management specialist at the earliest opportunity of the admission of a formal or informal active prisoner
- informing all colleagues through local induction of the trust’s admission, discharge and transfer manual and relevant local procedures or standard operating procedures
- recording and monitoring standards to ensure compliance with trust policy for admission, transfer and discharge
- monitoring, recording, and reporting delays in transfer of care as per agreed trust process
- ensuring good communication between inpatient and community agencies
- ensuring national and local guidance is adhered to
11.1.6 Local security management specialist (LSMS)
Once notification by the lead clinician, ward manager or service manager or modern matron has been received the LSMS must attend that specific ward and liaise with the prison officers to carry out a joint risk assessment based on the prisoner’s history obtained from the police to define responsibilities of staff during the patients’ care and continued detention. This will be reviewed at regular intervals.
11.1.7 All RDaSH colleagues
Colleagues who come into contact with patients are seen by doctors, nurses, allied health professionals, pharmacists, psychologists, bank staff and agency workers, students and volunteers. All are expected to ensure that each person coming into their care and their carers are treated with dignity and respect.
Members of the multidisciplinary team including external agencies, the patient and their family or carers should be aware of and involved in the admission, transfer, and discharge process in a timely manner.
All clinical and non-clinical colleagues involved in the admission, discharge or transfer of a patient to and from trust services, should ensure local and national guidance in relation to this are adhered to.
11.1.8 Care coordinator (mental health)
In line with the RDaSH care programme approach (CPA) policy or equivalent, the care coordinator should stay involved throughout admission and support discharge planning. Where the care coordinator is not available, a deputy should be in place.
11.2 Appendix B Monitoring arrangements
11.2.1 Admission or discharge experience.
- How: Review of complaints.
- Who by: Patient Safety and Investigations team.
- Reported to: Care groups.
- Frequency: Bi-monthly.
11.2.2 Admission or discharge experience.
- How: Your opinion counts forms.
- Who by: Service managers.
- Reported to: Care group quality meetings.
- Frequency: Monthly.
11.2.3 Staff compliance with policy.
- How: Monitoring of admission documentation via management or clinical supervision.
- Who by: Ward managers or service managers.
- Reported to: Service managers escalated if required to care group nurse directors.
- Frequency: Minimum bi-monthly.
11.3 Appendix C Informal admission leaflet
Please click on the following link to access the most up to date version of the admission as an informal patient to a mental health unit leaflet.
11.4 Appendix D Nursing admission checklist
11.5 Appendix E Named nurse leaflet
Please click on the following link to access the most up to date version of the your named nurse leaflet.
11.6 Appendix F Evidence of legal authority to admit an informal patient checklist
11.7 Appendix G Capability framework, needs to be uploaded as word document
11.8 Appendix H Key contact details
11.8.1 Rotherham
Rotherham Hospital
Moorgate Road
Rotherham
S60 2UD
- Telephone: 01709 820000
11.8.2 Doncaster
Doncaster Royal Infirmary
Armthorpe Road
Doncaster
DN2 5LT
- Telephone: 01302 366666
11.8.3 North Lincolnshire
Scunthorpe General Hospital
Cliff Gardens
Scunthorpe
DN15 7BH
- Telephone: 01724 282282
11.8.4 Useful telephone numbers
CAMHS Manager on call 01302 796000.
| Locality | Adult crisis team | Emergency social services |
|---|---|---|
| Rotherham | 08006 529571 | Rothercare: 01709 364689 |
| Doncaster | 08008 048999 | ESST (Emergency Social Services team): 01302 796000 |
| North Lincolnshire | 08000 150211 | Duty Social Worker team: 01724 296555 |
11.9 Appendix I Recording of referrals and activity on SystmOne
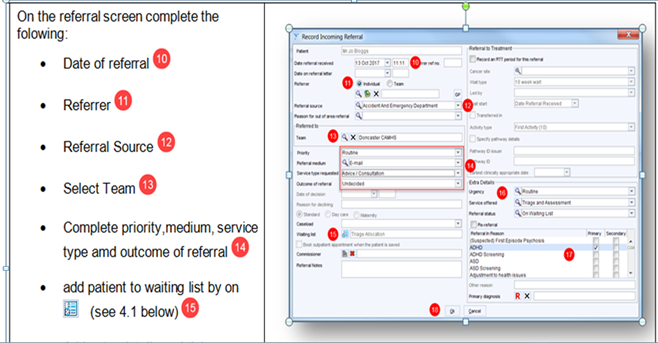
On the referral screen complete the following:
- date of referral (10)
- referrer (11)
- referral source (12)
- select team (13)
- complete priority, medium, service type and outcome of referral (14)
- add patient to waiting list on (see 4.1 below) (15)
13, team equals locality CAMHS Crisis team the child presents at, for example, ‘Scunthorpe CYP Crisis team’, ‘Doncaster CYP Crisis team’ or ‘Rotherham CYP Crisis team’ by A and E or emergency care centre locality.
14, priority equals very urgent for out of hours (or emergency if immediate threat to life).
Service type requested equals advice and consultation.
Complete outcome of referral to ‘accepted’ if possible, if not task the relevant locality team to accept.
11.10 Appendix J Adult and older persons mental health bed capacity
11.10.1 Doncaster bed capacity
| Site | Bed number | Contact number or MiCollab |
|---|---|---|
| Tickhill Road Hospital | 6 | 01302 798174 or 01302 798175 (11176) |
| Site | Bed number | Contact number or MiCollab |
|---|---|---|
| Tickhill Road Hospital | 20 | 01302 798060 or 01302 798185 (11061) |
| Site | Bed number | Contact number or MiCollab |
|---|---|---|
| Tickhill Road Hospital | 20 | 01302 798170 or 01302 798171 (11170) |
| Site | Bed number | Contact number or MiCollab |
|---|---|---|
| Tickhill Road Hospital | 20 | 01302 796087 (14086) |
11.10.2 Rotherham best capacity
| Site | Bed number | Contact number or MiCollab |
|---|---|---|
| Swallownest Court | 5 | 01709 447443 (15521) |
| Site | Bed number | Contact number or MiCollab |
|---|---|---|
| Swallownest Court | 18 | 01709 447442 (15531) |
| Site | Bed number | Contact number or MiCollab |
|---|---|---|
| Swallownest Court | 18 | 01709 447441 (15529) |
| Site | Bed number | Contact number or MiCollab |
|---|---|---|
| The Woodlands | 15 | 01709 447003 (15601) |
| Site | Bed number | Contact number or MiCollab |
|---|---|---|
| The Woodlands | 15 | 01709 447002 (15611) |
11.10.3 North Lincolnshire bed capacity
| Site | Bed number | Contact number or MiCollab |
|---|---|---|
| Great Oaks | 17 | 01724 382077 (16011) |
| Site | Bed number | Contact number or MiCollab |
|---|---|---|
| Great Oaks | 13 | 01724 382054 (16166) |
11.11 Appendix K Ward transfer checklist
11.12 Appendix L Adult mental health and older persons process for arranging and authorising out of area placements
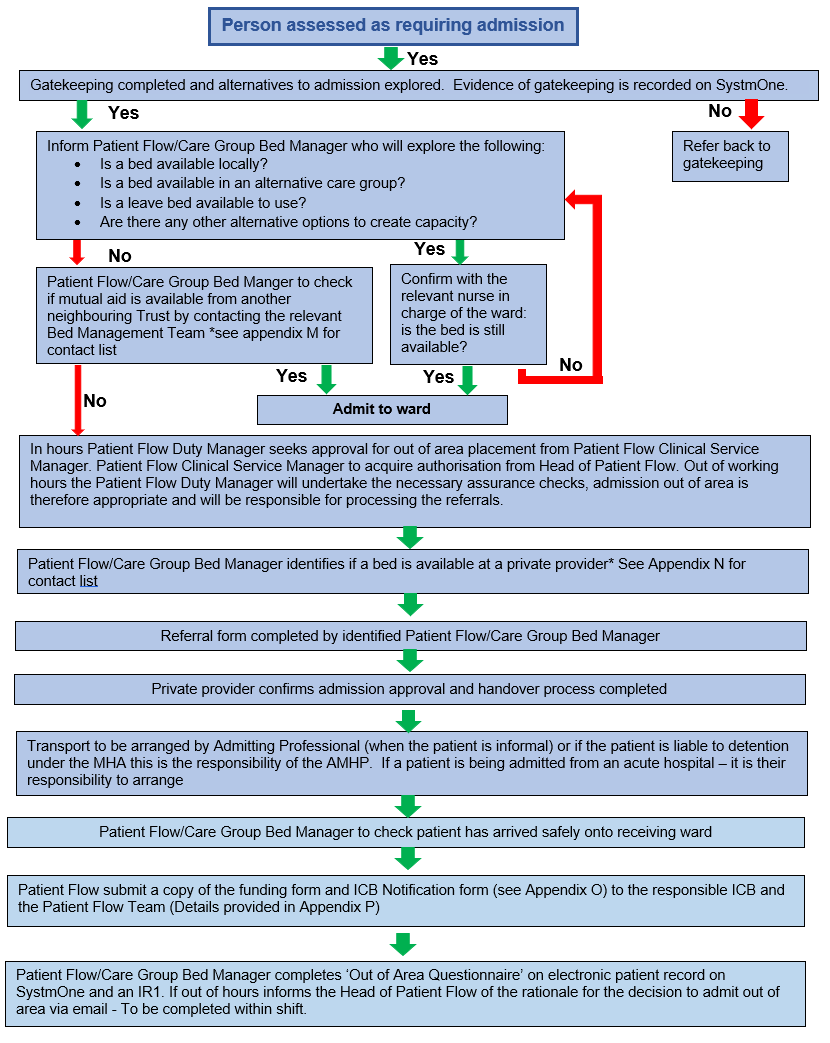
- Person assessed as requiring admission.
- Gatekeeping completed and alternatives to admission explored. Evidence of gatekeeping is recorded on SystmOne.
- no, refer back to gatekeeping. End process
- Yes, inform patient flow or care group bed manager who will explore the following:
- is a bed available locally?
- is a bed available in an alternative care group?
- is a leave bed available to use?
- are there any other alternative options to create capacity?
- yes, confirm with the relevant nurse in charge of the ward : is the bed is still available?
- yes, admit to ward. End process
- yes, confirm with the relevant nurse in charge of the ward : is the bed is still available?
- No, patient flow or care group bed manager to check if mutual aid is available from another neighbouring trust by contacting the relevant Bed Management team, see appendix M for contact list
- yes, admit to ward. End process
- No, in hours patient flow duty manager seeks approval for out of area placement from patient flow clinical service manager. Patient flow clinical service manager to acquire authorisation from head of patient flow. Out of working hours the patient flow duty manager will undertake the necessary assurance checks, admission out of area is therefore appropriate and will be responsible for processing the referrals.
- Patient flow or care group bed manager identifies if a bed is available at a private provider, see appendix N for contact list.
- Referral form completed by identified patient flow or care group bed manager.
- Private provider confirms admission approval and handover process completed.
- Transport to be arranged by admitting professional (when the patient is informal) or if the patient is liable to detention under the MHA this is the responsibility of the AMHP. If a patient is being admitted from an acute hospital, it is their responsibility to arrange.
- Patient flow or care group bed manager to check patient has arrived safely onto receiving ward.
- Patient flow submit a copy of the funding form and ICB notification form (see appendix O) to the responsible ICB and the patient flow team (details provided in appendix P).
- Patient flow or care group bed manager completes ‘out of area questionnaire’ on electronic patient record on SystmOne and an IR1. If out of hours informs the head of patient flow of the rationale for the decision to admit out of area via email, to be completed within shift.
11.13 Appendix M Mutual aid contact details
11.13.1 Mutual aid contact details in hours
11.13.1.1 Barnsley
Patient Flow team:
- No central contact number.
- Email: swypftpatientflow@swyt.nhs.uk
11.13.1.2 Sheffield
Patient Flow team:
- Telephone: 0114 271 6310
- Email: flowcoordinatorsteam@shsc.nhs.uk
11.13.1.3 Navigo
No dedicated Patient Flow team. Ask for duty manager:
- Telephone: 01472 874111
11.13.2 Mutual aid contact details out of hours (5pm to 9am)
11.13.2.1 Barnsley
Intensive Home-Based Treatment team:
- Telephone: 01226 644 150
11.13.2.2 Calderdale
Intensive Home-Based Treatment team:
- Telephone: 01422 222 908
11.13.2.3 Kirklees
Intensive Home-Based Treatment team:
- Telephone: 01484 343 161
11.13.2.4 Navigo
On call manager:
- Telephone: 01472 874111
11.13.2.5 Sheffield
Patient Flow team:
11.13.2.6 Wakefield
Intensive Home-Based Treatment team:
- Telephone: 01924 316 263
11.14 Appendix N Private providers contact details
11.14.1 Mutual aid contact details in hours
11.14.1.1 Cygnet
- Telephone: 0808 164 4450
- Email: chcl.referrals@nhs.net
11.14.1.2 Elysium
- Telephone: 0800 218 2398
- Email: referrals@elysiumhealthcare.co.uk
11.14.1.3 Priory
- Telephone: 0800 0901 356
- Email: prioryenquiries@nhs.net
11.14.1.4 St Andrew’s
- Telephone: 01604 616 000
- Email: Different email addresses for different hospitals
11.15 Appendix O ICB notification and funding form submission details
11.15.1 Trust notification contact details
11.15.1.1 Corporate
Patient Flow team, patient flow managers:
11.15.2 ICB notification contact details
11.15.2.1 Doncaster
11.15.2.2 Rotherham
11.15.2.3 North Lincolnshire
11.16 Appendix P Out of area patient ICB notification form
11.17 Appendix Q Adult mental health and older persons out of area (OOA) placement monitoring process
The adult mental health and older persons out of area (OOA) placement monitoring process flow chart provides oversight of the monitoring requirements for all patients placed in either an inappropriate or appropriate placement external to the trust.
An inappropriate OOA placement occurs when clinical demand for an inpatient bed exceeds the trust bed stock availability and therefore patients need to be accommodated in an alternative NHS or private sector setting.
An OOA placement may on occasion be defined as appropriate if a patient requires their needs to be met in a particular environment due to risk, for example, a male only PICU or if a patient is close to discharge and elects to remain OOA for continuity of care.
Specialist placements refer to care provision outside of the trust services, for example, secure and locked rehab and are therefore outside of the scope of this flow chart.
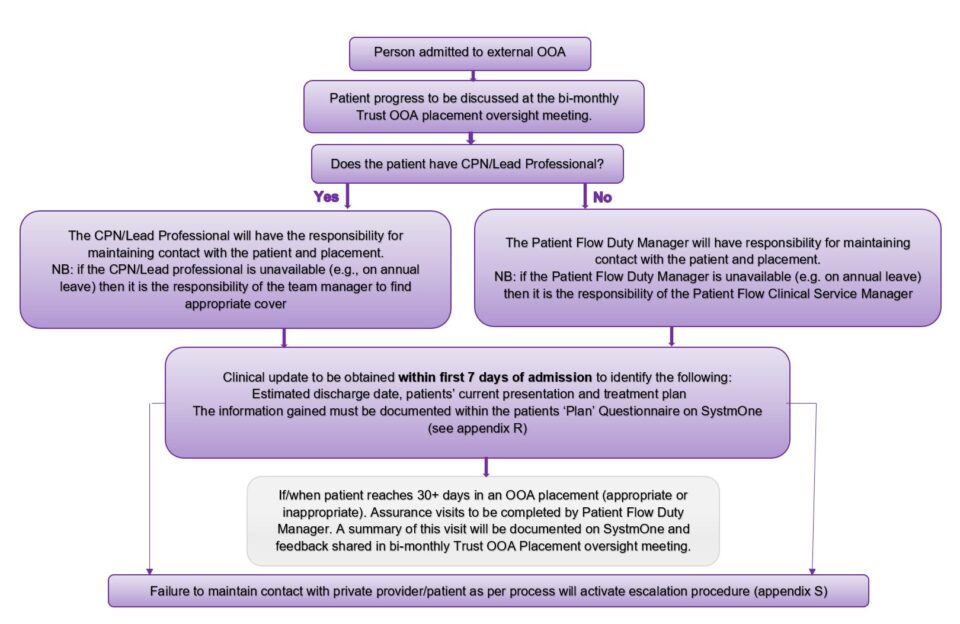
- Person admitted to external OOA bed.
- Patient progress to be discussed at the bi-monthly trust OOA placement oversight meeting.
- Does the patient have CPN or lead professional?
- yes, the CPN or lead professional will have the responsibility for maintaining contact with the patient and placement. Note, if the CPN or lead professional is unavailable (for example, on annual leave) then it is the responsibility of the team manager to find appropriate cover
- no, the patient flow duty manager will have responsibility for maintaining contact with the patient and placement. Note, if the patient flow duty manager is unavailable (for example, on annual leave) then it is the responsibility of the patient flow clinical service manager
- Clinical update to be obtained within first 7 days of admission to identify the following:
- estimated discharge date, patients’ current presentation and treatment plan
- the information gained must be documented within the patients ‘plan’ questionnaire on SystmOne (see appendix R)
- if or when patient reaches 30 or more days in an OOA placement (appropriate or inappropriate). Assurance visit to be completed by patient flow duty manager. A summary of this visit will be documented on SystmOne and feedback shared in bi-monthly trust OOA placement oversight meeting
- Failure to maintain contact with private provider or patient as per process will activate escalation procedure (appendix S).
11.18 Appendix R How to document clinical updates
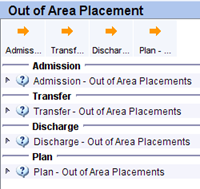
Data capture for out of area placement (OAP) is completed using 4 questionnaires within SystmOne, admission, transfer, discharge and plan.
11.18.1 Adult units
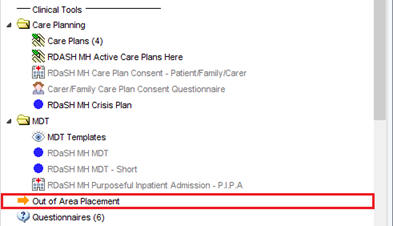
The questionnaires can be located on the Clinical Tree, on a node called “out of area placement”. All of the questionnaires are in one place. This node is located just under care planning or MDT on each unit.
Once you click on the node, there are four buttons:
- admission
- transfer
- discharge
- plan
Upon any of the first three being completed, a task will be sent automatically to the Patient Flow team for information. All of the fields in these three questionnaires are now mandatory to aid data quality.
The fourth questionnaire (plan) is used to record discussions with out of area providers, or the patient, and considerations of repatriation.
Once a questionnaire has been completed, they’ll go under the corresponding section. To view these, either right click and select “View Questionnaire” or use the little triangle at the left side:
Out of area placement tutorial (staff access only) (opens in new window).
11.19 Appendix S Escalation procedure
- Appropriate professional to obtain initial update within 7 days of
admission. - Failure to obtain update within 7 days of admission since last contact will be escalated to the team manager by the Patient Flow team.
- Failure to obtain update within 10 days of admission or since last
contact will be escalated to the service manager by the Patient Flow
team. - Failure to obtain update within 14 days of admission or since last
contact will be escalated to the group director by the Patient flow
team. - The Patient Flow team to complete IR1 form if update is not received within 28 days.
11.20 Appendix T Ward closure procedure adult and older adults mental health
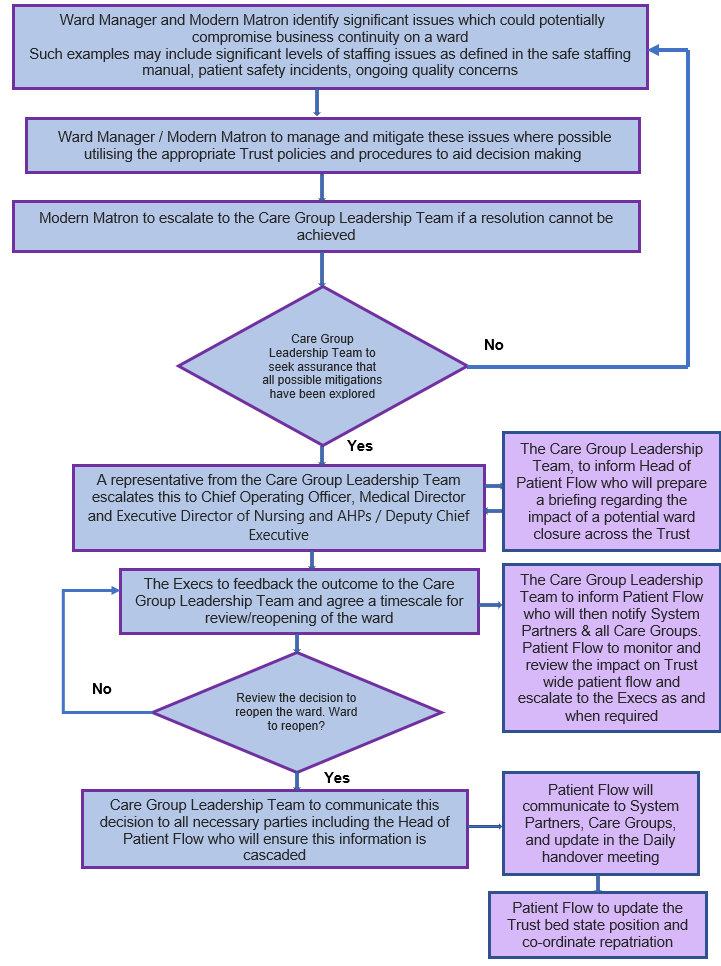
- Ward manager and modern matron identify significant issues which could potentially compromise business continuity on a ward
Such examples may include significant levels of staffing issues as defined in the safe staffing manual, patient safety incidents, ongoing quality concerns. - Ward manager or modern matron to manage and mitigate these issues where possible utilising the appropriate Trust policies and procedures to aid decision making.
- Modern matron to escalate to the Care Group Leadership team if a resolution cannot be achieved.
- Care Group Leadership team to seek assurance that all possible mitigations have been explored.
- no, go to step 1.
- Yes, A representative from the Care Group Leadership team escalates this to chief operating officer, medical director and executive director of nursing and AHPs or deputy chief executive:
- the Care Group Leadership team, to inform head of patient flow who will prepare a briefing regarding the impact of a potential ward closure across the trust
- The executives to feedback the outcome to the Care Group Leadership team and agree a timescale for review or reopening of the ward:
- the Care Group Leadership team to inform patient flow who will then notify system partners and all care groups. Patient flow to monitor and review the impact on trust wide patient flow and escalate to the executives as and when required
- Review the decision to reopen the ward. Ward to reopen?
- no, go to step 8.
- Yes, care Group Leadership team to communicate this decision to all necessary parties including the head of patient flow who will ensure this information is cascaded.
- Patient flow will communicate to system partners, care groups, and update in the daily handover meeting.
- Patient flow to update the trust bed state position and co-ordinate repatriation.
11.21 Appendix U Rockwood frailty scale
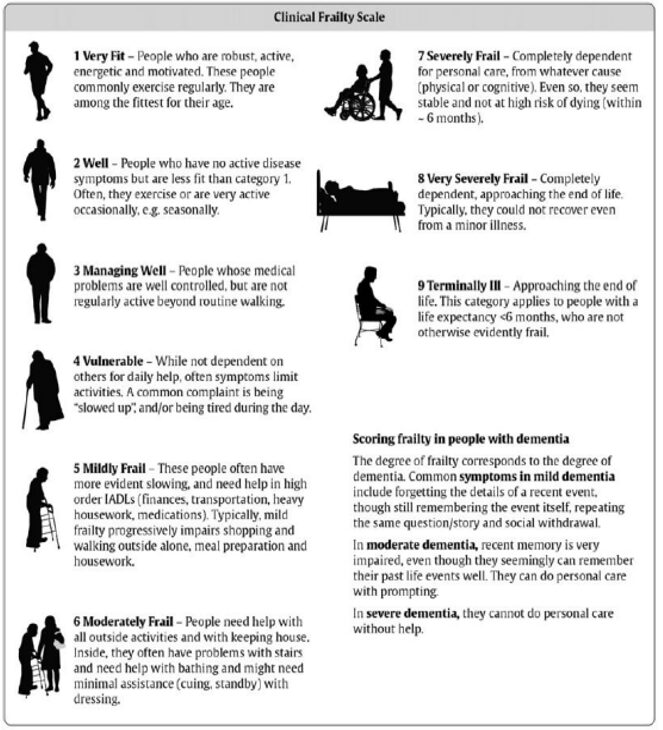
- Very fit, people who are robust, active, energetic and motivated. These people commonly exercise regularly. They are among the fittest for their age.
- Well, people who have no active disease symptoms but are less fit than category 1. Often, they exercise or are very active occasionally, for example, seasonally.
- Managing well, people whose medical problems are well controlled, but are not regularly active beyond routine walking.
- Vulnerable, while not dependent on others for daily help, often symptoms limit activities. A common complaint is being “slowed up”, and, or being tired during the day.
- Mildly frail, these people often have more evident slowing, and need help in high order IADLs (finances, transportation, heavy housework, medications). Typically, mild frailty progressively impairs shopping and walking outside alone, meal preparation and housework.
- Moderately frail, people need help with all outside activities and with keeping house. Inside, they often have problems with stairs and need help with bathing and might need minimal assistance (cuing, standby) with dressing.
- Severely frail, completely dependent for personal care, from whatever cause (physical or cognitive). Even so, they seem stable and not at high risk of dying (within 6 months).
- Very severely frail, completely dependent, approaching the end of life. Typically, they could not recover even from a minor illness.
- Terminally iII, approaching the end of life. This category applies to people with a life expectancy less than 6 months, who are not otherwise evidently frail.
11.21.1 Scoring frailty in people with dementia
The degree of frailty corresponds to the degree of dementia. Common symptoms in mild dementia include forgetting the details of a recent event, though still remembering the event itself, repeating the same question or story and social withdrawal.
In moderate dementia, recent memory is very impaired, even though they seemingly can remember their past life events well. They can do personal care with prompting.
In severe dementia, they cannot do personal care without help.
Please note as advised by the NHS specialised clinical frailty network the clinical frailty scale has not been widely validated in younger populations (below 65 years of age), or in those with learning disability. It may not perform as well in people with stable long term disability such as cerebral palsy, whose outcomes might be very different compared to older people with progressive disability. It is therefore to be used to support decision making in the context of this procedure as in the round it will be part of a wider and more holistic assessment of need. Further information can be found at the NHS specialised clinical frailty network site (opens in new window).
11.22 Appendix V Taxi booking form
11.23 Appendix W Private ambulance secure transport booking form
11.24 Appendix X 72 hour follow up technical guide
Document control
- Version: 2.2.
- Unique reference number: 1006.
- Approved by: Clinical policies review and approval group.
- Date approved: 11 March 2024.
- Name of originator or author: Head of patient flow.
- Name of responsible committee or individual: Chief operating officer.
- Date issued: 11 March 2024 (minor amendment to appendix A and B).
- Review date: 30 September 2024.
- Target audience: Trust wide.
Page last reviewed: April 23, 2024
Next review due: April 23, 2025