Contents
1 Introduction
Rotherham, Doncaster and South Humber NHS Foundation Trust (RDaSH) is a diverse organisation providing both physical and mental health services. The trust recognises that admission, transfer and discharge from hospital should take place in a planned and structured way regardless of speciality. It should be equitable, and patient centred, with patients, families and carers feeling well orientated and secure in their environment.
Because discharge planning often begins at admission, these processes regularly require a multidisciplinary and multi-agency approach. For this reason, good communication is seen as essential in ensuring there is a seamless process where all involved, the patient and where possible and appropriate, their family or carers, feel they have received high quality care, risks are managed, and they are able to contribute fully to the discharge process.
The trust recognises the contribution that effective discharge or transfer care planning makes to high quality service provision, continuity of care and the recovery journey. Hospital discharge may not be the point of discharge from care but a transfer in the location of delivery of care.
Guidance in relation to additional admission arrangements:
- Amber Lodge, all admissions are agreed through NHS England commissioning arrangements
- Emerald Lodge is a stand-alone unit. Patients should be admitted in a pre-planned and organised way with no out of hours admissions. All those being admitted should have an up-to-date risk and needs assessment reflecting appropriateness of the environment
- St Johns Hospice, patients will be triaged and assessed prior to admission and patient needs will be determined in line with policies and clinical judgement relating to patient need
- New Beginnings, admissions are elective and as such are organised in advance with the appropriate team
1.1 Children admitted to inpatient wards
Whilst it is accepted that patients under the age of 18 should not be admitted to a Rotherham, Doncaster and South Humber NHS Foundation Trust (RDaSH) inpatient ward as the trust is not commissioned to provide these services, there may be exceptional circumstances in cases for patients between the ages of 16 to 18 of urgent necessity and the absence of satisfactory immediate alternatives where in the short term, this may need to occur.
There should be no circumstance in which a patient under the age of 16 will be admitted to an RDaSH inpatient ward.
The legal framework governing the admission to hospital and treatment of children and young people under the age of 18 is complex, and those responsible for their care in hospital should be familiar with the relevant legislation as outlined within the Mental Health Act (1983), Mental Health Act Code of Practice (2015), Children Act (1989) and the Mental Capacity Act (2005). Information in regard to this can be found in the following policies:
- care and treatment of children under the age of 18 on adult acute mental health inpatient areas policy
- assessment and care of children and young people with mental health needs who are placed in an acute general hospital ward policy
1.2 Pregnant patients admitted to inpatient wards
Cases concerning interventions with pregnant women experiencing mental disorder, illness or impairment are complex, medically, ethically and legally. Mental disorders are no less common in pregnancy than at other times in a woman’s life. Effective care can best be delivered when there is good communication, information sharing and joint working between professionals involved in caring for childbearing women. Care planning and multi-agency working is important for all mental health patients, however for pregnant women it is essential. The needs of both the mother and the unborn child need to be considered.
The trust Safeguarding team should be informed of all pregnant patients that are admitted to the ward regardless of whether there are identified safeguarding concerns.
- Assess risk of pregnancy on admission. Consider history, contraception, age, and gender.
- If a pregnancy is suspected or known contact the trust safeguarding team for advice and guidance and complete trust incident reporting system.
- Consider gestation of pregnancy, patient wishes in continuation of pregnancy and other services that can support with decision-making (consider mental capacity around decision-making).
- Considering gestation of pregnancy and wishes of patient pregnancy, delivery and postnatal care, liaise with midwifery, notify Health visiting team and refer to local authority children social care.
- The inpatient ward is responsible for coordinating initial professionals meeting.
- Multi-agency response to assess any risk of harm to the patient, unborn child and others.
- Ensure clear planning and documentation around proposed interventions.
2 Purpose
The purpose of this policy is to:
- provide a unified admission, transfer and discharge process identifying and outlining how the core components of effective practice are to be delivered across diverse services and geographical areas and to provide an overarching framework to support local standard operating procedures (SOPs) and, or procedural documents
- ensure patients families and carers are directly involved with decisions and choices to be made about their care
- to ensure discharge is planned at the earliest opportunity and considered from admission onwards
- to support compliance with national and local guidance, ensuring all necessary health and social care needs are met
The policy addresses aspects of orientation, assessment and discharge planning which can result in a safe and effective patient stay.
2.1 Definition
Inpatient mental health and forensic learning disability services at RDaSH provide assessment, care and treatment for people whose presenting need cannot be safely managed in the community or setting they are currently residing at. Any admission to inpatient services should take into consideration the guiding principles of the Mental Health Act (1983) the Mental Capacity Act (MCA) and the least restrictive options available to support the person whilst balancing this against levels of complexity and risk to self or risk to others.
A person is defined as an inpatient either:
- when they are able to give valid consent to the admission (Informal status, mental health services)
- are formally admitted under the Mental Health Act (1983) (MHA) (detained status, always for forensic learning disability services)
- are admitted under a best interest decision under the Mental Capacity Act (2005) and ensure the assessment and decision is evidenced in line with trust Mental Capacity Act (2005) policy
And they have arrived at the ward, have been clerked in and admitted onto the electronic patient record into an available bed by an admitting professional, so the admission or assessment process can commence.
Any person brought to our hospital-based place of safety (section 136 suite) under section 136 of the Mental Health Act (1983) for assessment are not deemed inpatients and therefore are outside the scope of this manual. Please see the section 136 of the Mental Health Act (1983) policy for details.
All other Inpatient services which include New Beginnings drug and alcohol, St Johns Hospice, Magnolia (neurorehabilitation) Hazel and Hawthorne have their own process and criteria for Inpatient admission and colleagues should follow the procedures contained within this manual.
3 Scope
This document will apply to all healthcare colleagues working in the trust’s in-patient areas, including managers, nurses, doctors and allied health professionals or whichever professional first makes contact with the patient and initiates assessment of their needs. This includes when assessment begins prior to the actual admission to the hospital.
The trust provides a diverse range of in-patient services as outlined below:
- St John’s Hospice
- neuro rehabilitation services
- intermediate care services
- forensic services
- all age mental health services
- drug and alcohol rehabilitation (New Beginnings)
4 Procedures
4.1 Patient flow procedure
4.1.1 Aim
An inpatient admission to hospital may be an essential component to a person’s treatment and recovery to safely facilitate their care. The trust recognises that admission to hospital can be a stressful experience for the person, their family, friends and carers. Every effort is therefore made to ensure that the person’s admission is timely, purposeful, supportive to their needs, aimed towards their recovery, with privacy and dignity in mind and for no longer than clinically necessary.
Bed capacity both within the trust, and nationwide, is in high demand, so the management of resources must be effective and adopt a consistent approach with clear understanding of the roles and responsibilities of all involved.
The aim of this procedure is to provide clinical colleagues with a clear framework for the optimal use and safe and effective management of the trust’s beds within the adult and older person’s mental health inpatient services, both during times of “business as usual” and periods of high demand within a care group or trust and country wide. It also describes the operation, roles and responsibilities of the Rotherham, Doncaster, and South Humber (RDaSH) NHS Foundation Trust’s Patient Flow team.
4.1.2 Scope
This procedure applies to adult and older person’s mental health inpatient services within the trust. The following services have their own procedures and are excluded from the scope of this procedure:
- physical health wards
- St John’s hospice
- neuro rehabilitation services
- intermediate care services
- forensic services
- mental health rehabilitation services
- drug and alcohol rehabilitation (New Beginnings)
4.1.3 Mental health and older person’s bed capacity
The trust has three adult mental health in-patient sites comprising psychiatric intensive care and acute services, with a current total of 104 beds and a further 63 older person’s mental health beds across the Rotherham, Doncaster and North Lincolnshire care groups.
The current configuration of adult and older person’s mental health beds can be found in appendix J adult and older person’s mental health bed capacity.
4.1.4 The role and function of the Patient Flow team
The role of the Patient Flow team is to work with Clinical teams and operational managers to make the most effective and efficient use of in-patient resources in agreed inpatient pathways.
The Patient Flow team will have bed management responsibility for all adult and older person’s mental health inpatient pathways in the trust in collaboration with Clinical teams, operational managers and on-call colleagues.
The Patient Flow team operates a 7-day service with identified bed management cover for all adult and older person’s in-patient wards in scope across the whole 24-hour period.
The Patient Flow team currently consists of:
- 1 head of patient flow
- 1 patient flow clinical service manager
- 6 patient flow duty managers
- 1 patient flow officer
- 6 patient flow co-ordinators
- 1 patient flow administrator
The head of patient flow will have overall management and responsibility for patient flow in the trust to ensure that the highest standards of patient flow are provided to help solve immediate operational problems. The head of patient flow will work closely and proactively with the care groups to ensure a central and coordinated approach to patient flow.
The patient flow clinical service manager and patient flow duty manager will be active and core to resolving any issues that arise relating to patient flow, which can include, though not limited to sourcing a bed (and issues related to this), difficulties with patients who are clinically ready for discharge (CRFD) but delayed, approving any referrals for trust out of area (OOA) placements and maintaining governance and oversight of those patients sent out of area both internal and external to the trust.
The primary responsibilities of the Patient Flow team are to:
- identify an appropriate bed when a patient requires admission to hospital
- coordinate transfers between the adult and older person’s mental health wards
- arrange all internal and external trust repatriations to the adult and older person’s mental health beds
- monitor all patient admissions to trust beds within scope and liaising with other trusts, ensure any non-trust patients are returned to their locality as soon as possible
- liaise with the Infection Prevention and Control team for support in managing patient placements or transfers for patients with infections
- assist and predict flow through the in-patient pathway and escalate any concerns to the clinical teams and operational managers as and when necessary
- maintain proactive oversight of length of patient stay and support clinical teams to identify any potential barriers to discharge upon admission and escalate any concerns regarding those patients clinically ready for discharge but delayed resolving any issues as swiftly as possible
- produce patient flow or bed management related reports, sharing these with Clinical teams, operational managers and senior leaders as and when required
- ensure good governance and oversight of patients sent out of area both internal and external to the trust and ensure these patients are repatriated as soon as practically possible. This does not replace the clinical responsibility when a patient has a care co-ordinator or lead professional assigned
It is not appropriate for wards to arrange transfers or repatriations between themselves as colleagues may be unaware of all associated clinical issues and other potential transfers or admissions that may take priority.
On occasion, patients require ward transfer for reasons not related to locality, for example, clinical reasons, safeguarding reasons. The Patient Flow team will facilitate and authorise all transfers of this kind, taking into consideration clinical presentation, safeguarding advice, interventions used and the needs of potential receiving wards.
4.1.5 Principles of good patient flow management
There are some key principles for good bed management which are outlined below:
- where possible, all patients should be admitted to their home locality
- a patient should be admitted to a ward that provides the least restrictive level of care necessary
- discharge planning should commence at the point of admission
- a full review of patient needs and care (including activities of daily living (AODL), and infection prevention and control) should be taken into consideration when planning admission, transfer or discharge
- admission, transfer, leave and discharge information must be kept up-to-date on SystmOne to ensure that bed occupancy can be accurately monitored. Any patient going on leave from the ward, should be recorded immediately, and updated as soon as they return
- any patient who has been admitted from out of area or overseas should be repatriated at the earliest opportunity
- the facilitation of early discharge by the Home-Based Treatment and Community teams should be prioritised where it is safe and appropriate to do so
- concerns regarding bed access pressures and those patients experiencing delays and the reasons for this, should be monitored in daily meetings and escalated accordingly to the senior leadership team and partner organisations
Please refer to the SystmOne in-patient guides (staff access only) via the following link for advice and further guidance.
4.1.6 Routes into hospital
There are only 3 lawful ways in which an assessing professional can admit a patient to hospital (without the intervention of the courts):
- under the Mental Health Act (1983) including community treatment order (CTO) and Ministry of Justice (MOJ) recalls
- informally (the patient gives fully informed consent)
- under the Mental Capacity Act (2005), in limited circumstances
Where a patient lacks the capacity to consent to being admitted for care and, or treatment and they do not object to this and to any treatment they will receive for mental disorder, the patient can be admitted under either the Mental Health Act or via the Mental Capacity Act under best interests, but the deprivation of their liberty will need to be authorised by a Deprivation of Liberty Safeguards (DoLS) authorisation. However, consideration should be given as to the overarching need for admission, for example, care and treatment for mental disorder, and balance which regime (Mental Health Act or Deprivation of Liberty Safeguards) is the least restrictive. See mental Capacity Act (2005) Deprivation of Liberty (DoL) policy for further guidance.
Note, an assessing professional is defined as a consultant, a section 12 doctor, an approved mental health professional (AMHP), a Community Treatment team (CTT) clinician of band 6 or above, a member of the home-based treatment, crisis resolution or Hospital Liaison team.
4.1.6.1 Assessments under the Mental Health Act
Assessments under the Mental Health Act will be completed by two doctors, one of whom must be section 12 approved and an approved mental health professional.
The Patient Flow team will not allocate or book beds prior to a face-to-face assessment being made including Mental Health Act assessments. The only exception where the trust patient flow will reserve a bed in advance of a Mental Health Act assessment will be for a Ministry of Justice or community treatment order recall, or in extraordinary circumstances where the presenting urgency and risk has been escalated by the approved mental health professional lead or service manager and this has been agreed by the head of patient flow (or the silver on call manager out of hours).
The assessing team should inform the Patient Flow team at the earliest opportunity of a planned Mental Health Act assessment pending including time of assessment and potential clinical needs. This allows the Patient Flow team to plan for a potential admission. At this stage, the Patient Flow team will not advise regarding the location of beds, but they may provide guidance on if a bed may be available within the trust if felt appropriate.
4.1.6.1.1 Gatekeeping
Prior to any bed being sourced, the admitting professional must ensure that all the necessary steps in the gatekeeping process have been followed.
The process of gatekeeping in mental health is the screening and approving of the decision to admit a patient into hospital. It also includes an assessment of the individuals’ needs and consideration of whether any identified risks and or the treatment required can be managed in the community.
A gatekeeping assessment ensures that patients are treated in the least restrictive environment possible and provides assurance that trust inpatient bed capacity is being used appropriately.
Admission to a hospital in-patient bed will only be supported where there are no safe alternatives for care or treatment within the community.
The gatekeeping process will determine if the patient’s treatment pathway is an adult or older person’s mental health ward due to frailty or physical ability.
The identified gatekeepers for adults of working age are:
- Doncaster, Intensive Home-Based Treatment team
- Rotherham, Crisis team, Intensive Home-Based Treatment team and the Hospital Liaison team
- North Lincolnshire, Crisis Resolution and Home Treatment team and Hospital Liaison team
The gatekeeping process differs for older adults. In these cases, the consultant, care coordinator or duty worker in the Older Person’s Community Mental Health team will “gatekeep”. If outside normal working hours or a transfer from the general hospital, this process may also involve the hospital liaison or Crisis team.
Once the gatekeeping process has been completed, and if a hospital admission is purposeful and required, a phone call should be made by the gatekeeper to the Patient Flow team so that a bed can be identified following discussion around the person’s needs and requirement for admission.
4.1.6.1.2 Gatekeeping for admissions under the Mental Health Act
Where a person has been assessed under the Mental Health Act and deemed appropriate for admission (either detained or to be admitted informally), this will act as the completed gatekeeping process. However, the Mental Health Act assessing team must contact the relevant gatekeeper for the patient’s locality to inform them of the assessment and to ensure involvement in the discussion for this to count as having been appropriately gate kept.
4.1.6.1.3 Gatekeeping for admissions when the patient is being admitted informally
No person can be admitted informally to an inpatient bed without having first been gate kept for admission and this decision must be clearly documented on the template on SystmOne.
Documented assurance must also be provided which shows that alternatives to admission have been explored and an admission to hospital is purposeful and the least restrictive option for the patient. This will be reviewed by the Patient Flow team prior to allocation of a bed.
Where possible a gatekeeper will be present at any 136 assessments to consider alternatives to admission when someone does not require detention under the Mental Health Act.
Note, for more information and guidance relating to gatekeeping, please refer to section 4.2.5 of the admission to adult and older persons mental health service inpatient wards procedure.
4.1.7 Sourcing a bed
Prior to any bed being requested, the admitting professional must ensure that all the necessary steps in the gatekeeping process outlined above have been completed. If gatekeeping has not been completed and is required for admission the admitting professional will be advised to complete this task before the patient is added to the to come in list.
Once a need for admission has been identified, the patient flow bed manager will be responsible for finding a bed. To request a bed the admitting professional is required to phone the Patient Flow team on 03000 211 850.
Only requests received via a phone call will be accepted. At the time of requesting the bed the admitting professional will be expected to provide the following information as part of the request and record on SystmOne:
- patient name, NHS number and date of birth
- current location
- legal status of the patient (Mental Health Act or informal, Mental Capacity Act consent (MCA1)
- the type of bed, which is required, for example, adult acute, psychiatric intensive care unit (PICU), organic, functional (if a psychiatric intensive care unit bed is required, section 4.1.8.3 of this procedure will be followed)
- the purpose of admission, diagnosis (if known) and the expected aims and outcomes of admission as jointly agreed by the admitting professional, the patient and their family, friends and carers (where appropriate)
- medical fitness and placement considerations, for example, physical health needs, language or cultural issues safeguarding concerns and legal issues
- the expected time of the patient’s arrival on the ward, how they will arrive and who will be accompanying them
The risk assessment is also to be updated by the admitting professional on SystmOne. In some cases, such as a Mental Health Act assessment which has been completed by an approved mental health professional or if the patient is in an out of area location, it is recognised that this may not be completed. In this circumstance, the approved mental health professional report will suffice, along with a verbal handover of any risk details or the originating areas documentation.
Prior to admission to a mental health inpatient setting, an assessment of a patient’s physical health care needs (including relevant blood tests and physical examination for patients over the age of 65) must take place, as it may be clinically necessary for them to be admitted to a general hospital in the first instance. This may require use of Mental Health Act (1983) to detain the patient to the acute general hospital. Prior to transferring to a mental health inpatient bed from an acute general hospital setting, a final physical healthcare review must have taken place within 24 hours to ensure the patient is medically fit and the receiving team are informed of any specific physical healthcare needs or adaptations required to support the patient on arrival and throughout their stay.
The patient flow bed manager will then advise the admitting professional of the bed availability and liaise with the ward to confirm admission. It is the responsibility of the admitting professional to contact the nurse in charge of the ward where the patient will be admitted providing a thorough and comprehensive handover prior to the patient arriving at the ward.
4.1.8 Bed allocation
On notification that a patient requires admission into a Rotherham, Doncaster and South Humber NHS Foundation Trust (RDaSH) bed, the patient flow bed manager will determine the named integrated care board (ICB) for the patient in the electronic patient record (SystmOne). This can be located within the general practitioner (GP) details section of the patients record.
Admission should only be agreed if the patient’s integrated care board is within the trust footprint unless a pre agreement or extenuating circumstance has been discussed with the head of patient flow, for example, the person being admitted is a colleague of another trust or mutual aid arrangements have been approved.
Where the integrated care board is unclear, or there is a discrepancy please refer to the who pays guidance which will support decision-making regarding admissions.
Once the patient has been confirmed as an RDaSH integrated care board funded patient. The patient flow bed manager will take clinical and demographic details to allocate an appropriate clinical pathway bed for that patient to be admitted.
The decision on pathway allocation will usually be reached through discussion of clinical needs with referrers, but final decision on pathway allocation rests with the patient flow bed manager (in consultation with the relevant inpatient team as and when necessary) as they have all the up-to-date knowledge of bed state and associated issues across the trust.
The patient flow bed manager will utilise a standard approach to ensure that patients are allocated beds in their own locality or close to that locality and that admissions are allocated evenly across the trust’s resources.
In the first instance, admission should be directed towards an available bed within the relevant care group, dependent upon risk assessment and suitability. The patient flow bed manager will be responsible for liaising with the nurse in charge (NIC) of the relevant ward and agreeing admission considering any issues or concerns re acuity, safeguarding, infection prevention and control and safe staffing levels.
In circumstances where the person to be admitted is or has been a member of the armed forces, the trust should comply with the Armed Forces Covenant.
The principles of which are:
- the armed forces’ community should enjoy the same standard of, and access to healthcare as that received by any other UK citizen in the area they live
- family members should retain their place on any NHS waiting list, if moved around the UK due to the service person being posted
- veterans should receive priority treatment for a condition which relates to their service, subject to clinical need
- those injured in service should be cared for in a way that reflects the nation’s moral obligation to them, by healthcare professionals who have an understanding of the armed forces culture
In practice point 3 above means that if you have two patients with the same level of clinical need, but the mental disorder of one is caused by service, they should be given priority for the bed. Point 4 means that a patient can request to be admitted under a team or clinician with armed forces expertise or decline to be repatriated away from such.
Patients must always be cared for in an environment that meets their clinical needs and is safe for all. In most cases, adults under 65 years of age are admitted to an adult mental health ward. Adults over 65 years of age are usually admitted to an older person’s mental health ward. However, there may be situations where it is more appropriate to admit to an alternative ward. There must be sound, clinical rationale for this, and it will be recorded on the patient electronic record (using the clinical frailty scale on SystmOne).
Some clinical examples may be.
- a person over the age of 65 but currently under the care of an adult mental health community team
- a person under the age of 65 but who meets the frailty criteria as proposed by the admitting professional and approved by the patient flow team in relevant consultation with the inpatient clinical team
Patients under 65 should not be admitted to an older person’s ward purely to manage bed pressures and the converse is true of people over 65 being admitted to an adult ward as doing so can introduce unnecessary risks to both patients and colleagues.
4.1.8.1 Frailty criteria
When there are concerns relating to frailty, to assist with determining which inpatient service to admit a patient to, the admitting professional should refer to the Rockwood frailty scale (appendix S). This is an easy-to-use guidance tool to support decision-making which covers general principles of frailty and its applicability to under 65’s which are typically seen in an older adult population. We will the tool to determine environmental suitability for the most appropriate inpatient care, rather than the nature of other interventions, which are individually care planned.
Patients who score 5 or below should be considered appropriate for admission to a ward for adults of working age (under 65 years) and patients scoring 6 should be considered appropriate for admission to a ward for older adults (over 65 years).
In addition to the bed referral form, the patient flow bed manager will complete the frailty score and enter this on SystmOne, taking all necessary clinical information from the admitting professional. In hours, patient flow will liaise with the relevant clinical team regarding the score, and a joint decision will be made. Out of hours this will be discussed with the nurse in charge of the ward ensuring the nurse has all the relevant clinical information re that patient so that an appropriate decision can be made.
If there is a dispute regarding the frailty score or concern regarding the purpose or appropriateness of the admission to the identified ward, in hours the inpatient responsible clinician or relevant deputy will be consulted and where necessary a multidisciplinary team (MDT) discussion will take place between the Inpatient and Community teams before the bed is allocated. Out of hours, the patient flow duty manager will liaise with the on-call consultant, and a joint decision will be made considering all the relevant clinical information.
Following admission, if the appropriateness of the bed allocation is disputed by the Inpatient Clinical team, the patient electronic record will be reviewed and the bed management form on SystmOne referred to as this will provide the rationale for the admission. Where necessary a joint multidisciplinary team discussion in hours will then take place between the relevant service and where necessary the patient will be reassessed and transferred to the most appropriate environment. Any lessons learnt will then be shared and actioned accordingly.
4.1.8.2 Admission and transfer of people living with dementia
Out of hours a person living with dementia presenting in acute onset crisis must have a physical health care review in the most appropriate setting prior to any assessment under the mental health act to rule out any physical causes for deterioration. The patient flow bed manager will seek assurance from the admitting professional and check the patient’s electronic record (where applicable) that all necessary physical healthcare investigations have been completed and that the patient is medically optimised for admission before a bed is allocated. This applies for all patients living with dementia regardless of setting.
Admission to hospital or transfer between inpatient services for those patients with a diagnosis of dementia should occur as a planned purposeful admission or transfer within core working hours of the specialist community or mental health team to avoid unnecessary harm and destabilisation. People living with dementia should not be transferred at night unless there is a risk to self or others and this rationale is evidenced within the patient electronic record.
Some clinical examples may be:
- the patient in accident and emergency (A&E) and has 2 medical recommendations for detention and an approved mental health professional has completed the application (if a bed has been identified)
- the patient is in a care home and continues to present with behaviours which challenge and cannot be managed safely
- the patient is at home, there are significant safety risks, and the patient has 2 medical recommendations for detention, and an approved mental health professional has completed the application (if a bed has been identified)
Any referrals relating to inpatient admission for a person living with dementia under the age of 65, must have a frailty assessment completed to determine the most suitable environment. A diagnosis of dementia does not automatically mean a bed will be allocated on an older person’s ward.
4.1.8.3 Consideration of bed allocation on a psychiatric intensive care unit ward
When a clinical team feels that transfer of an existing inpatient to psychiatric intensive care unit (PICU) is clinically necessary, or when a patient is assessed and due to their risk requires admitting directly to a psychiatric intensive care unit ward, part A of the psychiatric intensive care unit referral form will be completed on the patient electronic record by the admitting professional or multidisciplinary team representative who will then notify the Patient Flow team that this has been completed.
The Patient Flow team will ensure all the necessary information is contained in the referral form and will inform the relevant psychiatric intensive care unit ward that the referral requires screening, and the outcome will be recorded in part B of the referral form. It will be usual for clinicians in the receiving pathway to agree any such referrals to a PICU environment.
The Patient Flow team will maintain oversight of any transfer to a psychiatric intensive care unit ward. The exception to this, is when patient need, and safety will be compromised if the transfer is not made immediately. A copy of the psychiatric intensive care unit referral form and psychiatric intensive care unit flow chart (staff access only).
4.1.8.4 Dispute resolution
Within normal working hours, disputes within adult and older person’s mental health services over admission where a bed is available should be referred to the head of patient flow for a final decision. Disputes between services should be escalated to the patient flow clinical service manager in the first instance to arrange an urgent conference call between modern matrons or service managers to reach an agreement. If the dispute remains unresolved, it should be escalated to the relevant Care Group Senior Leadership team and head of patient flow.
Out of ordinary working hours, disputes should be reported to the silver on-call manager via the patient flow duty manager. The final decision rests with the silver and gold on-call manager, with clinical advice from the on-call consultant if needed.
4.1.9 Action if or when all inpatient beds are occupied
Due to the nature of adult mental health and older person’s mental health care provision, there will be occasions where the demand for inpatient beds outweighs the number of beds that are available. During normal working hours, modern matrons and ward managers are responsible for monitoring ward occupancy levels and liaising with the Patient Flow team.
To assist with sourcing an inpatient bed when there is no availability, the following steps should be taken.
4.1.9.1 Consideration of patient transfer
If the patient to be admitted, or a patient who is already on the ward can be transferred to another ward on site, within the locality or the wider trust based on meeting the frailty criteria and clinical judgement then this should be actioned. This would then make a bed available for the patient requiring admission.
Consideration of transfer to another ward or locality to create capacity must only be done where clinically indicated. Clinically indicated transfers may include:
- a patient who has been referred for, or would benefit from, transfer to a rehabilitation and recovery ward
- a patient who meets the admission criteria to an adult or older person’s ward
- admission to a crisis house is deemed appropriate
The following should be considered:
- the legal status of the patient
- the patient’s view on the transfer
- the receiving ward’s clinical view on the suitability of transfer
- the patient’s risk profile
- the impact on the patient’s recovery and the views of family or carers
- any safeguarding issues
- any infection prevention and control issues
The transfer of a patient will be coordinated by the Patient Flow team however, it is the responsibility of the ward manager or nurse in charge to ensure all relevant information is handed over to the receiving ward, including all identified risk factors by completing the trust patient transfer checklist. The nurse in charge will send the checklist to the receiving ward who will complete the receiving ward section.
No transfers should take place between the hours of 10pm to 7am unless there is an exceptional circumstance which is recorded in the patient’s electronic patient record and agreed by the on-call consultant.
4.1.9.2 Use of a leave bed
If no patients are suitable for transfer, then the use of a leave bed will be considered.
Prior to patients going on leave, the Clinical teams will consider the needs and risks of the patient to determine whether the bed can be utilised for another patient. If the clinical team have concern regarding the leave this should be classified as a red leave bed and the bed should not be used.
The criteria below are guidance for professionals as to when a bed should be recorded as red.
Leave bed should not be used:
- for the first episode of leave
- when the patient is on leave for less than 48 hours to their own home or a physical health acute hospital setting
- when a patient is subject to Ministry of Justice restrictions
- concerns are being expressed by family or carers or community team about risks or progress on leave that have not been addressed and resolved by the multidisciplinary team
- there has not been any verification of progress on leave from others involved in care where relevant
- home environment or leave destination is not suitable for community management
- when the view of the clinical team is that there is a significant risk that the patient may suddenly and unexpectedly return from leave
Things you might consider to determine significant risk may include:
- previously failed leave
- use of illicit substances that resulted in marked deterioration in mental state
- refusal to return from previous leave
- previous non engagement with agreed leave care plan
- a notable deterioration in mental state during previous leave or an increase in self-injurious behaviour whilst on previous leave
All beds of patients that are utilising overnight leave must be clearly documented on the patient’s electronic record (SystmOne) by the ward multidisciplinary team to assist the Patient Flow team in bed allocation and prevent unnecessary out of area admissions.
The Patient Flow team are to receive twice daily updates in the morning and afternoon handover meetings from the care groups regarding each current ward position to enable an understanding of the whole trust position.
4.1.9.2.1 Good practice guidelines relating to the use of leave and management of beds
- The timing of leave should be carefully considered for factors including, but not limited to, the purpose of leave, the timing of clinical review upon return, the impact of missing therapeutic ward activity and availability of community support (including carers, family and community services).
- Leave beyond 7 or more days would be unusual, however instances where leave exceeds 7 or more days the use of the leave bed must be considered.
- Where the patient on leave is detained under the Mental Health Act consideration should be given to any relevant restrictions and conditions around leave requirements and the implications of extending leave.
- Multidisciplinary teams should extend existing leave periods or bring forward planned leave (unless there are any barriers preventing early leave) when it is appropriate to do so, to enhance bed capacity, ensuring that the patient, family or carer and relevant community team are able to offer additional support.
Other alternatives to create flow will be considered by the multidisciplinary team and the following options should be explored and communicated where necessary to the Patient Flow team by the modern matrons:
- extending existing leave periods where this is clinically safe and appropriate, ensuring that the patient, family or carer and relevant community team are aware and able to offer additional support
- bringing forward planned leave where this is clinically safe and appropriate, ensuring that the patient, family or carer and relevant community team are aware and able to offer additional support
- early discharge might be considered where clinically safe appropriate. Where a patient is subject to section 3, 37, 45, 47, 48 and has aftercare entitlement under section 117 of the Mental Health Act then a section 117 aftercare meeting should be arranged first
4.1.9.3 Out of area (OOA) placements, trust patients
In extreme circumstances, when clinical demand for an in-patient bed exceeds the trust bed stock availability, trust patients may need to be accommodated in an out of area hospital placement, either in an alternative NHS setting or in the private sector.
An out of area placement is defined when, a person with assessed acute mental health needs, who requires an inpatient care, is admitted to a unit that does not form part of their usual local network of services. This means an inpatient unit that does not usually admit people living in the catchment of the person’s local community mental health service, and where the person cannot be visited regularly by their families, friends, carers and loved ones, and care co-ordinator or Lead Professional to ensure continuity of care and effective discharge planning.
A trust patient will ordinally be placed in an out of area NHS provider placement when mutual aid has been agreed from a neighbouring trust or due to the patient presenting in crisis to another NHS provider.
A trust patient may be placed in a bed in the private sector if the trust has subcontracted the bed or, due to no bed availability, the trust have had to spot purchase a bed. The Patient Flow team will have the most up-to-date information for bed availability for private providers.
Once a potential bed has been identified, it will be the responsibility of the patient flow bed manager to contact the provider and complete the referral paperwork. It is the responsibility of the admitting professional to ensure that all supporting documentation, the risk assessment and approved mental health professional report (where necessary) is up-to-date and accurate before the referral is sent for processing.
Within working hours (Monday to Friday, 9am to 5pm) the head of patient flow will be consulted and provide authorisation for any out of area placement. Outside working hours, the patient flow duty manager will undertake the necessary assurance checks that all other available options have been exhausted, admission out of area is therefore appropriate and will be responsible for processing the referrals. The patient flow duty manager will inform the head of patient flow of the admission via email including the rationale for the decision and complete an IR1 the head of patient flow will share the rationale with the relevant care group leaders, the next working day.
Please see appendix J which outlines the process for arranging and authorising an adult mental health or older persons out of area placement.
The Patient Flow team will inform the responsible integrated care board after placing a trust patient out of area by completing the integrated care board notification template.
Once the patient has been admitted, it is the responsibility of the patient flow officer to complete the out of area placement questionnaire on SystmOne. For patients formally admitted under the Mental Health Act, the admitting professional must ensure that the Mental Health Act paperwork reflects the correct unit being admitted to.
Should a patient refuse an admission to an out of area placement then the involved clinical team in conjunction with the patient flow duty manager, matron or service manager should be involved in decision-making in regard to next actions. Consideration should be given to the patient’s capacity, their reason for refusal and the alternative safe strategies that can be utilised to support the patient until a local bed is available.
The Patient Flow team will maintain oversight of out of area placements to ensure that:
- the out of area questionnaire’s on SystmOne are completed and accurate
- the out of area power business intelligence (BI) dashboard on RePortal is aligned to all known current out of area placements
- contact is maintained with the clinical team of any patient in an out of area placement at least once a week
- any patient that exceeds 30 days in an out of area placement will be visited by the Patient Flow team for the purpose of quality, assurance, and patient experience
- senior managers within the trust are informed of the number of out of area placements and the plans to repatriate
Please see appendix Q adult mental health and older persons out of area (OOA) placement monitoring process for the oversight of the monitoring requirements for all patients placed in an out of area placement.
The Patient Flow team will be responsible for coordinating the return of any out of area hospital placement to a trust bed or another clinical service at the earliest opportunity. Prior to the patient returning from out of area the Patient Flow team will liaise with the private provider to ensure the ward transfer checklist is completed and sent to the receiving ward before transport is arranged so the receiving clinical team has all the relevant clinical information regarding the patient and the repatriation confirmed. The transport will then be arranged by the ward currently caring for the patient and they will be responsible for providing a verbal handover to the receiving ward. The funding of transport will be the responsibility of the identified care group.
Prior to a detained patient being returned from out of area the patient flow bed manager will notify the appropriate Rotherham, Doncaster and South Humber NHS Foundation Trust (RDaSH) Mental Health Act Office of the proposed transfer and check that all the necessary paperwork relating to the section along with the form H4 to formally transfer detention under the Mental Health Act has been completed and will accompany the patient.
Note, the objectives set out in the NHS Five Year Forward View (2015) and NHS Long Term Plan (2019) states that out of area placements will essentially be eliminated for acute mental health care for adults by 2021.
Some patients choose to have their care facilitated out of area or require a specialist placement to meet their needs, for example, secure, male only or locked rehab services. As RDaSH is not commissioned to provide these services they are outside the scope of this procedure.
4.1.9.4 No trust or private provider bed availability
Where there are no trust or private provider beds available nationally, within hours, the head of patient flow will escalate to the Care Group Senior Leadership teams and the chief operating officer.
Out of hours, the silver on-call manager should escalate to the gold on-call manager who will then contact the integrated care board or NHS England to seek advice.
Should we have a patient who requires admission, and a bed cannot be identified by following the guidance in section 4.1.9.1 to 4.1.9.3 above, admission to a red leave bed or holding the patient (under section 140) in the health-based place of safety (section 136 suite) will be considered.
4.1.9.5 Use of a red leave bed
In extreme and exceptional circumstances and only when all the options outlined in the sections above have been explored and unsuccessful, the decision to admit a patient to a red leave bed may be made. Authorisation to do so has to be provided by the relevant Care Group Senior Leadership team (in hours) or the gold on-call via the silver on-call manager out of hours in consultation with the on-call consultant.
Admission to a red leave bed will only occur when there are no suitable beds available trust wide and should consider the following:
- identified levels of clinical risk and the impact on these if admission is not facilitated
- the patient’s liability to detention under the Mental Health Act
- family and social support and level of carer burden if the admission is not facilitated
If the decision is made to admit a person to a red leave bed, there should always be at least one red leave bed remaining across the trust. If a red leave bed is admitted into, an IR1 should be completed by the receiving ward.
4.1.9.6 Section 140 provision
4.1.9.6.1 Section 140 definition
Integrated care systems or local commissioners at place and local authorities are responsible for commissioning mental health services to meet the needs of their areas.
Under section 140 of the Mental Health Act (1983), local commissioners at place have a duty to notify local social services authorities (LSSAs) in their areas of arrangements which are in force for both:
- the reception of patients in cases of special urgency
- the provision of appropriate accommodation or facilities specifically designed for patients under the age of 18
The act refers to reception into a hospital, not specifically to a bed.
4.1.9.6.2 Special urgency definition
The term “special urgency” is a situation where a person experiencing a mental disorder is so acutely unwell that failure to urgently admit the person to hospital under the Mental Health Act or an excessive wait for a bed could cause significant harm, trauma, health issues or potential death of the patient, those assessing the patient or other members of the public.
The need for special urgency must be based on a current medical examination by a section 12 approved doctor or other doctor in consultation and agreement of a consultant psychiatrist (applicable to both detained and informal patients) due to their severe mental disorder.
The decision maker in respect of whether a case meets the “special urgency” criteria will be the section 12 doctor or consultant psychiatrist who may consult with the approved mental health professional in cases of Mental Health Act assessments to determine urgency and risk. The assessment may also include consultation with the clinical colleagues normally involved in the person’s care, police or ambulance colleagues in attendance or Crisis Home Treatment teams.
Where a Mental Health Act assessment is not required, the urgency and risk will be assessed through the gatekeeping process. In all cases this will be approved by the clinicians detailed above, following a current risk assessment.
The following is not an exhaustive list but is proposed as guidance for the identification of “special urgency” for adults under section 140:
- an episode of immediate life-threatening self-harm or severe suicidal intent and clearly identified severe mental disorder signs and symptoms
- acute and severe mental disorder in a community setting with other high-risk factors, for example living alone with lack of engagement with Community teams, non-concordance with treatment including medication, self-neglect, active agitation and, or thoughts of self-harm or harm to others
- patient with such severe mental disorder that they lack capacity to carry out activities of daily living including self-care and who present with severe self-neglect, for example showing features of dehydration or sustained food refusal
- patient showing features of relapse of mental disorder and presenting with a serious risk of significant harm to others, with other high-risk factors including non-concordance with medication, disengagement from services, carrying weapons and, or making threats to harm others
If the criterion for special urgency is met, the admitting professional must advise the patient flow bed manager of the name of the doctor who has assessed and approved this. The rationale should also be in the electronic patient record (EPR).
Note, children and young people (under 18 years of age) are always assumed to be in “special urgency” regardless of the situation, though decision-makers should always consider whether there are less restrictive options as alternatives to detention under the act.
4.1.9.6.3 Exclusion criteria
Where patients meet any of the criteria outlined in section 4.1.9.6.2 but are already in a place of safety, A&E or in police custody ‘special urgency’ may not apply if a clear plan is in place to manage risks to self and others.
Acute presentations requiring hospital admission or detention under the Mental Health Act would not, on their own, be deemed cases of “special urgency”.
4.1.9.6.4 Section 140 provision for adults or older persons
For the reception of adults and older persons in cases of special urgency, the inpatient wards as detailed in appendix H adult and older persons mental health bed capacity are available.
If there are no available or appropriate beds within the above listed provision, it may be necessary to procure a bed with an alternative provider. This could be with an alternative NHS trust or with a private provider as detailed in section 4.1.9.3.
Where no bed can be sourced in a timely manner, the trust will receive adult or older persons into the section 136 suites (subject to availability) in cases of special urgency as defined above.
4.1.9.6.5 Section 140 provision for children and young people under the age of 18
The trust is not commissioned to provide inpatient services for children and young people under the age of 18.
The commissioned inpatient services for children and young people in Doncaster, Rotherham and South Humber are as follows:
- South Yorkshire integrated care board, The Becton Centre, Sheffield
- North Yorkshire and Humber Integrated Care Board, Inspire, Hull
Therefore, all under 18 admissions for the purpose of section 140 should be referred to these services.
4.1.10 Management of patient flow
4.1.10.1 Clinical responsibility
Once a patient has been admitted to another care group, their care becomes the responsibility of the clinical team on that ward and will remain with them until the patient is discharged or transferred back to their home locality. It is the responsibility of the care coordinator or lead professional from the patient’s home locality to maintain contact with the patient at least once a week, whilst they are on another care group’s ward.
For patients in out of area specialist placements, responsibility for liaison and clinical updates lies with the care coordinator or lead professional. All clinical updates and liaison are to be documented clearly on SystmOne.
4.1.10.2 Patients clinically ready for discharge (but delayed)
To ensure a collective understanding of what we mean by a delayed discharge and enhance partnership working across multiple organisations, NHS England has produced a national definition of “clinically ready for discharge” for mental health inpatients, to replace the previous delayed transfer of care (DToC) reporting.
A patient is clinically ready for discharge (CRFD) when the multidisciplinary team conclude that the person does not require any further assessments, interventions and, or treatments, which can only be provided in the current inpatient setting.
To enable this decision:
- there must be a clear plan for the ongoing care and support that the patient requires after discharge, which covers their pharmacological, physical health, psychological, social, cultural, housing and finances, and any other individual needs or wishes
- the multidisciplinary team must have explicitly considered the patient and their chosen carers’ views and needs about discharge and involved them in co-developing the discharge plan
- the multidisciplinary team must also have involved any services external to the trust in their decision-making, for example, Social Care teams, where these services will play a key role in the person’s ongoing care
Working in collaboration with all relevant multidisciplinary teams, the Patient Flow team will maintain oversight of any patients identified as clinically ready for discharge (CRFD) (but delayed) and ensure that patients are assessed for supported discharge on an ongoing basis. Suitable patients should be referred to home treatment or Community teams according to the early discharge protocol.
The Patient Flow team will work closely with patient flow co-ordinators on the wards to identify and solve issues preventing discharge from hospital.
Multidisciplinary teams, care coordinator’s or lead professional’s and the Patient Flow team will work with all agencies involved with these patients to minimise delays and facilitate transfer as quickly as possible
4.1.11 Exceptional clinical issues relating to patient flow
4.1.11.1 Support for allied mental health practitioners and community teams when making decisions in situations where no beds are immediately available
This guidance is designed to provide support and information to approved mental health professionals when making decisions in relation to scenarios where no bed is immediately available for a person being assessed under the Mental Health Act.
Each situation will differ and should be considered on a case-by-case basis. Support can also be sought via other approved mental health professional colleagues, the approved mental health professional lead and other on-call colleagues if discussion and joint decision-making is required.
- Approved mental health professionals have a legal duty to consider all requests for a Mental Health Act assessment under section 13 of the Mental Health Act.
- A blanket stance of not acting on a request would be in breach of this duty; therefore, consideration and triage of the request must take place, whatever the resources. However, it may be necessary and justified in some circumstances to delay the interview element of the assessment, but this must not be solely down to the lack of a bed if, had there been one, it would have gone ahead. Examples of such circumstances to delay may be the person is likely to abscond, harm themselves or others as a result of the assessment. The reasons for the decisions to delay should always be recorded by the approved mental health professional.
- Once the need for a hospital admission has been established, it is important that all parties work cooperatively to help make the necessary arrangements for the patient. A bed will always be sourced for patients when needed, however if this is not immediately available, the approved mental health professional, the assessing doctors and others involved in the process (including carers) should work together to formulate a safety plan to manage the risk whilst continued efforts are made to source an inpatient bed by the Patient Flow team.
- The referrer and other relevant health colleagues (for example, care co-ordinator, Dr, Crisis and Home Treatment team) will need to retain their usual responsibilities for supporting the person whilst the request is considered and coordinated.
- Part of the role of an approved mental health professional (once a decision has been made to pursue hospital admission) is to make the necessary arrangements for the conveyance of the person to hospital. If a hospital bed is not immediately available, it will not be possible for the approved mental health professional to complete the assessment process or indeed to make an application in respect of the involved patient. This also applies in cases of special urgency.
- If there is significant concern or historical evidence that the act of carrying out a Mental Health Act assessment will trigger an extreme reaction (for example, aggression or violence) that would present a risk to those in attendance or the person themselves, then consideration should be given to request Police attendance or apply for a section 135(1) warrant to manage the assessment in a more contained fashion, if the criteria for this are thought to be met.
- The safety and well-being of the person and those around them is the responsibility of all those mental health and social care professionals involved in their care and support and these responsibilities do not end when a Mental Health Act assessment is requested or carried out.
4.1.11.2 Process to follow when a request for a Mental Health Act assessment is made or completion of a Mental Health Act assessment and no bed is currently available and one is not likely to be available imminently
A joint risk assessment of the situation for patients in the community and acute general hospital settings with the relevant health and social care colleagues involved in the patient’s care including approved mental health professionals, crisis, Home Based Treatment and Hospital Liaison teams will need to be undertaken.
Information from this risk assessment will be used to develop a safety plan which must be documented on the patient’s electronic record and shared with the relevant health and social care colleagues who will be supporting the person in the interim period. Details of the safety plan must be shared with the trust Patient Flow team by the admitting professional and the relevant team who are providing support for the patient to maintain oversight of the safety plan in the interim period.
Decisions about what to inform the patient and where relevant their family, friend or carers at this time are to be considered on a case-by-case basis but where possible approved mental health professionals should aim to be open and honest about what support is planned and how it will be monitored and coordinated. Contact details for the relevant services are to be shared or support or information. This needs to include advice to contact emergency services 999 if there is an immediate risk to life or limb.
The approved mental health professional will ensure medical recommendations are stored safely where they can be accessed later:
- for people on medical wards or in custody place within person’s notes
- for people in the community, place with Crisis team or Home-Based Treatment team other 24-hour accessible place (it is recommended to designate an agreed place in each locality for this purpose)
- ideally also ensure copies are scanned up to the person’s record so they can be used electronically if required.
If the assessing approved mental health professional is willing to be contacted outside their shift to make an electronic application in the event of a bed becoming available, then please make approved mental health professional colleagues aware in order that they can avoid a repeat assessment and instead proceed on the basis of this application. There is no expectation for approved mental health professionals to do this.
Feedback should be provided to approved mental health professional team colleagues on the current situation and where the relevant information or papers can be found.
The type or level of mental health care available to the patient awaiting the allocation of a bed, cannot be insisted by the approved mental health professional service. The law is clear that an approved mental health professional cannot be expected to address the delay themselves, the responsibility rests with all mental health services. The approved mental health professional service should work collaboratively with all parts of the service to minimise the risk and distress to the patient and others.
4.1.11.3 Unplanned admissions of non-trust patients
On occasion, patients from other NHS trust areas will present to trust services and require hospital admission. If trust services complete an assessment for a patient from another locality (outside Rotherham, Doncaster and South Humber NHS Foundation (RDaSH) Trust), it is the responsibility of the admitting professional to liaise with patient flow who will then notify the relevant trust that we have assessed their patient and they require admission. The Patient Flow team will liaise with the admitting professional and the patients’ home area to make the most appropriate plan to meet needs and safety.
The patient should be admitted to their home area, but when this is not possible or regarded as unsafe, in extreme and exceptional circumstances the patient will be admitted to a RDaSH bed (if available) and repatriated to their home area as soon as possible.
If the home area does not have a bed (assuming the person is fit to travel) and there is no bed available within RDaSH, the patient flow bed manager, will get written confirmation in an email that the patient’s home area will fund the bed. Attempts will then be made to source an out of area placement. As the admitting professional will be with the patient and having completed the most recent assessment, it may be necessary to contact the home area for collateral information. When completing the funding form all relevant details for the home area as this will go on the form for payment of the bed and any transport arranged.
The Performance team will collect information on all out of area activity (incoming and outgoing) and report to relevant stakeholders on issues and trends.
The Patient Flow team will liaise with the trust finance department to ensure that all recharges are accurately processed.
4.1.11.4 Non-trust patient in accident and emergency
There may be an occasion whereby a non-Rotherham, Doncaster and South Humber NHS Foundation (RDaSH) integrated care board patient is assessed in A&E and requires admission. On this occasion it is the responsibility of the patient flow team to:
- identify the appropriate patient flow or bed management team of the patient’s home locality and notify them of the patient requiring admission
- the patient flow team will obtain the home locality’s bed management and escalation contact details and share this with the admitting professional and appropriate team within the trust and where necessary the local acute trust caring for the patient
- share the contact details via the system co-ordination centre (SCC) for any escalations between the A&E department and the receiving trust to take place
When this is complete the patient flow team will relinquish their responsibilities.
It is the responsibility of the admitting professional to maintain contact with the identified trust regarding bed availability.
If the patient is detained under section 136 and reaches 18 hours without a bed identified, escalation to the RDaSH patient flow team is required to discuss contingency planning and the options available until a bed can be sourced within the patient’s home locality.
4.1.11.5 Care of children and young persons with a mental disorder
4.1.11.5.1 16 to 18 years
Whilst it is accepted that the admission of a young person to an adult mental health ward should not occur as the trust is not commissioned to provide these services, there may be exceptional circumstances in cases of urgent necessity and the absence of satisfactory immediate alternatives where in the short term, this may need to occur for a young person suffering from mental disorder between the ages of 16 to 18 years.
Prior to assessment the assessing team must refer to the Children and Young People’s Crisis team who operate 24 hours a day, 7 days a week and cover trust wide receiving referrals for young people under 18 presenting with a mental health concern, who may pose a significant risk to self or others. Referrals can be made 24 hours a day, 7 days a week by phoning single point of access (SPA) on 03000 218 996, option 2 (mental health services) followed by option 1 (urgent).
Please have all demographic information, circumstances of presentation and any other key information to hand.
Non-urgent phone number for professionals, Monday to Friday 9am to 5pm, 03000 213 101.
During the assessment of any young person, to decide whether admission to an adult acute mental health ward is appropriate, the following must be considered:
- under what grounds they will be admitted.
- what, if any, treatment plan is appropriate; and
- how any needs the young person has will be met during the admission.
An adult mental health ward will only be used if no specialist tier 4 child and adolescent bed can be secured and it is an emergency situation with admission to an adult acute mental health ward or the health-based place of safety (section 136 suite) being the only safe option.
If the patient is not admitted under the Mental Health Act 1983 the patient’s capacity to consent to the admission must be considered. If the patient lacks capacity and the “acid test” is met parental responsibility cannot be relied on to consent to the deprivation of liberty and an urgent application will need to be made to the Court of Protection to authorise the deprivation of liberty. The Mental Capacity Act lead or Mental Health Act Manager should be consulted in these cases.
The assessing team will contact the Patient Flow team and the child and adolescent mental health services (CAMHS) crisis and intensive community support service manager.
When making this call, the assessing service will provide the following details:
- name of the patient
- age of the patient
- reason for admission
- the child or young person’s ability to consent or not to the admission
- details of any safeguarding children concern
- any identified risks
- child protection status
- the reason why an admission to an acute general hospital is not appropriate
- the alternatives to admission to an adult acute mental health ward that have been explored and a rationale as to why these are not suitable or available
During core working hours, the child and adolescent mental health service (CAMHS) clinician must seek authorisation from the relevant Care Group Senior Leadership team to admit into an adult mental health bed or if deemed more clinically appropriate, the health-based place of safety (section 136 suite).
Out of hours authorisation will be sought from the gold on-call via the silver on-call manager to admit into an adult mental health bed or the health-based place of safety (section 136 suite).
In circumstances when this occurs an IR1 must be completed by the receiving ward or section 136 suite and the Care Quality Commission notified (via the local Mental Health Act Office).
If the decision has been made to care for the child or young person in the health-based place of safety (section 136 suite), this will remain closed for the duration of the placement and the local police force notified of the closure (as per section 136 closure procedure).
4.1.11.5.2 Under 16 years
There should be no circumstance in which a patient under the age of 16 will be admitted to a Rotherham, Doncaster and South Humber NHS Foundation Trust Adult mental health bed or the section 136 suite.
A patient under the age of 16 should be admitted to a tier 4 age-appropriate Child and adolescent mental health service (CAMHS) unit or the paediatric ward at their local Acute General Hospital Trust.
For further guidance regarding children and young people’s mental health service admissions please follow the links below:
- care and treatment of children under the age of 18 on adult acute mental health inpatient areas policy
- children and young people’s mental health service out of hours service standard operating procedure
4.1.11.6 Patients with a diagnosis of learning disability and or autism
4.1.11.6.1 Definition
A learning disability (LD) is currently defined by the DSM-5 as limited functioning within social skills, conceptual skills and practical ability. With the ICD-11 stating:
“A condition of arrested or incomplete development of the mind, which is especially characterised by impairment of skills manifested during the developmental period, which contribute to the overall level of intelligence, for example, cognitive, language, motor and social abilities.”
Within the trust, a learning disability is primarily assessed through WAIS-IV testing, providing a comparative score against the global population, diagnostic testing can also be complemented by functional assessments for a more accurate representation of an individual’s needs. Therefore, someone with a learning disability may be eligible for specialist services with an intelligence quotient (IQ) score of 70 and below, however, there should be consideration of the individual’s primary need to determine which service is the most appropriate to provide support and guidance states that there should be “inclusivity of mainstream mental health services for people with learning disabilities who have mental health problems”.
A learning disability can be classified as mild, moderate or severe.
Autism is a neurodiverse condition, with or without the presence of a learning disability. Someone with autism may have presented in crisis to the Community Learning Disability team or the Community Mental Health team, the process is the same irrespective of which team they have presented to.
4.1.11.6.2 Inpatient care
The transforming care agenda, building the right support and homes not Hospitals aims to enhance community capacity, thereby reducing inappropriate hospital admissions and subsequent length of stay and there are currently no local NHS provisions of assessment and treatment units.
It is accepted that the admission of a patient with a primary diagnosis of a learning disability and, or autism to one of the adult or older person’s mental health in-patient wards should not occur as the trust is not commissioned to provide these services. Should someone require a specialist admission, the integrated care board with support from the patient’s care co-ordinator will lead on the sourcing of a suitable bed.
However, there may be circumstances when an admission to an adult or older person’s mental health ward may be necessary, for example:
- when mental health is presenting as the patient’s primary need
- there is an increased risk of harm to self and others, which cannot be managed within a community environment
- following a breakdown of the community placement and the patient being detained under the Mental Health Act
- following a breakdown of the community placement and the patient being subject to an order of the Courts and, or Deprivation of Liberty Safeguards
4.1.11.6.3 Pre-admission
Prior to admission to hospital a patient with a diagnosis of learning disability and, or autism, who is thought to be at risk of a hospital admission, should already be known to local services and will be placed on the dynamic support register (DSR). If someone is presenting as “at risk of admission” they would hold a red rating and throughout the period of admission, the person will remain on the dynamic support register. The dynamic support register will be held by the integrated care board with involvement from the Learning disability Community teams and be reviewed every 2 weeks in a multi-professional team meeting.
Prior to admission a local area emergency protocol (LAEP) should be implemented with recommended outcomes and contingency plans associated to the admission. The local area emergency protocol recommendations should be shared with the patient flow team and admitting ward, with a full care and treatment review (CTR) arranged by South Yorkshire Integrated Care Board or Humber and North Yorkshire Integrated Care Board. The local area emergency protocol process will consider if someone is suitable for a mental health inpatient environment or if they require specialist learning disability inpatient services.
4.1.11.6.4 Admission
Anyone with a diagnosis of a learning disability and, or autism who is detained under the Mental Health Act will be eligible for a care and treatment review.
There may also be occasions when someone is unknown to local learning disability or mental health services, and this will be identified upon admission. A single access referral form should be completed to request support from the relevant community team.
Should someone be suspected of having a learning disability, diagnostic assessments would not be undertaken during a period of mental illness as this would invalidate the assessment, however they can be referred for future assessment when they are no longer presenting with an acute episode of mental illness.
At the point of and during subsequent admission, reasonable adjustments need to be implemented to ensure accessible care. These adjustments will be person specific, however will need to include easy read or accessible information regarding the legal framework they are admitted under.
In circumstances where the patient is admitted following the breakdown of a community placement either under the Mental Health Act or subject to an order of the Court or Deprivation of Liberty Safeguards, the following actions must be taken:
- the trust Mental Health Act manager should be notified, at the earliest opportunity to ensure that the appropriate legal framework is in place and where necessary that the trust solicitors are consulted
- escalation to the chief operating officer, in order that there is senior oversight of the case within the trust
- regular update meetings are held with the appropriate integrated care board representatives, local authority representatives, placement representatives and ward manager or modern matron, in order to ensure either the patient returns to the placement, or that an alternative placement can be found
The local community learning disability teams will liaise with the ward manager to confirm the in-reach support requested during admission, on a needs-led basis. This will then be discussed with the crisis and intensive support team (Doncaster) or the relevant clinical pathway (mental health pathway or positive behaviour pathway) for Rotherham or North Lincolnshire for agreement. Any disputes will be escalated to the relevant service manager or modern matron.
In-reach support will not ordinarily include the community team working on an inpatient ward.
4.1.11.7 Restricting of beds and requests to close a ward
There may be occasions when due to clinical issues relating to safety, a request is made to restrict beds or close a ward to admissions. All requests to restrict beds should be directed to the care group leadership team by the ward. If the restriction is agreed, the care group will inform the Patient Flow team.
Please refer to appendix R which outlines the governance process for an adult and older person’s mental health ward closure.
In the event of a critical or major outbreak that causes the closure of multiple wards the chair of the trust’s Outbreak Control team will notify the accountable emergency officer (AEO) and directors of all the care groups. Please refer to the outbreak of infection management procedure for information.
4.1.11.8 Short term sickness or absence cover arrangements for the patient flow officer and duty manager
In the event there is short term absence of the patient flow officer, the patient flow duty manager, will be responsible for bed managing throughout the period of absence.
If there is short term absence of the patient flow duty manager, the following action will be taken:
- a review of the patient flow roster will be completed by the patient flow clinical service manager to identify any potential shift swaps or change in working patterns to fill vacant shifts
- offer of flexible or home working to be explored
- offer of overtime or bank to band 7’s across the trust or person with relevant experience to fill any operational cover required
- offer of overtime or bank to band 4 or person with relevant experience to fill any out-of-hours bed management cover required
If the above has been explored and there is still no patient flow duty manager cover, in hours (9am to 5pm) the patient flow clinical service manager will cover the role of the patient flow duty manager throughout the period of absence.
If the absence occurs out of hours, it is the responsibility of the patient flow duty manager to inform silver on call of the absence.
The bed management duties will then be delegated to the nurse in charge or unit co-ordinator (where applicable) of each care group (Doncaster, Rotherham and North Lincolnshire). Silver on call will be required to answer all operational calls throughout the period of absence.
The care group bed manager will be the first point of contact to ascertain bed availability and coordinate any admission to hospital that is presented to them by the out of hours admitting professional.
This can include but is not limited to:
- liaising with other care group bed managers to ascertain bed availability and coordinate admissions
- supporting the admitting professional with liaising with other trust Bed Management teams to ensure anyone that falls outside the scope of the trust’s footprint is admitted to the appropriate NHS trust (see section 4.1.8)
- processing referrals into trust psychiatric intensive care unit beds (see section 4.1.8.3)
- completing and sending referrals to out of area placements where necessary (see section 4.1.9.3)
At the end of the out of hours period it is the responsibility of the care group bed manager to e-mail the patient flow inbox rdash.patient-flow-team@nhs.net with any action taken overnight, and any tasks to be carried forward into the following shift.
4.1.12 Governance, learning and escalation
4.1.12.1 Governance
To ensure good governance, maintain effective communication and escalate concerns relating to patient flow proactively, the following meetings are in place:
- a daily on call morning handover (Monday to Friday at 9:15am)
- a daily on call afternoon handover (Monday to Friday at 4pm)
- weekend planning (every Friday at 11am)
- weekly care group multi-agency clinically ready for discharge (but delayed)
- bi-monthly trust wide clinically ready for discharge (but delayed) oversight
- bi-monthly trust out of area oversight
- integrated care board system pressures calls, once a week as a minimum and stepped up as and when required
Ad hoc meetings will also be convened with Clinical teams and partnership agencies where necessary to discuss complex cases.
4.1.12.2 Learning and continuous improvement
With the aim of identifying future learning needs for individuals, teams and the trust whilst also highlighting areas of good practice, the Patient Flow team will undertake case reviews to examine situations that have caused a disruption in patient flow in the trust.
All case reviews will be completed with input from clinical colleagues or teams, and the findings will be used to support and transform the patient flow within the trust by identifying areas of process development and prevent future disruptions in service.
On completion each case review will be tabled and presented at the relevant care group quality and assurance meeting for discussion and subsequent sign off. Following sign off, anonymised themes regarding lessons learnt and actions identified will be shared at trust level within the trust organisational learning forum.
As part of the patient safety incident response framework (PSIRF) and to enhance our governance relating to patient care, experience and risk management, colleagues will complete IR1’s to identify opportunities for learning and further development of the service.
The Patient Flow team will complete an IR1 relating to an adverse healthcare event, admission or transfer or discharge planning issues, due to lack of bed availability in the following circumstances:
- when a patient is sent inappropriately out of area
- if a patient in A&E has been waiting for a mental health bed for over 12 hours
- if a patient in the community (who will be being supported by a community team) has been waiting for a mental health bed over 24 hours
- if a patient has been admitted to the 136-suite due to lack of bed availability elsewhere or for the purpose of section 140
The Patient Flow team will also support colleagues as required by facilitating debriefs to discuss clinical and operational issues and enable continuous improvement.
4.1.12.3 Escalation
The following escalation and governance process for patient flow with agreed authorisation and escalation criteria has been approved and implemented regarding managing beds within working hours.
Outside business hours, the existing on-call management structure will remain responsible for the management of patient flow including all necessary escalations and authorisations. See patient flow escalation framework (staff access only).
4.2 Admission to adult and older persons mental health service inpatient wards procedure
4.2.1 Aim
The aim of this procedure is to set out the specific standards for when a patient is admitted to one of the adult or older person’s mental health service inpatient wards. Admission to hospital can be a difficult time for both the patient and their carers and can bring on feelings of vulnerability. For this reason, it is important that we make people feel safe and secure and that they feel that they have received personal and individualised care.
4.2.2 Scope
The contents of this procedure apply to clinical colleagues working across adult and older person’s mental health inpatient services.
4.2.3 Access or pre-admission
All referrals for a mental health assessment go to the community and, or hospital liaison, crisis, and Home-Based Treatment teams for assessment.
As part of this assessment the identified professional will consider the least restrictive option in which to provide care and treatment, taking into consideration the patient’s wishes, in line with the level of identified clinical need and risk. Crisis plans and advance statements will also be considered when arranging care.
If the outcome of a Mental Health Act (MHA) assessment is that a patient does not require an in-patient bed but may be suitable for home treatment, the admitting professional should discuss with the available gatekeeping for the patient’s locality as identified in section 4.2.5.
4.2.3.1 Patients assessed as requiring an inpatient admission
There are only 3 lawful ways in which an assessing professional can admit a patient to hospital (without the intervention of the courts):
- informally (the patient gives fully informed consent)
- under the Mental Health Act (1983)
- under the Mental Capacity Act (2005), in limited circumstances
Where a patient lacks the capacity to consent to being admitted for care and, or treatment and they do not object to this and to any treatment they will receive for mental disorder, the patient can be admitted under either the Mental Health Act or via a deprivation of liberty safeguards (DoLS) authorisation. However, consideration should be given as to the overarching need for admission, for example, care and treatment for mental disorder, and balance which regime (Mental Health Act or Deprivation of Liberty Safeguards) is the least restrictive.
Prior to a patient being admitted, the admitting professional should ensure that where possible they understand the reason for admission and why they need to be in hospital.
For those patients who are formally admitted to an Inpatient Ward under a section of the Mental Health Act (1983), colleagues must adhere to the requirements of the Mental Health Act (1983) and the Mental Health Act Code of Practice (2015).
For those patients who lack the capacity to make the decision to be admitted to hospital, colleagues should on admission ensure that the principles of the Mental Capacity Act (2005) have been followed:
- that an assessment of capacity has been undertaken and documented
- that where the decision to admit the patient is made in the best interests of the person, that there is a record of this
4.2.3.2 Assessments and documentation
When an inpatient mental health admission has been identified as part of an initial assessment or by a mental health treatment team the following process should be followed.
The admitting professional will ensure the following assessments and documentation is completed and documented on SystmOne:
Patients who are new to service:
- mental health assessment and review (full needs assessment)
- functional assessment of care environments (FACE) risk assessment
- complete the mental health clustering tool
- next of kin or carer details and contacts
Patients already known to a treatment team:
- update the functional assessment of care environments risk assessment to reflect any change in the patient’s clinical presentation and risk profile
- ensure the mental health assessment and review (full needs assessment) is up-to-date
- check and confirm whether there are any changes to the next of kin or carer details and contacts
- re-cluster (using the mental health clustering tool) to reflect the deterioration in mental health and increased need which led to admission
If the admission is outside of normal working hours and there is a concern that the admitting professional will have to attend another assessment or attend to other duties that could result in disruption to the completion of assessments for the admission, these documents will be completed at a later time (but before the end of their shift) by the admitting professional.
4.2.3.3 Action for those patients being admitted to hospital informally
In order for the patient to make an informed choice regarding admission if they are not detained under the Mental Health Act (1983), the admitting professional should give the patient as much information as possible about the ward and provide them with a copy of the informal admission leaflet (see appendix C) and specifically discuss that the wards are smoke free and that when infection prevention and control (IPC) guidance stipulates, they may be required to isolate on admission. Please refer to the assessment and treatment provided by community services during COVID-19 (including Mental Health Act assessment) standard operating procedure for further information.
For informal patients, an assessment of capacity should be undertaken and recorded on an MCA1 by the professional making the decision to admit to evidence the patient’s capacity to consent to the admission.
For patients who lack the capacity to consent to informal admission who are not liable to detention under the Mental Health Act, a best interest decision should be made by the professional making the decision to admit and recorded on an MCA2 and authorisation should be sought under the Deprivation of Liberty Safeguards immediately. Please see Mental Capacity Act (2005) Deprivation of Liberty (DoL) policy
4.2.3.4 Gatekeeping
Prior to any bed being sourced, the admitting professional must ensure that all the necessary steps in the gatekeeping process have been followed. Where a person has been assessed under the Mental Health Act and deemed appropriate for admission (either detained or informal), this would act as the completed gatekeeping process.
No person can be admitted informally to an inpatient bed without having first been “gate kept” for admission and this decision must be clearly documented in the template on SystmOne. Documented assurance must also be provided which shows that alternatives to admission have been explored. This will be reviewed by the patient flow team prior to allocation of a bed.
Where possible a gatekeeper as identified below, would be present at any 136 assessments in order to consider alternatives to admission when someone does not require detention under the Mental Health Act.
Overall, the gatekeeping process ensures that patients are treated in the least restrictive environment possible and provides assurance that trust inpatient bed capacity is being used appropriately.
The gatekeepers will determine if the patient’s treatment pathway is an adult acute mental health ward or older person’s mental health ward due to frailty or physical ability.
4.2.3.4.1 Gatekeeping process of adults of working age
The identified ‘gatekeepers’ for each area are:
- Doncaster: Home Treatment team
- Rotherham: Crisis team, Home Treatment team and the Hospital Liaison team
- North Lincolnshire: Access team, Home Treatment team and Hospital Liaison team
4.2.3.4.2 Gatekeeping process for older persons
The gatekeeping process differs for older adults. In these cases, the consultant, care coordinator or duty worker in the Older Person’s Community Mental Health team will “gatekeep”. If outside of normal working hours or a transfer from the general hospital, this process may also involve the hospital liaison or Crisis team. The assessment prior to admission should include a review of the patient’s medical needs as it may be required for them to be admitted to the general hospital. This should be considered prior to admission to the mental health unit.
4.2.3.5 Sourcing of a bed
Once the gatekeeping process has been completed, a phone call should be made by the gatekeeper to the patient flow bed manager (within working hours 8am to 8pm, 7 days a week) so that a bed can be identified following discussion around the person’s needs and requirement for admission. The patient flow bed manager will review the bed state and in the first instance will contact the wards in the relevant care group to confirm bed availability. Outside of working hours (8pm to 8am, 7 days a week) a member of the hospital liaison, crisis or home-based treatment team will be responsible for sourcing a bed (when the approved mental health practitioner is the admitting professional, they will delegate this responsibility) and they will liaise with the identified care group bed manager regarding availability. The bed manager for each care group will be identified in the “patient flow management document” which is sent out after the mental health handover meeting every day.
At the time of requesting the bed the admitting professional will provide the following information and record on SystmOne:
- patient name, NHS number and date of birth
- legal status of the patient (Mental Health Act or informal)
- the type of bed, which is required, for example, acute, psychiatric intensive care unit (PICU), organic, functional
- reason for admission and expected outcomes of admission
- the expected aims of admission as agreed among the admitting professional, the patient and where appropriate their carers
- expected time of patient arrival on the ward, how they will arrive and who will be accompanying them
The Patient Flow team or care group bed manager will then advise the admitting professional of the bed availability and liaise with the ward to confirm admission.
If a bed is not available within the trust and capacity cannot be created by urgently reviewing and utilising a leave bed (where safe), the out of area process must be followed (see appendix J)
4.2.3.6 Handover process
The admitting professional will ensure a thorough handover is given to the receiving ward. In addition to the information detailed in section 4.2.6. The following admission details must be discussed and confirmed with the nurse in charge of the ward and recorded on SystmOne:
- current clinical risk profile of the patient and that the admitting professional will complete or update the patients’ functional assessment of care environments (FACE) risk assessment. If the admission is due to a transfer from another inpatient ward in the trust, the FACE risk assessment must be reviewed and updated
- further information around risk, for example, risk to self, risk to others, falls, and any adult and, or child safeguarding concerns, multi-agency public protection arrangements (MAPPA) status where known and any bail conditions or restrictions if the patient has been seen by the Liaison and Diversion team
- any caring responsibilities that the person being admitted to hospital may have for family, relatives including children or animals and how this is going to be managed
- the patient’s physical health care needs and requirements, including any details of recent investigations, for example, bloods, electrocardiogram (ECG), urinalysis, mobility needs.
- if known, original do not attempt cardiopulmonary resuscitation (DNA CPR), recommended summary plan for emergency care and treatment (ReSPECT), advanced statements (original or a copy of) that the patient has in place.
- details of current medication and any allergies
- contact details of family or carer to be informed of the admission and any caring responsibilities highlighted
- whether the patient is already known to service (this will allow the ward colleagues to gain further detail from the patient’s electronic record)
- confirmation that the admitting professional has informed the patient that we operate smoke free sites
- any relevant historical information
- information about who has been or still needs to be informed of the admission. Where possible the admitting professional will inform the relevant people of the plan to admit as part of their assessment and immediate care duties; This may include family members; home care agencies who may be due to visit; the care-coordinator; general practitioner et cetera. A good handover and communication of this information enable the ward colleagues to then take over this area of responsibility as required
If the patient’s first language is not English and, or any specific communication needs have been identified, for example, the requirement for a British Sign Language (BSL) interpreter, the ward colleagues should be informed of this so that arrangements can be made for an interpreter to be available at the earliest opportunity, please see interpreters policy (provision, access and use of, for patients, service users and carers).
4.2.3.7 Admission to hospital
4.2.3.7.1 What a patient should expect during their stay in hospital
During their stay in hospital patients should expect to have their privacy, dignity and confidentiality respected and to be treated in a holistic person-centred manner.
Interventions should be purposeful and carried out with the patients consent where possible or under an appropriate legal framework.
Colleagues will start to build therapeutic relationships as early as possible to:
- ensure the person feels supported and is an active participant in their care
- encourage the person to engage with treatment and recovery programmes
- collaborative decision-making
- create a safe, contained environment
- reduce the risk of suicide, which is increased during the first 7 days after admission
Communication between the multidisciplinary team should take place in a timely way to ensure care is streamlined and in most cases, recovery focussed, with the aim being towards successful discharge.
4.2.3.7.2 Orientation and information
On admission to the ward, patients will be welcomed by colleagues and shown around the ward being introduced to the various colleagues and other patients. The patient will be offered refreshments and addressed using the name and title they prefer.
Patients and carers will be asked to wait where they most feel comfortable before the admission clerking process begins (subject to risk assessment and staffing levels).
Patients will be provided with the name of the doctor under whom they have been admitted and when they are likely to see the person who will be managing their care.
At the earliest opportunity, the admitting team should provide the patient and their family, carer, or advocate with an opportunity to discuss their care. Discussions should be documented on SystmOne and cover:
- place of care and reason for admission to hospital
- daily routines (including the use of medicines and equipment)
- mealtimes and menu choices and meaningful activities available including timetables
- any visiting times or arrangements
- any restrictions they may be subject to whilst on the ward including the mental health units (use of force) policy
- any known risks including safeguarding and any additional support required.
- an explanation of confidentiality, its limits, and patient preferences for sharing information with third parties
- advance statements or advance decisions to refuse treatment (ADRT) in place
- what contingency plans may be required
- end-of-life care wishes where relevant
- any lasting powers of attorney for health and welfare or deputyship
On admission patients will be offered access to independent advocacy services that will take into account their language, communication, cultural, social needs and protected characteristics.
Consideration should also be given to identify whether there is a need for reasonable adjustments to be made to accommodate the patient in hospital. This is in line with the Equalities Act (2010). Examples include:
- providing communication aids (this might include an interpreter)
- ensuring there is enough space around the bed for wheelchair users to move from their bed to their chair
- single sex accommodation
- support for cognitive difficulties
Patients will be supported with their cultural and spiritual needs including meals, access to faith book or materials, a faith room and support from chaplaincy where appropriate.
Patients should be given accessible written information which colleagues talk through with them as soon as is practically possible.
The information includes:
- their rights regarding admission and consent to treatment
- rights under the Mental Health Act including right to appeal
- how to access independent advocacy services
- how to access a second opinion
- interpreting services
- how to view their records
- how to raise concerns, complaints and give compliments
- the identified contact or link person for each agency involved with their care
Patients will know who the key people are in their team and how to contact them if they have any questions. Patients will also be informed of the colleagues who is their first point of contact for each shift.
4.2.3.7.3 Other considerations
On admission the following is given consideration:
- the security of the patient’s home
- arrangements for dependants (children, people they are caring for)
- arrangements for pets
- benefits
- essential maintenance of home and garden
4.2.3.7.4 Action on patient’s arrival in the ward or as soon as practicable
Please refer to appendix D, the nursing admission checklist which details all actions to be completed on and within 72 hours of admission to hospital.
- The admitting nurse will contact the ward doctor if admission takes place between Monday to Friday 9am to 5pm, otherwise contact the on-call doctor to notify them of the patient’s arrival on the ward and agree who will be completing which sections of the admission assessment. It is the responsibility of the ward doctor or on-call doctor to clerk the patient in and undertake the physical health and wellbeing assessment. Please see physical health policy.
- Initial admission tasks to be completed by ward colleagues using the Inpatient launchpad on SystmOne. In the event that any of these cannot be fully completed a note is to be made as to the reason why and arrangements made for their completion the next day in line with local arrangements, for example, handover documentation, diarise, and no later than 72 hours following admission.
4.2.3.7.5 Admission care plan
- All patients will have a 72-hour admission care plan to meet their immediate needs and risks, taking into account the patient’s orientation to the ward and detailing their observation status. All colleagues involved in the patient’s admission need to be mindful of the fact that admission to hospital can lead to an increase in the level of stress or distress being experienced by the patient and that the provision of timely information and support can help to alleviate this. However, colleagues should take a thoughtful and sensitive approach to the patient’s presenting needs and whilst some aspects of the admission are to be completed immediately others may be completed as soon as is clinically appropriate.
4.2.3.7.6 Purposeful inpatient admission (PIPA)
- In order to ensure effective, safe, and therapeutic patient-focused care our inpatient wards are implementing the components of purposeful inpatient admission (PIPA). One of the first steps of purposeful inpatient admission is for there to be a clear reason for admission as agreed by the admitting professional, the clinical team, the patient and their carers where consent is given, therefore this to be documented as part of the admissions care plan.
- Where other needs and risks have been identified at the point of admission, associated care plans are also to be put in place. Where possible all care plans are to be formulated in conjunction with the patient and signed by them. The patient is to be offered copies of their care plans, colleagues to ensure that the relevant template on SystmOne is completed. If the patient declines or is not well enough to be involved in the development of their care plans a record of this is to be made in the electronic patient record.
4.2.3.7.7 Restrictions
Ward colleagues and the multidisciplinary team (MDT) will ensure that any restrictions including restrictions on access to personal possessions are necessary and proportionate in relation to the patient concerned, take into consideration the safety of the patient and others on the ward, are explained clearly to ensure the person understands, why the restrictions are in place and under what circumstances they will be changed.
4.2.3.7.8 Discharge planning
Discharge planning will commence at the point of admission in collaboration with a range of multi agencies, multidisciplinary team disciplines, the patient and the patients’ relatives and carers and, or advocate (where consent is given) throughout their stay.
Within 72 hours of admission all patients will have a discharge care plan. This will detail follow-up arrangements by the service or after care arrangements, including prioritising follow up within 48 hours of discharge for patients who presented with a risk of suicide during their inpatient stay.
4.2.3.8 Mental health assessment
On admission to hospital all patients will have a comprehensive mental health assessment and review utilising the local multidisciplinary team processes. This assessment will be started within 4 hours of admission, and the standard is for the initial assessments to be completed within 1 week or prior to discharge.
This assessment will be undertaken by the multidisciplinary team and consider the patients:
- mental health and medication
- psychosocial and psychological needs
- strengths and areas for development
The outcomes of initial mental health assessments should be shared with the patient and carer (providing patient consent has been given).
4.2.3.9 Physical health
All patients will have a comprehensive physical health review which will be started within 4 hours of admission or as soon as is practicable possible. The assessment is completed within 1 week or prior to discharge.
This review will include details of past medical history including any:
- long-term conditions
- current medication, including side effects and adherence
- details of past family medical history
- a review of physical health symptoms and a targeted systems review
- lifestyle factors, for example:
- sleeping patterns
- diet
- smoking
- exercise
- sexual activity
- drug and alcohol use
- consideration of whether the patient is at risk of withdrawal from drugs or alcohol
- physical observations including:
- blood pressure
- heart rate
- temperature
- weight
- height (abdominal circumference where indicated)
- respiratory rate
Where applicable a falls risk assessment to be completed to highlight falls prevention needs and the associated strategies to be put in place immediately. Colleagues should also inform the ward physiotherapist of the admission. Note that a hospital admission is a recognised falls risk in itself; as the patient is in an unfamiliar environment with unfamiliar routines at a time when they require increased help and support. Please refer to the patient falls manual (prevention and management) for more detail.
Arrangements to be made for any special or immediate associated provision, for example, sourcing of specialist equipment or aids or wheelchairs etc.
Wherever possible, patients will be offered a colleague of the same gender as them, and, or a chaperone of the same gender, for physical examinations. For any consultation, examination, procedure, treatment or care that is of an intimate nature, a chaperone should be offered. Obvious examples of an intimate examination include examination of the breasts, genitalia and the rectum. The patient should be given the opportunity to state their preferences in relation to the sex of the chaperone. This must be documented in their health records.
Patients will be informed of the outcome of their physical health assessment, and this will be recorded in their notes. With patient consent this can also be shared with their carer.
Patients will be offered personalised healthy lifestyle interventions such as advice on healthy eating, physical activity and access to smoking cessation services. This will be documented in their care plan.
Reiterate to any patients identifying as smokers, that the trust is a smoke free site and nicotine replacement therapy (NRT) to be offered as soon as possible to help keep them comfortable and minimise the effects of nicotine withdrawal. If an in-house smoking cessation service is available, the referral should be made within 24 hours of admission. If there is no established internal smoking cessation service in place, smokers should be provided with nicotine replacement therapy and e-cigarettes free of charge throughout of the duration of their in-patient stay and referred to the community smoking cessation services on discharge. Please see the smoke free policy.
Where concerns about physical health are identified during their admission, patients will have follow-up investigations and treatment. These investigations will be undertaken promptly and a named individual responsible for follow-up. Advice will be sought from primary or secondary physical healthcare services as necessary.
Where the patient is found to have a physical condition which may increase their risk of collapse or injury during restraint or the delivery of other aspects of their care, this is to be:
- clearly documented in their records
- regularly reviewed
- communicated to all multidisciplinary members;
- evaluated with them and, where appropriate, their carer or advocate
- discussed with the Reducing Restrictive Interventions team
There should be a care plan for any newly identified or pre-existing medical condition or problem where assistance or supervision from colleagues is required.
4.2.3.10 Risk assessment and management
4.2.3.10.1 Functional analysis of care environments (FACE) risk assessment
All patients will have a functional analysis of care environments (FACE) risk assessment and management plan which is reviewed and updated regularly (in response to significant clinical or risk changes and in keeping with minimum frequency outlined in RAG tool) and shared where necessary with relevant agencies (with consideration of confidentiality). The assessment will consider risks to self, risk to others, neglect, and risk from others.
All colleagues to be aware that the risk of suicide is increased during the first 7 days after admission. Where possible the functional analysis of care environments (FACE) risk assessment will be coproduced and include risk to carers and incorporate carers’ views on risk where necessary.
4.2.3.10.2 Red, amber, green (RAG) rating
All new patients are to be red, amber, green (RAG) rated as red. This rating will remain in place until at least the review at 72 hours or the patient’s first multidisciplinary team review (comprising multidisciplinary team discussion and face to face patient review).
4.2.3.11 Named nurse responsibilities
All patients admitted to the ward will have an allocated named nurse who is responsible for the coordination of their care and liaising with other agencies, family, and carers during the patient’s stay. The allocated named nurse should be on duty within 24 hours of the patient’s admission and should not be imminently due to take any annual leave or other planned absence of more than two days from the ward where possible.
At the first meeting with the patient, the admitting or named nurse where appropriate will:
- introduce and explain their role
- inform the patient of their right to be involved in decisions about their care and treatment and explain how to achieve this, including how to engage the services of an advocate
- determine what level of contact the patient wishes to have with their relatives or carers and what information they wish to be shared in relation to their care and treatment whilst an inpatient. This is to be documented in the records
- if the patient refuses to give consent for any information to be shared, the named nurse will explain that such a refusal will not prevent discussion taking place to enable relatives or carers from sharing information or any concerns with colleagues
- ascertain if the patient has any responsibility for the care of a child or other person. If yes, the named nurse will work with admitting professional or other agencies, friends or family to ensure that safe alternative arrangements are in place for the duration of the admission
- check that the patient’s admission and related assessments (see above) are complete
- review the patient’s care plans with them
- provide them with a copy of the named nurse leaflet (see appendix E)
During the admission, the named nurse will:
- actively engage both the patient and their relatives or carers and be the main conduit for information both to and from multidisciplinary team
- liaise with the allocated care coordinator or lead professional throughout the inpatient stay if already known to a community team
- take on the functions of the care coordinator under care programme approach or equivalent for patients not previous known to community mental health teams until a care coordinator is appointed or the patient is discharged
- ensure all care plans have review dates timed to suit individual needs of the patient which are the minimum timeframe for review of care plans
- review care plans as a minimum at the review dates stipulated and whenever there is a significant change in clinical presentation or social circumstances and at any transition of care (for example, transfer or discharge)
- provide the patient with copies of their care plan
- offer to meet with the patient for named nurse 1-to-1 sessions of least one hour per week. Sessions declined should be recorded in the records
- review functional analysis of care environments (FACE) risk assessments at the minimum agreed time intervals and in the event of a significant change to risk or clinical presentation or planning of leave
- monitor treatment compliance and response to medication and report any side effects
4.2.3.12 Positive behaviour support (PBS) and crisis plan
During admission ward colleagues will discuss with the patient any strategies for coping that they use and how they can continue to use, adapt, and develop positive coping strategies whilst on the ward.
Based on a risk assessment as well as observation of a patient for any behaviour which may indicate that there is a heightened risk of violence, aggression or abuse, individual care plans including positive behavioural support (PBS) plan if required should be developed.
The positive behaviour support (PBS) plan should include any identified or known triggers for these behaviours, actions to be taken should any of these occur, and any known physical health conditions that may be exacerbated by restrictive interventions and may impact on the post incident physical health monitoring.
The behaviour support plan must detail the responses such as de-escalation techniques, distraction, diversion and sometimes disengagement to be used by colleagues when a person starts to become anxious, aroused or distressed (secondary preventative strategies).
Any person who can reasonably be predicted to be at risk of being exposed to restrictive interventions must have an individualised behaviour support plan.
A crisis plan should also be developed as part of the care planning process and should include:
- relapse indicators and plans
- who to contact in a crisis
- coping strategies
- preferences for treatment and specific interventions
- advance decision to refuse treatment (ADRT)
4.2.3.13 Care programme approach (CPA) and care planning
All patients admitted to adult and older person’s mental health inpatient wards will be recorded as being on care programme approach or equivalent. Where a decision has been made to remove care programme approach during an admission this must occur after a multidisciplinary team review with clearly documented reasoning.
There will be a documented care programme approach (or equivalent) or admission review meeting within 72 hours (where practicable) of the patient’s admission. Patients are supported to attend this with advanced preparation and feedback. Any form of meeting discussing and reviewing any aspect of patient care must be documented in the records.
Every patient will have a written care plan, reflecting their individual needs. Colleagues collaborate with patients and their carers (with patient consent) when developing the care plan and they are offered a copy:
The care plan will clearly outline:
- agreed intervention strategies for physical and mental health
- Mental Health Act status
- measurable goals and outcomes
- strategies for self-management
- any advance statement or advance decision to refuse treatment (ADRT) the patient has made
- crisis and contingency plans
- review dates and discharge framework
Patients will be supported to be active participants in the planning and management of their own health and wellbeing. Each patient will have a personalised care and support plan that:
- captures and records conversations, decisions and agreed
- outcomes in a way that makes sense to the person
- is proportionate, flexible and coordinated and adaptable to a person’s health condition, situation and care and support needs
- includes a description of the person, what matters to them and all the necessary elements that would make the plan achievable and effective
The Community Mental Health Framework for Adults and Older Adults (NHS England, 2019) and related guidance is applied when planning and coordinating care with community providers.
All patients will have a documented diagnosis and a clinical formulation which is jointly constructed by the patient.
This formulation will include the presenting problem and predisposing, precipitating, perpetuating, and protective factors as appropriate. Where a complete assessment is not in place, a working diagnosis and a preliminary formulation is devised.
It is good practice for any patients who are known to have been under the care of another mental health provider for colleagues to make a request through the trust information governance department for copies of the clinical records to be forwarded to the ward so that they can be reviewed to inform decision-making around future care and treatment.
4.2.3.14 Care planning when patients decline or lack the capacity to involved
Should a patient decide not to be involved in their care planning, or if they have been assessed as lacking the capacity to be involved in their care planning this should be documented in the patients record at the time with a clear rationale for the decision-making around this.
A person’s capacity and level of engagement can change and fluctuate throughout their hospital stay, so colleagues should continue to make attempts to engage and involve the patient in the care planning process. Colleagues should document each time that attempts are made and the outcome.
See Mental Capacity Act (2005) policy for further information.
4.2.3.15 Medicines management on admission
The admitting nurse will ask the patient if they have brought any of their prescription medications with them. If yes, they are to be removed and stored in the treatment room, so that the doctor can check the prescription as part of the medicine reconciliation process and prescribe on SystmOne.
All patients who are admitted must have their medicines reconciliation and allergy status completed and documented within 24 hours or as soon as access to the primary care record is available, in line with National Institute for Health and Care Excellence (NICE) guidance and the safe and secure handling of medicines manual. Upon completion, this should be indicated in the electronic patient record. Colleagues should understand what the patient is prescribed and what they are taking including medication which may not be prescribed. Consideration should be given to reviewing medication and any changes should be clearly documented with a clear rationale provided. See safe and secure handling of medicines manual for further information.
When medication is prescribed, assessment of capacity and consent are recorded by the consultant or clinician in charge in accordance with trust policy on the relevant system template.
For detained patients, an assessment of capacity to consent to prescribed psychiatric and physical health medication must be completed and recorded within at least 7 days following admission under the Mental Health Act (or within 7 days of detention if informal on admission).
4.2.3.16 Patient identification
Patient identification can be undertaken in a number of ways, and these are clearly set out in the patient identification policy.
In the event that a patient is admitted with the same or a similar name to an existing patient an alert to this effect is to be placed on the electronic patient record of both patients.
4.2.3.17 Communication and support for carers
The named nurse will contact family or carers within the first 48 hours of admission to discuss concerns, family history and their own needs. A face-to-face meeting can be facilitated on request where appropriate.
Colleagues should be aware, when consent has not been given for sharing information with carers or relatives, there may be situations when they can share general information about things that the carer or relative already knows; for more guidance see common sense confidentiality video on YouTube.
If not already done the carers are to be asked if they wish to be referred for a statutory carers’ assessment in line with the Care Act (2014). If yes, the referral will be made by the ward colleagues. Ensure a carers assessment has been offered, or started, before the person is discharged from hospital
4.2.3.18 Do not attempt cardiopulmonary resuscitation (DNACPR), recommended summary plan for emergency care and treatment (ReSPECT), advance decisions or statements
Patients who have had previous involvement with the mental health services may have made an advance statement and an advance decision to refuse treatment (ADRT) determining their wishes in-respect of the care and treatment should they require inpatient care. These decisions can be made by the patient and, or anyone else that may have legal authority, for example, lasting power of attorney or court appointed deputy.
Colleagues should refer to the trust’s advance statements and advance decisions to refuse treatment policy for full details and check both with the patient or carers of any advanced statement or advanced decision and SystmOne for any record of an advance statement or advanced decision.
4.2.3.19 Planned admissions
Prior to a planned admission there should be a multi-professional discussion regarding the rationale and outcomes expected from the admission. The gatekeeping process outlined in section 4.2.5 will be followed.
For planned admissions, patients will be offered an opportunity to visit the inpatient unit before they are admitted. If this is not possible, consider using accessible online and printed information including photographs of the unit to support discussion about their admission.
If admission is being planned for a treatment episode involve the person who is being admitted, their family members, parents or carers, community accommodation and support providers.
When planning treatment for patients being admitted, take account of the expertise and knowledge of the person’s family members, parents, or carers.
Allow more time and expert input to support people with complex, multiple or specific support needs to make transitions to and from services, if necessary.
This may include:
- children and young people
- people with dementia, cognitive or sensory impairment
- people with neurodiverse conditions, for example:
- attention deficit hyperactivity disorder (ADHD)
- autism
- dyspraxia
- dyslexia
- dyscalculia
- dysgraphia
- Tourette’s syndrome
- people with learning disabilities and other additional needs people placed outside the area in which they live
To support the person’s transition to the ward, the admitting nurse or person responsible should make the following items available if the person needs them: a toothbrush, hygiene products and nightwear. This is particularly important for people who have been admitted in crisis.
4.2.3.20 Contingencies
4.2.3.20.1 Specific requirements for patients admitted who are subject to detention under the Mental Health Act (1983)
Colleagues should refer to the Receipt and scrutiny of detention papers Mental Health Act (1983) policy and section 132 informing detained patients of their legal rights procedure for full details.
4.2.3.20.2 Prisoners not detained under the Mental Health Act or those detained by the police
When a prisoner or person lawfully detained by the police, UK Border Agency or national security services is admitted to an inpatient unit, (other than forensic services) then the relevant modern matron or service manager, Safety team and associate nurse director are to be informed as soon as reasonably practicable, preferably within one working day.
A risk assessment is to be carried out in conjunction with the detaining authority (prison, police) which includes the potential risk to others, specific risks to colleagues, the presence of detaining authority guards, the use of mechanical restraints, restricting access to areas other than the bed area or room, and to ascertain the required action if the person attempts to leave the ward or department.
For mechanically restrained persons (prisoners in chains), an agreement between the detaining authority and the ward or department on the use of restraints, including when they are used, is to be documented in the care record.
Ideally the person will be accommodated in a single room rather than multiple occupancy room; this will reduce anxiety of other patients, improve privacy for the person and make security management easier. Seclusion is not to be used for this purpose unless the clinical presentation indicates that seclusion would be a viable clinical intervention.
The detaining authority (if necessary, their medical department) are to be included in all discharge planning prior to discharge to ensure suitable arrangements are made.
4.2.3.20.3 Patients requiring admission to or consideration for a psychiatric intensive care physical environment (PICU) environment
The multidisciplinary team on receipt of the referral form will make decisions regarding the suitability of the patient admission or transfer. The multidisciplinary team may decline to accept patients if they anticipate that the patient mix will comprise safety and, or therapeutic activity. This decision to accept or decline patients will be based on a clear clinical rationale based on risk assessment and alternative care options will be identified if the referral is declined. The decision will be recorded on the referral form and on SystmOne. Psychiatric intensive care physical environment referral form (staff access only) and psychiatric intensive care physical environment referral flow chart (staff accesS only).
4.2.3.20.4 Request from another trust to utilise an adult and older person’s mental health inpatient bed
If another trust is asking to use one of our in-patient beds, this must be approved by the Patient Flow team (within working hours) and the bronze on-call manager outside these times.
4.2.3.20.5 Patients who are homeless or at risk of being homeless
Patients, who have recently been homeless, or who are at risk of being made homeless, should be identified as soon as possible on or before admission, so that the appropriate agencies in both health and social care can be involved at an early stage. This will ensure that appropriate and timely needs assessments have been actioned to develop a discharge plan proportionate to individual need. If for any reason it has not been possible to secure appropriate accommodation and the patient is no longer requiring an inpatient bed, the patient is to be directed to either the:
- Citizen’s Advice Bureau
- Local Authority Housing Department Crisis Accommodation team
For any homeless patient subject to care programme approach there must be explicit plans in place to maintain contact and enable the 72-hour follow-up to take place before they leave the ward.
4.3 Safe discharge or transfer of patients from adult and older persons mental health service inpatient wards procedure
4.3.1 Aim
Safe, effective, and timely discharge from the adult and older persons mental health service inpatient wards is a shared responsibility between the Rotherham Doncaster and South Humber Trust and other service providers, and discharge planning should begin as soon as a patient is admitted to hospital.
However, it is important that any transfer between, or discharge from a service is not viewed by clinical colleagues as an isolated event as it is only one component of the patient’s care pathway, and as far as possible be seen as one seamless and integrated process. To not view it in this way can result in patients experiencing a disjointed, delayed, or unsatisfactory episode of inpatient care.
The aim of this procedure is to provide colleagues working within the adult and older persons mental health in-patient services clear guidance on how to safely manage the discharge and, or transfer of patients.
4.3.2 Scope
The contents of this procedure only apply to clinical colleagues working across the adult and older person’s mental health inpatient services.
4.3.4 Procedure
Discharge planning will commence at the point of admission in collaboration with a range of multi agencies, multidisciplinary team (MDT) disciplines, the patient and the patients’ relatives and carers and, or advocate (where consent is given) throughout their stay.
The discharge of any patient from the inpatient services will be a planned event which only takes place after full consultation with all the relevant people involved in the patient’s care (including where consent is given with relatives, carers and, or their advocate). Discharge planning will be collaborative, person-centred, and suitably placed, so that the patient does not feel their discharge is sudden or premature.
As there could be any number of circumstances which make the discharge of a particular patient more complex, the following guidance is not exhaustive and will need to be adapted to meet the needs of each individual patient.
4.3.4.1 Action on admission
- On admission the patient, and where appropriate their family, carer and, or advocate will be advised of the purpose of admission and the means by which they will be involved in the discharge planning process.
- Within 72 hours of admission the multidisciplinary team will review the admission assessment, consider the patients’ needs (short and long term) and commence the discharge care plan to meet the needs of the patient. The discharge care plan will identify if the patient is to be discharged home or to an alternative care setting where applicable. Relevant community mental health services (CMHS) will also engage in planned multidisciplinary team meetings (ward rounds) and other planning arenas.
- To ensure the inpatient admission is focussed on active treatment and supports timely discharge, within 72 hours the multidisciplinary team will identify and record in the electronic patient record (EPR) the estimated date of discharge (EDD). These decisions will be reviewed, and both the discharge care plan and estimated date of discharge updated throughout the patient’s stay.
4.3.4.2 Discharge and crisis care planning
Within 72 hours of admission all patients will have a discharge care plan. This will detail follow-up arrangements by the service or after care arrangements, including prioritising follow-up within 48 hours of discharge for patients who presented with a risk of suicide during their inpatient stay.
As a minimum the discharge care plan should include:
- the plans that are in place to manage any identified risk. Including the heightened risk of suicide in the first three months following discharge
- possible relapse signs
- the arrangements for promoting the patients ongoing recovery and engagement with service support
- actions to be taken by patient or carer in the event of deterioration
- who to contact
- where to go in a crisis or emergency
- budgeting and benefits
- handling personal budgets (if applicable)
- social networks
- educational, work related and social activities
- details of medication including any monitoring arrangements
- details of treatment and support plan
- physical healthcare needs including health promotion and information about contraception (where applicable)
- date of review of the care plan
- explicit plans for how the service will respond in the event of the patient becoming non-compliant or disengaging with the service
A determination should be made as early as possible in discharge planning about the status and views of any carers who provide care, including that they are willing and able to do so. This will need to be age appropriate if this is a young carer under the age of 18.
Before discharge, the multidisciplinary team should consider and offer a series of individualised psychoeducation sessions to promote learning and awareness.
Sessions should:
- start while the person is in hospital
- be conducted by the same practitioner throughout if possible
- continue after discharge, so the person can test new approaches in the community
And cover:
- symptoms and their causes
- what might cause the person to relapse, and how that can be prevented
- psychological treatment
- coping strategies to help the person if they become distressed
- risk factors
- how the person can be helped to look after themselves
- phased leave (the patient can have trial periods out of hospital before discharge) with support where necessary (consider community mental health team, home treatment)
- phased return to employment or education
- This is important for people who have been in hospital for an extended period and who have had restricted access to the community
During discharge planning multidisciplinary teams also need to consider group psychoeducation support for carers this should include signposting to information on the specific condition of the person they care for.
People in hospital should be supported to participate actively in making informed choices about their care, including, for people who fund their own care, the potential longer-term financial impact of different care options after discharge. These conversations should begin early in a hospital stay, and not when a person is ready to be discharged. This should also include, where appropriate, information about housing options (adaptation of the existing home and possible alternative housing, for example supported living).
On discharge from hospital people who have new or additional needs should be offered of onward care and support to aid their recovery. The choices available should be suitable for their short-term recovery needs and available at the time of discharge.
Where the patient is discharged to a community team the discharge care plan should be reviewed by the care coordinator or lead professional within one month of the patient’s discharge.
4.3.4.3 Discharge assessment criteria and record keeping
The assessment criteria to determine the patient’s fitness for discharge are:
- a clinical decision has been made that a patient is ready for discharge
- a multidisciplinary team decision has been made that the patient is ready for discharge
- the patient is safe to discharge
Multidisciplinary team (MDT) in this context includes nursing and other health and social care professionals. It is acknowledged that circumstances of discharge will vary, and the multidisciplinary team should consider the individual circumstances of the patient when determining if the discharge is delayed. This determination should consider the following factors against each of the criteria.
Once the multidisciplinary team have made the decision that the patient is fit for discharge or transfer this will be documented in the electronic patient record (EPR).
At a time when the clinical decision has been made that the patient is ready for discharge the multidisciplinary team or ward round will discuss plans for aftercare and ensure an appropriate package of care is in place and agreed with consideration of the patient’s consent and capacity.
If a person’s preferred care placement or package is not available once they are clinically ready for discharge, an available alternative, or alternatives appropriate for their short-term recovery needs should be offered, while they await availability of their preferred choice. People do not have the right to remain in a hospital bed if they no longer require acute care, including to wait for their preferred option to become available.
Where the person is assessed to lack capacity to make the specific decision or there is dispute between the clinical team and the patient’s family regarding capacity, a best interest’s decision should be made in line with the Mental Capacity Act (2005) policy and recorded on the relevant templates in the electronic patient record (EPR).
Where an individual wishes to return home and their family member or unpaid carer is unwilling or unable to provide the care needed, NHS bodies, local authorities and care providers should work together to assess and provide the appropriate health and care provision required to facilitate the individual’s choice, where possible, and enable a safe discharge.
Where there is disagreement between a person and their unpaid carers or family members, and the person is deemed by the appropriate professional to have capacity to make decisions relevant to their discharge, the person’s right to make these decisions should be respected. If the person or their family are objecting to the proposed discharge especially, where they involve a change of residence then consideration will be needed whether the matter needs to be referred to the Court of Protection. Advice should be sought from the Mental Capacity Act lead.
4.3.4.4 Risk assessment
Prior to discharge a thorough assessment of the patient’s personal, social, safety and practical needs to reduce the risk of suicide on discharge must be undertaken with the aid of the functional analysis of care environments (FACE) clinical risk assessment tool. This must take into account:
- any change in the risk profile once the patient is discharged from the ward
- the setting the patient is being discharged to
- patient engagement
- carer involvement (if the patient agrees)
- the possibility of using a personal health or social care budget and ensure the person understands about charges for social care
- aftercare support, in line with section 117 of the Mental Health Act (1983)
- aspects of the person’s life including:
- daytime activities such as employment, education, and leisure
- food, transport, budgeting, and benefits
- pre-existing family and social issues and stressors that may have triggered the person’s admission
- ways in which the person can manage their own condition
- suitability of accommodation
- risks to children
- risks to the patient from others due to their vulnerability
- risk of domestic abuse
This is undertaken and reviewed by the multidisciplinary team in the discharge meeting. Where timeframes do not allow for this, for example, when a patient requests discharge at short notice, it will be the responsibility of the nurse in charge of the ward at the time to complete the review of the clinical risk assessment.
The management of any identified risks will be included in the discharge care plan.
4.3.4.5 Pre discharge meetings
A pre-discharge meeting must be organised by the named nurse in liaison with the nominated community-based care co-ordinator or lead professional where applicable. This meeting should include the patient, carers (where patient consent has been given) and all members of the multidisciplinary team involved in the inpatient care, as well as the nominated community-based care co-ordinator or lead professional, family, carer and, or advocate where appropriate and will be recorded electronically in the form of a care programme approach review summary (or equivalent).
The following will be agreed at the meeting:
- care programme approach status or equivalent (all inpatients are automatically placed on care programme approach, any decision to remove care programme approach must be documented with a clear rationale from the multidisciplinary team in the electronic patient record)
- follow-up requirements, either a minimum of 48 hours (for patients identified having a risk of suicide on preparation for discharge) or 72 hours including location, date, time and by whom, see appendix U, 72 hours follow-up technical guide for further information
- current clinical risks including a review and update of the functional analysis of care environments (FACE) risk assessment
- eligibility for section 117 aftercare including any provision for aftercare services required or in place colleagues should refer to trust section 117 Mental Health Act (1983) policy for further guidance
- details of carers and offer of carer’s assessment if one has not already been offered
- identification of any unmet needs
- crisis and contingency plans
- any required support around administration of medication or management of side effects
- use of personal budgets to support identified social care needs
- any aftercare arrangements agreed with other services (for example, substance misuse, older adults or learning disability services)
- any transport requirements which may be required
- referral to the home treatment team
At this meeting it will be ascertained if the patient will require a statement of fitness for work (form med 3 is required) and if so, arrangements made for the doctor to complete one. The patient will be given a copy of the discharge pack and the discussion and agreement from the pre-discharge meeting will be recorded in the patient’s electronic patient record, and a discharge care plan formulated which will include all agreed actions. The nurse who was present in the pre-discharge meeting will arrange for a prescriber to order any prescribed take home medication to ensure that it will be on the ward ready for when the patient leaves.
4.3.4.6 A clinical decision has been made that a patient is ready for discharge
A patient is medically ready to be discharged when, as at 8am that morning, they meet all of the following three criteria.
No further interventions are needed that can only be carried out in an inpatient setting. The person could be assessed, cared for, and treated in their home or less restrictive setting.
The multidisciplinary team have concluded that the person is medically fit and ready for discharge. The multidisciplinary team should include parties external to the trust, for example social care colleagues. This step involves considering issues such as housing, family or carer needs and the support available in the community, to decide whether discharge would be appropriate. When deciding whether someone is ready for discharge, members of the multidisciplinary team should explicitly consider the person and their family or carers’ views about whether the person feels ready for discharge and engage with them about the proposed discharge plan.
This criterion is likely to be met when:
- the multidisciplinary team responsible for the care and treatment in hospital has agreed that the patient no longer requires an inpatient bed to meet their continuing health need
- the multidisciplinary team has recorded a consensus decision that inpatient stay is no longer required to meet the patient’s continuing health need
- an appropriate level of care (including accommodation with care) required to meet the patient’s needs has been defined
- an adequate person-centred discharge plan has been agreed with the person to carry on any necessary assessments, care, and treatment in the community. The plan should provide clear information about the proposed discharge process and enable the person and their family or carers to shape decisions about discharge. Medically fit does not indicate complete recovery, instead it is the point at which the person could be safely assessed, cared for, and treated in their home or less restrictive setting. It is important that all three criteria are met rather than only one or two. Being medically ready for discharge does not mean that patients should be rushed to be discharged if the conditions are not in place to continue their recovery outside of hospital. Rather it is an indication that the person could continue their recovery outside of hospital were the adequate support or services in place
This criterion is likely to be met when:
- an aftercare plan has been determined which will maintain the patient’s safety
- the patient no longer requires an inpatient stay to maintain basic safety
- the defined aftercare plan is assessed as appropriate to maintain safety
All medically ready for discharge dates are to be recorded on the patient electronic record. Once a patient meets all three of the above criteria but cannot be discharged that day, they become a delayed transfer of care (DToC), standards for recording and reporting Delayed transfers of care (staff access only) and expected date of discharge medically ready for discharge and delayed transfers of care SystmOne guidance (staff access only).
4.3.4.7 Recording of a delayed transfer of care
The NHS England 2018 Monthly Delayed Transfers of Care Situation Report, Principles, Definitions and Guidance define a delayed transfer of care (DToC) as follows:
“A delayed transfer of care from NHS-funded acute or non-acute care occurs when an adult (18 and over years) patient is ready to go home and is still occupying a bed. A patient is ready to go home when the criteria detailed in section 4.3.4.2 are met.”
A delayed transfer of care will be recorded on the patient electronic record when the patient is medically ready for discharge but unable to transfer due to external delays. See standards for recording and reporting delayed transfers of care (staff access only) and expected date of discharge medically ready for discharge and delayed transfers of care SystmOne guidance (staff access only).
4.3.4.7.1 Internal delayed transfer of care definition
An internal delayed transfer of care is when the patient is medically ready for discharge but unable to transfer due to an internal delay. This should not be recorded on SystmOne as a delayed transfer of care however it is good practice for clinical teams to discuss any internal delays in the weekly multi-disciplinary care group delayed transfer of care meetings and escalate to the Patient Flow team, as necessary.
4.3.4.7.2 Process
It is the responsibility of the multidisciplinary team to determine the estimated date of discharge, medically fit for discharge and delayed transfer of care, the nurse representative at the multidisciplinary team is responsible for ensuring the outcome of the discussion is recorded in the electronic patient record. The nurse may choose to delegate this task where appropriate but will remain responsible for ensuring the record is updated.
4.3.4.7.3 Monitoring
Patient flow and performance will carry out weekly reconciliations to verify the numbers of delayed transfer of care and other delays, comparing system recording with information shared at the weekly delayed transfer of care meetings, to ensure accuracy. This will be supported by other processes, for example audit, as needed.
4.3.4.8 Communication with carers
The engagement and active participation of carers as equal partners is central to the delivery of care and in the planning of a successful discharge. However, there may be times when a patient with capacity refuses to give consent for the sharing of any information about their care and treatment with their carers. In such a situation the patient’s decision is to be recorded under information sharing on the general information template in the electronic patient record (EPR). Colleagues must then revisit this decision with the patient at regular intervals throughout their stay on the ward.
The carer is to be informed of the patient’s wishes, but consideration must also be given to the fact that there is some information which can be shared without breaching patient confidentiality. In addition, if there are any risks posed to the carer the organisation may have a duty to keep the carer informed of the fact that the patient will be leaving the ward. If colleagues are unclear as to what can be shared, they should seek advice from the modern matron.
Before the person is discharged, the following must have happened subject to patient confidentiality and risk considerations outlined above:
- inform carers of the plans for discharge
- discuss with carers the person’s progress during their hospital stay and how ready they are for discharge
- ensure that carers know the likely date of discharge well in advance
- determine any change in carers’ circumstances since admission which may affect discharge planning
4.3.4.9 Medication management
Medicines management plays an important role in preparing patients and their carers for their discharge from hospital. Compliance with medication has an impact on a patient’s recovery and, or maintenance of their condition once they leave hospital.
An assessment of the patients’ ability to self-medicate must also be made. If the patent requires assistance on discharge this must be communicated to the appropriate health and social care professionals.
As part of this assessment the patient is to be provided with the relevant information leaflets in respect of the medication they are taking, and the most common side effects they may experience.
It must be made clear to the patient who to seek advice from should they experience any side effects which are causing them concern.
Any medication required by the patient on discharge from hospital should be requested from the pharmacy supplier at least 24 hours in advance.
The nurse in charge has the responsibility for ensuring that the patient understands the importance of the medication being taken to support concordance.
It is also important that patients are fully informed both verbally and in writing as to the medication they have been prescribed, when to take it, and where to go for advice or further supplies.
At discharge, patients will normally be provided with a 14-day supply of their medication. The exception to this is finishing off a course of medication or when required medication. In the case of patients who have a high risk of overdose, a decision may be made by the prescriber to provide the medication in smaller supplies. In this case it is important that the patient’s general practitioner is aware of this, and arrangements must be in place for the patient to collect their repeat prescriptions.
For any patient prescribed clozapine, they must be referred to clozapine clinic prior to discharge. Colleagues in the clinic must be informed of the proposed discharge date for the patient so that the next appointment can be booked within the correct timeframe and arrangements for clozapine prescriptions confirmed.
For any patient prescribed lithium, consideration must be given to the arrangements for ongoing monitoring in the community. In most cases this will be via the community lithium clinic (responsible for routine monitoring for stable treatment). Referrals must be made with sufficient notice and the following criteria met and information shared:
Criteria:
- stable dose of lithium established
- next bloods due in 3 months (if not, still refer but make arrangements for interim monitoring)
- information required for referral:
- brand and dose of lithium
- indication
- other medications prescribed
- relevant history, medical
- relevant risks, for example, compliance, medical, mental health
- date and results of last lithium monitoring bloods
For any patient prescribed an injectable antipsychotic (depot, long-acting injection) consideration must be given to arrangements for the ongoing administration and this must be agreed with plans in place at the point of discharge. The prescription must be available for the community prescriber to view on SystmOne including:
- the last administration date so that the next administration date is clear
- any side effects or problems at injection sites.
4.3.4.10 Information for patients
Patients who are being discharged from hospital have the right to be fully involved in the arrangements and should receive the following:
- full information regarding their diagnosis and assessment of their health and social needs, in preparation for discharge
- a copy of their discharge care plan
- a copy of the discharge pack which will include:
- information on the services available in the community relevant to their care, including voluntary organisations and support groups
- information on PALS and advocacy support
- a copy of the trust “your opinion counts form”
- contact names and numbers for help or advice post-discharge
- copy of the discharge notification
In addition, patients should be made aware of the fact that they have the right to receive copies of any correspondence issued by the service which relates to their care and treatment, and colleagues are to refer to the healthcare record keeping policy for full details and information for copying letters to service users.
4.3.4.11 Action on the day of discharge
On the day of discharge the nurse who is responsible for assisting the patient or overseeing them safely leaving the ward will:
- assess if there has been any change to the patient’s presentation or risk profile, any change should be discussed with the multidisciplinary team
- reconfirm follow-up arrangements if not made on the same day and provide the patient with a discharge card with the follow-up arrangements (including location, date, time and by whom) and name of relevant professionals and their contact number (for example, care coordinator), ward number and details of whom to contact in an emergency and how
- check dispensed take home medications against prescriptions to ensure correct medication and doses have been dispensed
- talk the patient and, or carers through the prescribed medication and how to obtain further supplies, answering any queries which they may have. Advice must also be given on whom the patient is to contact should they experience any side effects from their medication. If there is any concern identified in respect of the patient’s ability to manage their own medication the discharge is to be delayed whilst advice is sought from a member of the medical team
- return any personal belongings held in safe keeping to the patient and document return on SystmOne
- check if the patient needs a medical certificate, med 10 can be issued by a registered nurse or doctor and only covers the duration of their inpatient stay, med 3 can cover a further period of sick leave following discharge from an inpatient bed but can only be issued by a doctor
- check that patients have the means to access the property they are being discharged to or that someone will be there to receive them
- confirm any required transport arrangements are in place
- contact the care coordinator or team providing follow-up to confirm discharge has taken place if not present at a discharge meeting held on the same day
- notify other people or services that may need to be informed of the patient’s discharge if they are not already aware, for example, probation, public protection unit, the police etc. and document this in the clinical records
- once the patient has left the ward an entry to this effect will be made in the patient’s clinical record on the electronic patient record which will also confirm the actual time the patient left the ward, their destination, and any other relevant information. The ward bed status will then be updated
- if the person is subject to a deprivation of liberty authorisation the supervisory body should be informed of the changes and a Deprivation of Liberty Safeguards form 10 completed. If the request for authorisation has not yet been granted an email should be sent to the supervisory body to cancel the request. See Mental Capacity Act (2005) Deprivation of Liberty (DoL) policy for further guidance
Patients should be made aware that they have the right to receive copies of any correspondence issued by the service which relates to their care and treatment. Wishes to receive a copy of letters should be recorded in their clinical record.
Patients discharged from inpatient care have their care plan sent to everyone identified in the plan as involved in their ongoing care within 24 hours of discharge.
Any paper copies of the patient’s records are to be filed and forwarded to the ward clerk for scanning onto the electronic patient record or archived.
4.3.4.12 Transport arrangements
Most patients will make their own transport arrangements, but it is important that the nurse in charge checks that this is the case before the patient leaves the ward.
For patients who are being transferred to another service provider the nurse in charge of the ward will organise appropriate transport taking into account safe transportation of patients and staff (adult and older person’s mental health and learning disability).
- Clinical risk.
- Risk of violence, and, or absconding.
- Least restrictive methods to manage any identified risk.
- Size of transport required to accommodate both the patient and any escorting colleagues.
- Distance to the new provider.
If a patient is considered too high a risk for trust colleagues to safely escort the nurse in charge will speak to the modern matron about the need to employ a specialist transfer and escort company.
Colleagues should refer to the safe transportation of patients and staff (adult and older person’s mental health and learning disability) for full guidance. This guidance also includes the roles and responsibilities of the escorting colleagues.
4.3.4.13 72-hour follow-up
Prior to discharge a discussion will take place with the patient in relation to follow-up support post discharge. Support will be arranged according to their mental and physical health needs. This could include contact details, for example of:
- a community psychiatric nurse or social worker
- the out-of-hours service
- support and plans for the first week
- practical help if needed
- employment support
The inpatient team makes sure that follow-up arrangements (within 48 or 72 hours of discharge) are in place before patients are discharged from hospital. The patient is made aware of these arrangements, and they are documented on SystmOne. This includes location, date, time and by whom. This applies to all patients regardless of care programme approach status on discharge. All 72-hour follow-ups must be face to face unless there are significant exceptions such as patient refusal or non-engagement, removal from the country or transfer to another mental health inpatient facility.
Consideration should be given to contacting adults admitted for self-harm, who are not receiving treatment in the community after discharge, and providing advice on:
- services in the community that may be able to offer support or reassurance
- how to get in touch with them if they want to
The arrangements for 72-hour follow-up will be agreed at the pre-discharge meeting, and the trust information department has in place an automatic notification system to remind clinicians of all discharges and the latest date by which the 72-hour follow-up visit has to have taken place.
However, any patient who presented with a risk of suicide during their inpatient stay should be seen within 48 hours of discharge. If a face-to-face visit is not possible for any reason the care coordinator should arrange to contact them by phone.
4.3.5 Patients with additional or alternative needs
4.3.5.1 Patients who require specialist equipment or home adaptations
Any equipment and, or home adaptation requirements should be assessed in advance of discharge and arrangements put in place to secure delivery in alignment with the date of discharge.
If deemed appropriate by the multidisciplinary team a home visit may be arranged prior to discharge to assess and identify the patient’s induvial needs and requirements. The multidisciplinary team may wish to consider referrals to other agencies at this stage.
Prior to discharge, the patient and their carers should be trained in the use of any equipment. This may require the organisation of a home visit facilitated in conjunction with the provider of the equipment.
Follow-up arrangements with the appropriate service will be in place to check that the equipment and, or home adaptation provided is adequately meeting the patient’s needs and being used correctly.
The patient will be provided with information around how to report any fault with the equipment or to arrange its return once it is no longer needed.
4.3.5.2 Patients who require funding for specialist placements
The assessment for, and delivery of, continuing health and social care, is organised so that individuals understand the continuum of health and social care services, their rights and receive advice and information to enable them to make informed decisions about their future care. In situations where a patient does not have the capacity to make such decisions, it will be necessary to first ascertain if there are decision-making mechanisms in place within either the Mental Health Act (1983) or the Mental Capacity Act (2005).
Once it has been decided that the patient requires the funding of a specialist placement the named nurse will first complete the continuing care checklist to determine if the patient is eligible and, where applicable, complete the full decision support tool with support from the multidisciplinary team.
Any decision around the most appropriate placement to meet the patient identified needs will be made by the multidisciplinary team. The multidisciplinary team will also be responsible for approaching any identified placements and organising assessments and pricing.
For patients who are assessed as requiring an alternative care setting or enhanced care needs the relevant funding requests processes and subsequent documentation should be initiated with the respective local authority (LA) or integrated care boards (ICBs). Where section 117 is applicable a statement of need document (located on SystmOne) should be completed to support decision-making in respect of funding where a need is identified. If during the admission a new need arises an assessment should be undertaken as soon as practicable.
4.3.5.3 Patients being discharged into the community who have been identified as a significant risk to others or are known to undertake offending behaviour
If the patient is subject to multi-agency public protection arrangements (MAPPA) a MAPPA 1 is to be completed and submitted to the multi-agency public protection arrangement coordination unit. This is not a referral but gives the opportunity for the sharing of clinical information and the opportunity to request information from the police and probation services to inform decision-making. The completed forms are to be submitted to either the South Yorkshire or North Lincolnshire multi-agency public protection arrangement unit. Prior to the discharge of the patient a decision will need to be made whether a multi-agency public protection meeting needs to be held.
For patients not currently subject to multi-agency public protection arrangements a multi-agency public protection arrangement referral is to be completed and include the following information.
- Likelihood of the patient offending.
- The risk of serious harm including to whom and when.
- Who needs to be invited to the multi-agency public protection arrangement meeting.
- A copy of the patients’ clinical risk assessment.
- A copy of the risk management plan.
The referral also needs to demonstrate that there are specific risks which require inter agency involvement beyond that which is normally provided.
If a multi-agency public protection arrangement referral is made the patient is to remain on the ward as an inpatient until the referral has been processed and if deemed necessary, a strategy meeting should be held.
Colleagues should refer to the multi-agency protection panel arrangements page (staff access only) for further advice.
4.3.5.4 Patients who are homeless
Patients, who have recently been homeless, or who are at risk of being made homeless, should be identified as soon as possible on or before admission, so that the appropriate agencies in both health and social care can be involved at an early stage. This will ensure that appropriate and timely needs assessments have been actioned to develop a discharge plan proportionate to individual need. If for any reason it has not been possible to secure appropriate accommodation and the patient is no longer requiring an inpatient bed, the patient is to be directed to either the:
- Citizen’s advice Bureau
- Local Authority Housing Department Crisis Accommodation team
Any patient who needs to attend one of these departments to sort out accommodation is not to be discharged outside of normal working hours as they will not be open to offer advice to the patients.
For any homeless patient subject to care programme approach there must be explicit plans in place to maintain contact and enable the 72-hour follow-up to take place before they leave the ward.
4.3.5.5 Patients subject to community treatment orders
Colleagues should refer to the trust community treatment order policy for full guidance, however the general steps of application are as follows.
4.3.6 Communication
4.3.6.1 Discharge letters
A discharge notification will be completed within 24 hours by a member of the medical team on the approved template in the electronic patient record on SystmOne which contains the following information:
- date of admission
- date of discharge
- legal status of patient
- medication at discharge
- International Classification of disease 10 (ICD-10) diagnosis
- medication recommendations
- relevant physical findings or investigation results
- any known allergies
- details of any medication changes during admission
- circumstances of admission
- summary of admission
- identified risks including any infection risks
- follow-up arrangements
- care programme approach requirements
- details of community workers involved
4.3.6.2 Communication with general practice (GP)
At the point of admission and discharge the GP should be notified. Within 24 hours, a discharge letter (or interim discharge summary) is emailed to the person’s GP. A copy should be given to the person and, if appropriate, the community team and other specialist services.
A full or detailed discharge summary is sent within a week to the patient’s GP and others concerned (with the patient’s consent), including why the patient was admitted and how their condition has changed, diagnosis, medication, and formulation. Where relevant a copy of the do not attempt cardiopulmonary resuscitation (DNACPR) and recommended summary plan for emergency care and treatment (ReSPECT) form should also be included.
Guidance note: this should include relevant physical health information such as new diagnoses, new concerns, outcomes or pending investigations, information regarding referrals, changes to physical health treatments and management and relevant updates on existing conditions.
4.3.6.3 Infection control
The Infection Prevention and Control team (IPCT) should be contacted for advice and support ideally prior to admission if it is suspected that the patient may have an infection or pose an infection risk to themselves or others.
Where this is not possible, the following timescales should be adhered to as a maximum:
- those being cared for onwards providing primarily physical healthcare should ideally contact the Infection Prevention and Control team within 24 hours
- those being cared for onwards providing primarily mental health care this timescale is within 48 hours
The infection prevention and control manual is available for further.
4.3.7 Requests for discharge
4.3.7.1 Discharge against medical advice
Should a patient request discharge against medical advice the following process should be followed:
- a senior member of the nursing team should discuss this issue with the patient and try to elicit their rationale for leaving, taking their wishes into account as far as possible, at the same time ascertaining the patient’s capacity to make the decision
- where the person does have capacity, colleagues should utilise their local procedure for supporting an appropriate discharge. Colleagues have no power to make them stay unless they believe that the patient is suffering from a mental disorder, in which case the provisions of the Mental Health Act may be considered
- if there is any question about the patients’ capacity to make this decision then colleagues must undertake a mental capacity assessment and document in line with the Mental Capacity Act (2005) policy. If the patient is found to lack capacity to make an informed decision regarding remaining in hospital, then medical opinion should be sought
- the doctor should consider whether it is in the patient’s best interest to remain in hospital. If this is the case, and the patient does not meet the criteria for detention under the Mental Health Act (1983), then this is likely to lead to the patient being deprived of their liberty and colleagues should consider making an urgent authorisation under the deprivation of liberty safeguards
- in all cases a full record of the assessment (including Mental Capacity Act) and any discussions must be documented in the patient’s records
- note, where a patient is expressing an objection to being in hospital for mental health treatment either verbal or non-verbal, Deprivation of Liberty Safeguards is not applicable
4.3.7.2 Request by a nearest relative for the discharge of a patient subject to detention under the Mental Health Act (1983)
Some sections of the Mental Health Act (1983) give the right to the patient’s nearest relative to request discharge from detention. Such a request must be made in writing to the hospital managers who then have 72 hours in which to respond to the request. During this period the patient’s responsible clinician will be required to review the patient and assess whether they wish to issue a barring order to prevent the discharge going ahead. For full guidance colleagues must refer to the trust procedure for the discharge of a patient detained under the Mental Health Act (1983) (amended 2007).
4.3.8 Transfers
4.3.8.1 General principles
During an episode of inpatient care they need may arise for a patient to be transferred to another care setting either within or outside the trust. Any such transfer of care should wherever possible be planned so that there is minimal interruption to the patient’s treatment programme and carried out with their consent or using the appropriate legal framework.
Where appropriate, the patient, carers and any legal representatives must be given adequate and timely information as to why the transfer is taking place. Transfers should take place ideally within working hours. For any out of hours transfers, a handover summary should be completed as soon as practicable by the referring or originating team.
Clear discussion in relation to transfer should take place and involve the patient and carers and members of the multidisciplinary team.
A detailed record is to be made in the patient’s clinical records of all aspects of patient transfer, this should include:
- follow the instructions detailed in the ward transfer guide (staff access only) to maintain an accurate patient record
- all information provided to the receiving service
- the date on which it was provided
- any additional information requested prior to the transfer
- discussion with the patient and carers about the planned transfer
For any patients with an existing do not attempt cardio-pulmonary resuscitation (DNACPR) or recommended summary plan for emergency care and treatment (ReSPECT) order, the order should be reviewed upon arrival at Rotherham, Doncaster and South Humber NHS Foundation Trust (RDaSH) services. Upon transfer outside services, the original form must be sent with the patient and handed over to the receiving service.
4.3.8.2 Transfer within the trust
It is recognised that there may be times when a patient has to transfer from one ward to another. Good communication and documentation underpin effective transfer processes.
The named nurse will complete an entry with the following details:
- date and time of transfer
- named nurse, on transferring ward
- responsible clinician, on transferring ward
- reason for transfer
- Mental Health Act status, record and ensure this is correctly captured on SystmOne Mental Health Act Office informed, who informed and when if applicable
- care plans, ensure care plans are up-to-date
- risks, ensure these are updated and captured in the functional analysis of care environments (FACE) risk assessment including any safeguarding risks
- physical health, ensure care plans are up-to-date and reflect these
- plan from formulation or care programme approach (CPA) meeting or most recent care planning meeting
- medication on transfer and items issued to transferring ward
- family or carers informed of the transfer
- patient property transfer (valuables)
- suggestions and outstanding tasks for receiving team
A member of the medical team will create an entry with the following information for a medical handover:
- reason for admission
- agreed purpose of admission
- relevant history
- progress, summary of progress, response to treatment, key risk incidents and relevant events
- physical health, any relevant medical handover in relation to existing or new conditions or concerns, medication-related monitoring and investigations
- treatment, treatment plan with respect to medications and other planned interventions
- handover of plans and, or outstanding tasks
A review of the admission assessments should occur to determine if there is any change that needs to be reflected in new documentation and consideration of the impact of transfer on the patient. This will include reviewing:
- admission clerking
- physical examination
- risk assessment
- care plans
- prescribed medications
- ensuring all admission tasks have been completed and are updated
4.3.8.3 Transfer of patients to or from another mental health care provider
For those people receiving mental health care, the principles of the care programme approach should be considered in line with the care programme approach (CPA) framework (or equivalent).
The standard discharge letter can also be used as a summary of transfer outside the trust.
Information relating to medications and allergies should be provided.
For any patients subject to detention under the Mental Health Act (1983) colleagues also need to refer to the trust section 19 transfer of patients detained under the Mental Health Act (1983) to another hospital or unit procedure.
4.3.8.4 Transfer of patients who lack capacity
Where consideration is being given to transfer a patient to another hospital and the patient who is not subject to the Mental Health Act lacks the capacity to make this decision, a best interest decision should be made involving all the relevant people (for example, family or carers).
If the person or their family are objecting to the proposed transfer arrangements, then consideration will be needed whether the matter needs to be referred to the Court of Protection. Advice should be sought from the Mental Capacity Act lead.
Where a patient does not have any family or carers and the period of stay is likely to exceed 8 weeks the named nurse or nurse in charge must make a referral to the Independent mental capacity advocate (IMCA).
All decisions regarding capacity must be recorded on the appropriate templates in the electronic patient record.
If the person is subject to a deprivation of liberty authorisation the supervisory body should be informed of the transfer and a Deprivation of Liberty Safeguards form 10 completed. If the request for authorisation has not yet been granted an email should be sent to the supervisory body to cancel the request. See the Mental Capacity Act (2005) Deprivation of Liberty (DoL) policy for further guidance.
4.3.8.5 Transfer of patients to and from a physical health care provider
If at any point during an episode of care a patient need to be transferred to a general or acute hospital bed colleagues must refer to the following for full guidance: care of informal inpatients who require care in the local acute hospital policy.
Procedure for the care and treatment of a patient detained under the Mental Health Act (1983) to a general hospital under section 17 Mental Health Legislation, Section 19 transfer of patients detained under the Mental Health Act (1983) to another hospital or unit procedure.
4.3.8.6 Transfer and discharge of patients who have a do not attempt cardiopulmonary resuscitation order in place
- Do not attempt cardiopulmonary resuscitation (DNACPR) status, it is the responsibility of the discharging clinician to ensure that the patients GP is informed of a DNACPR order via the discharge letter, and that all agencies involved in the patients care in the community are informed of the order. The DNACPR order must be reviewed before discharge. It may not be possible to review the DNACPR for out of hours transfers, at this point the review will be done by the accepting service.
- The original DNACPR order should be given to the patient or carer. Colleagues should ensure that the patient or carer is aware of and fully understands the order.
4.3.9 Contingencies
4.3.9.1 The discharge of patients in their absence
Whilst it is acknowledged that there are occasions when a voluntary patient goes on planned leave and then refuses to return the ward, the discharge of such a patient in their absence should not normally go ahead until they have been seen and assessed by either the home treatment team or their care coordinator or lead professional, and a pre discharge meeting held in their absence. Robust multidisciplinary team working between the inpatient and community teams must ensure that all relevant actions detailed in this Procedure are considered and adhered to where practicable. As a minimum, consideration should be given to notifying relevant services or individuals of the discharge, including any risk posed by the patient to self or others, any appropriate safeguarding or multi-agency public protection arrangement (MAPPA) referrals, arrangements for ongoing treatment or medication where applicable and arrangements for 72-hour follow-up from the date of discharge.
4.3.9.2 Patients who refuse to leave the ward
There may be occasions when a patient refuses to leave the hospital, particularly if they are not happy with the placement they are to be discharged to. Any patient fit for discharge does not have a right to occupy a hospital bed, but consideration must be given as to how best to deal with each individual refusal to leave the ward.
Usually, the matter can be resolved by talking to the patient and discussing their reasons for not wanting to leave. The use of force to remove a patient should only ever be considered if all other means have failed. Before resorting to this advice should be sought from the modern matron, or the senior manager on call if outside of normal working hours.
4.4 Discharge or transfer St John’s Hospice inpatient service procedure
4.4.1 Aim
This procedure is to provide additional guidance to the trusts’ admission transfer and discharge manual whose aim is to provide core guidance which is applicable to all services. This procedure represents best practice in relation to the safe and appropriate transfer and discharge of patients from St John’s Hospice inpatient unit:
- to ensure a safe, timely and effective discharge or transfer from the hospice or internal transfer for all patients
- to ensure the patient is always treated as an individual with due regard shown to their personal choice, cultural characteristics and dignity
- to take into consideration any advance care plan and preferred place of care or death (see advance statements and advance decisions to refuse treatment policy)
4.4.2 Scope
This procedure is applicable to all colleagues within St John’s hospice inpatient unit who are involved in the discharge and transfer of patients. All appropriate colleagues must be aware of the policy and ensure that they:
- complete trust approved training relevant to their role
- adhere to the admissions, transfer and discharge manual
- report any discharge and transfer related clinical incidents via the trust incident reporting system
4.4.3 Procedure
Preparation to enable safe and effective discharge which will support continuity of care, wellbeing or a peaceful death in their preferred place of care.
4.4.3.1 Multidisciplinary team
Is responsible for:
- deciding and communicating when a patient is medically fit for discharge and documenting the decision clearly within the electronic medical notes and on the discharge planning template
- discussing if additional teams are required after discharge for example, new referral to the community specialist palliative care team, or discharge information if already known to the team
- deciding the appropriateness of transferring patients to other areas as either being part of the patient’s pathway or within their best interests
- discussing this date of discharge or transfer with the patient and, where appropriate, their family or those named as closest to them
- take into consideration any advance care plan, any advance decision to refuse treatment and preferred place of care or death (see advance statements and advance decisions to refuse treatment policy)
4.4.3.2 Medical colleagues
Are responsible for:
- assessing and prescribing any medication the patient requires for discharge or transfer at least 24 hours prior to discharge. Use the trust approved method, as agreed by the Medicines Management Committee (see safe and secure handling of medicines manual, controlled drugs St John’s Hospice procedure, controlled drugs care groups, community physical health services procedure)
- write to take out’s (TTOs) for any patient attending an appointment external to the hospice. Supply enough medication to last the duration of time away from the inpatient unit and ensure a copy of the inpatient medical notes are sent with them
- completed to take out’s form or printout to be given to ward clerk to copy, scan and email to Doncaster Royal Infirmary (DRI) pharmacy and a copy to be put in discharge folder in the ward nurses’ office and saved to communications and letters in the patient’s medical notes
- if the patient has a nomad ensure that an FP10 form is completed 48 hours prior to discharge and given to the family. A copy of the FP10 must be scanned into the communication and letters section of the patient’s medical notes:
- all patients who meet the fast-track criteria (last 12 weeks of life) should be discharged with pre-emptive medications, as per national guidance. Write the instruction to administer the ‘as required’ pre-emptive medications on the trust approved non-syringe driver form, and if applicable, the instruction to administer a syringe driver. Give the forms to the nurse in charge to send to single point of access (SPA)
- for all fast-track patients, and patients with complex medication regimes, write, the general practitioner (GP) out of hours’ information form and give to the nurse in charge to email to FCMS out of hours GP service
- for patients on long term oxygen therapy (LTOT) or oxygen for palliative use, if it is a new or adjusted prescription the prescriber (who is authorised to prescribe oxygen) must complete the home oxygen order form (HOOF) as well as the initial home oxygen risk mitigation form (IHORM), if a new prescription. All information, assessment guidance and order forms, there is also a guide: A guide to the home oxygen service. liaise with the local home oxygen service in the trust via single point of access on 01302 566 999 if required. Bayswater automatically notify the trust Home Oxygen team of any new prescriptions or adjustments
- where appropriate and possible, provide the patient with the date for any required follow-up appointment for attendance to consultant’s outpatient clinics within St John’s Hospice prior to leaving the ward. Send appointment letter as soon as appointment is arranged if discharged first
- document all the above in the patient’s electronic medical records and on the discharge planning template
- within 24 hours of discharge write a detailed discharge letter to the GP and copy other services as appropriate for example, oncology, Community Specialist Palliative Care team. Offer a copy to the patient
- if appropriate, ring the GP and discuss any complexity in discharge, symptom management and prescribing decisions for example, complex regimes and shared care protocols
- during an episode of inpatient care a need may arise to transfer a patient to another care setting either within or outside the trust. There is a need for good communication between the trust and the receiving hospital or unit. Photocopies or printouts of the relevant records must be provided and a formal documented letter or handover of care between the trust and receiving service
A detailed record is to be made in the patients transfer letter of:
- all information provided to the receiving service
- the date on which it was provided
- who provided it
- any additional information requested prior to the transfer
- discussion with the patient and carers about the planned transfer
- if applicable, the recommended summary plan for emergency care and treatment (ReSPECT) and do not attempt cardiopulmonary resuscitation (DNACPR) information
- rationale for transfer
4.4.3.3 Ward coordinators and named nurses
Are responsible for:
- on admission the admitting nurse must assess and identify any special requirements that may need to be considered to facilitate the patient’s discharge. Discharge documentation must be commenced on or as soon as possible after admission and all communication and action taken concerning discharge clearly documented in the medical notes and on the discharge planning template. Adhere to the admission, transfer and discharge manual
- once a discharge date has been set, coordinate the discharge process, taking into account patient needs and wishes which may be included in advance care plan, any advance decision to refuse treatment or preferred place of care or death (see advance statements and advance decisions to refuse treatment policy)
- if the patient needs equipment to go home then ensure timely referral to occupational therapy. Consider referral to the physiotherapist for mobility assessment and stair assessment, where applicable
- commence the discharge check list prior to discharge
- record and manage appropriately any delays in discharge or transfers of care as per the safe discharge and transfer of patients from the adult and older persons mental health service inpatient wards
- allow opportunities for the different colleague groups to discuss and agree the discharge care plan via various arenas such as case conferences, best interest meeting and internal and external multidisciplinary team meeting agendas
- obtain clarity from patient, family or medical team on mode of discharge transport and document clearly in patient’s notes. Some patients may require a special ambulance (bariatric) or the ambulance service to access the property prior to discharge. This must be identified earlier to prevent a delayed discharge
- make appropriate arrangements for the provision of any support services required in the community checking with the patient, family or carer that they know how to access these services in the event of an emergency
- order medications to take home (TTOs) at least 24 hours prior to discharge
- if the patient has a nomad (blister pack of medications provided by the pharmacy) ensure that an FP10 form is completed 48 hours prior to discharge and given to the family
- cross-reference prescribed discharge medication against medication delivered and the take home medication chart. Liaise with pharmacy or prescribing medic for discrepancies. Complete IR1 if deemed appropriate
- provide the patient, family or carer with a to take out’s (TTOs) both verbally and a copy of the to take out prescription
- for fast-track patients, email the pre-emptive instruction to administer (non-syringe driver form) and the syringe driver instruction (if applicable) to the single point of access (SPA) at doncaster.spa@nhs.net. For all fast-track patients, and patients with complex medication regimes, scan and email the GP out of hours’
information form to FCMS out of hours GP service at ooh.doncaster@nhs.net - produce a discharge communication sheet for all appropriate services required (district nurses, Community Specialist Palliative Care team) to be involved in patient care. Complete any appropriate risk assessment
- document all of the above clearly in the electronic medical records and on the discharge planning template
- on transfer of patients to another care setting either within or outside the trust, coordinate transfer:
- organise transport
- ensure that written and verbal handover is given to the receiving organisation
- ensure that the relevant paperwork is collated and prepared for the transfer
- recommended summary plan for emergency care and treatment (ReSPECT) and do not attempt cardiopulmonary resuscitation (DNACPR) information, if applicable
- ensure that the patient and family or carers are aware of the transfer and the rationale
- if the patient has an identified infection risk this must be discussed with the receiving service to allow them time to make any necessary arrangements for the management of the infection once the patient is discharged to their care. All relevant information must also be documented on the patient’s transfer or discharge letter and care records updated accordingly
4.4.4 Recommended summary plan for emergency care and treatment and do not attempt cardiopulmonary resuscitation decision
Recommended summary plan for emergency care and treatment (ReSPECT) and do not attempt cardiopulmonary resuscitation (DNACPR) status: it is the responsibility of the discharging clinician to ensure that the patient’s GP is informed of any ReSPECT discussion and DNACPR decision via the discharge letter and that all agencies involved in the patient’s care in the community are informed of the order. The ReSPECT and DNACPR form must be scanned into the medical record, in communications and letters, and titled “ReSPECT” on discharge.
The ReSPECT and DNACPR decision must be reviewed before discharge. It may not be possible to review the DNACPR for out of hours’ transfers. At this point the review will be done by the accepting service.
The original ReSPECT and DNACPR form should be given to the patient or carer. Staff should ensure that the patient or carer is aware of and fully understands the form and decision.
All ReSPECT and DNACPR decisions must be documented on the ReSPECT or DNACPR template in the patient’s medical records.
4.5 Discharge or transfer of in-patients from Hawthorn and Hazel wards procedure
4.5.1 Aim
This procedure provides a description of the current recommended best practice for safe and successful discharge of patients from Hawthorn and Hazel wards of the intermediate care inpatients services at Tickhill Road Hospital.
4.5.2 Purpose
The detail contained within this procedure applies to all levels and disciplines of staff that provide a service to the patients within Hawthorn and Hazel ward, intermediate care inpatient services.
4.5.3 Procedure
4.5.3.1 Procedure for transfer and discharge planning and implementation for patients from Hawthorn and Hazel ward of the intermediate care inpatient services
- All patients will have an expected date of discharge (EDD) identified on admission by the admitting registered nurse (RGN) and documented on SystmOne.
- A board round will be undertaken daily by the multidisciplinary team (MDT) to review progress with patients and update them about their expected date of discharge.
- The discharge co-ordinator will update the nominated relative or carer once the reviewed expected date of discharge has been agreed by all the multidisciplinary team and patient.
- At each board round no criteria to reside (NCTR) status is reviewed by the multidisciplinary team and determined using the following 3 criteria:
- does the patient have clinical needs that must be met within the intermediate care bed base? yes or no
- are there any outstanding multidisciplinary team assessments that need to be completed? (nursing, occupational therapy, physio, pharmacy, social worker) yes or no
- does the patient require ongoing rehabilitation, which can only be completed within an intermediate care bed base? yes or no
No criteria to reside (NCTR) status will be recorded after the ward round on SystmOne and a daily report generated by the ward manager.
- Discharge will be discussed as part of the agenda at the weekly multidisciplinary team meeting and during bounds rounds held twice a week with patients receiving care on Hawthorn and Hazel wards.
- Discharge planning will involve all active members of the rehabilitation team, the patient and, or their representative.
- The multidisciplinary team meeting relating to the safe and successful discharge will consider individualised patient needs and as a minimum:
- preferred discharge location or suitability of this
- other needs relating to discharge location
- identified care needs beyond discharge
- identified representative, for example, family or friends
- support required from other agencies
- ability to administer own medications or to establish that arrangements are in place if unable
- safety outside the ward
- transportation outside the ward
- equipment needs
- consent and capacity relating to discharge planning
- safeguarding matters
- A home assessment or access visit will be carried out when appropriate based on clinically assessed individual needs of the patient. The purpose of this home assessment or access visit is specific to the individual patient, and the assessors will differ depending on patients’ specific needs.
- When the patient is assessed as lacking capacity to make decisions about their discharge, decisions will be made in their best interest. On every occasion staff must complete MCA1 and MCA2 to ensure that a robust record of capacity assessment and best interest decision is available for scrutiny. If the person has appointed someone to act as their attorney for health and welfare, consent must be sought from them. In all cases a representative will be identified to consult with. The patient and, or representative will be fully informed and understand the action plans relating to discharge (Mental Capacity Act 2005).
- If there are any proposals which involve a change in the person’s accommodation and they lack capacity to make the decision and have no one to represent them, an independent mental capacity advocate (IMCA) must be appointed to represent them.
- All patients and, or their representatives will be encouraged and supported to identify their preferred discharge location, suitability of this preferred discharge location will be ascertained prior to the multidisciplinary team meeting for the purpose of advising further discharge planning.
- If the property is deemed unsuitable, this will be discussed at the multidisciplinary team meeting, to enable further discharge planning, and access visits as necessary.
Once discharge plans are made, the patient will continue to be discussed at the daily ward round to ensure all outstanding tasks completed in line with the expected date of discharge.
- The registered nurse (RGN) will coordinate and facilitate a timely and individualised discharge planning process with the support of the full active multidisciplinary team in line with the expected date of discharge.
- If the patient has an identified infection risk this must be discussed with the receiving service to allow them time to make any necessary arrangements for the management of the infection once the patient is discharged to their care. All relevant information must also be documented on the patient’s transfer or discharge letter and care records updated accordingly.
- A phased discharge (if applicable to patient requirements) process will include increasing periods of time spent at the identified discharge location, with specific care needs met through a process of care planning with or without the support of other appropriate agencies as agreed in the discharge planning meeting.
- Referrals to other agencies will be made as the need is identified for the purpose of safe and successful discharge, in line with the expected date of discharge and within the Mental Capacity Act (2005)
- Where other agencies are to provide care beyond discharge; all active agencies or professionals will be notified of the expected date of discharge will be confirmed and agreed.
- Patients identified as having ongoing needs will require a formal assessment by the registered nurse and will be referred to the specific service prior to discharge and notified of discharge date. For example, community nursing, Community Mental Health team, drug and alcohol services.
- All professionals involved in providing care or treatment will ensure that all details are added to the discharge report or letter; the discharge report or letter will be completed, proofread, edited and finalised prior to the date of discharge.
- Any training required to ensure the continuation of patient care delivery beyond discharge will be coordinated by the registered nurse and action plans formulated in the safe and successful discharge goal.
- A copy of the discharge report will go with the patient on the date of leaving the ward and an electronic version sent to the registered general practitioner (GP).
- Discharge letter to include details of do not attempt cardiopulmonary resuscitation (DNACPR) recommended summary plan for emergency care and treatment (ReSPECT) document.
- Patients and, or their representatives will have a clear understanding of the plans for future rehabilitative, social and continuing health care, its location, frequency and purpose. The plan for this will be communicated by the named professional.
- Follow-up plans and details will be recorded by the multidisciplinary team onto the patient’s discharge report or letter, to include:
- type of follow-up, for example, physiotherapy, discharge medicine referral (DMS) to community pharmacy
- point of contact, for example, name and contact number
- date of any appointment, if known
- contact details of whom to contact in the case of an enquiry
- Patient and, or their representative will be provided with the contact details for any relevant equipment sources.
- All patients will receive information as to how to contact out of hours doctors and social services on the discharge letter.
- The original do not attempt cardiopulmonary resuscitation (DNACPR) order or recommended summary plan for emergency care and treatment (ReSPECT) document should be given to the patient or carer. Staff should ensure that the patient or carer is aware of and fully understands the order.
4.5.3.2 If the patient is identified as having ongoing care needs beyond discharge
- Allocated social workers will be invited to attend all case reviews and pre-discharge planning meetings for the purpose of supporting discharge planning.
- Any patient with complex moving and handling needs will have a moving and handling plan completed by their occupational therapist (OT). This will highlight specific handling and transfer techniques, equipment required and the number of people required to complete safe moving and handling of the patient. The moving and handling plan will be forwarded to relevant carers and care agencies and community occupational therapist (to enable future review).
- Assessment by the registered nurse and will be referred to the specific service prior to discharge.
4.5.3.3 If equipment or adaptation needs are identified as essential for discharge
Any additional items of equipment or adaptations deemed essential for discharge will be in place on or prior to the discharge date.
4.5.3.4 During the week of discharge
All discharge plans for those patients receiving care in Hawthorn and Hazel ward will be documented on the discharge planning template on SystmOne. To include:
- transport arrangements will be made and confirmed at least 48 hours prior to the discharge date
- 14 day supply of all required medications and dietary supplementation will be provided (safe and secure handling of medicines manual and nutrition policy)
- the pharmacy team will highlight if the patient previously used boxed medication or monitored dosage systems (MDS) whilst in the community. All monitored dosage systems to be ordered from the trust contracted pharmacy supplier
- the registered nurse (RGN) will identify from the patient and, or their representative how, where and who will be responsible for obtaining further supplies of medications for the patient and include this detail in the discharge letter
- all medication required beyond discharge will be received by the ward 48 hours prior to the discharge date, wherever possible
- supplies of all dressings, catheter supplies, continence aids will be arranged 48 hours prior to discharge
- the registered nurse will support the patient to apply for the return of any money or property stored in general office (patients’ monies and property procedure)
- final plans will be agreed and confirmed with the patient and, or their representative as arrangements are confirmed
- the registered nurse will ensure that the patient and, or their representative are provided with the contact details (and a link contact, where possible of all agencies providing care beyond discharge in the discharge letter
- the discharge co-ordinator will offer the patient, and, or their representative Care Opinion access and provide support with completion as required
4.5.3.5 On the day of discharge
The discharge co-ordinator will agree a plan for post-discharge follow-up with the patient and, or their representative, details of this plan will be entered into the discharge report, follow-up section. This will include an identified date for post discharge phone call for patients on Hawthorn or Hazel ward.
An identified patient representative will be contacted within 10 minutes of patient leaving the ward to inform them of the departure, (if this is an identified need recognised during discharge planning process).
What the patient will be provided with:
- medication supply of 14 days. Which is either boxed medication or monitored dosage system packs. Monitored dosage system packs will have been organised through the trust’s contracted pharmacy supplier. All medications dispensed will be checked by 2 registered nurses (RGNs) against the current prescription and the list of medications which will go with the patient. The exception is patient group direction (PGD) medications. Only named patient medication is supplied.
- monitored dosage system packs which are being organised through the trust’s contracted pharmacy supplier will be checked prior to discharge and pick up or delivery will be arranged
- all patients will take a signed copy of the discharge letter with them when they leave the ward
- ensure that the original do not attempt cardiopulmonary resuscitation (DNACPR) order or recommended summary plan for emergency care and treatment (ReSPECT) document goes with the patient if an order has been made
- any dressings, catheter supplies or continence aids that may be required
- a copy of the discharge letter will be sent electronically to the GP on the day of discharge, via SystmOne
4.5.3.6 Care beyond discharge
Post discharge follow-up contact will be made by the discharge co-ordinator, at a time frame agreed with the patient and, or their representative prior to the discharge date as part of the discharge plan; this will not be more than 2 days after discharge. This post-discharge follow-up may consist of a phone call or home visit depending on the patient’s individual needs.
The outcome of the post-discharge follow-up contact will be recorded in the patient record and action plans completed relating to any event or issue arising from this contact before the patient’s care is formally concluded.
4.5.3.7 Delayed discharge
In the event of discharge being delayed beyond the expected date of discharge:
- a report will be published every day identifying patients who meet the no criteria to reside criteria
- the ward manager will review the report daily and any escalations sent
- escalations are sent in accordance with the shared no criteria to reside policy
4.6 Children and young people’s mental health service (CAMHS) out of hours service procedure
4.6.1 Aim
This procedure is designed to ensure all children and young people have timely access to mental health assessments out of office hours when the urgent criteria are met across the care group localities (Rotherham, Doncaster, and North Lincolnshire).
Out of hours is defined as 8pm to 8am every day.
4.6.2 Scope
The out of hours service is provided for all children and young people (under 18 years of age) across the trust that require an urgent mental health assessment out of hours.
Referrals will be accepted from the following:
- accident and emergency departments (A&E), also referred to urgent, emergency care centre in Rotherham
- paediatric wards (or any other ward with a 0 to 18-year-old admitted)
- section 136 suite
- police via section 136 or A&E
This procedure is for use by all child and adolescent mental health service (CAMHS), approved mental health practitioners (AMHPs) and for information for all agencies listed above who refer to the out of hours child and adolescent mental health service and adult liaison teams in acute trust (for their understanding of the processes for those under 18 years of age).
This procedure should be read in conjunction with the clinical risk assessment and management policy and assessment and care of children and young people with mental health needs who are placed in an acute general hospital ward policy.
4.6.4 Procedure
Out of hours assessments will take place in general hospitals (urgent or emergency care services) and in-patient wards, including adult mental health. No home visits will take place out of hours due to safe lone working. See the lone working policy and paragraph 4.10 for further information. Police have access to a police surgeon and liaison and diversion service (locality specific) in the first instance if a young person is in custody, but where they have mental health concerns or feel that a young person requires a hospital bed, then they can access out of hours clinicians for advice.
The on-call clinician will not be expected to make phone calls to patients at home or to children’s homes to offer support. In exceptional circumstances, calls may be made where this has been previously agreed for a time limited period identified within a care plan and shared with child and adolescent mental health service practitioners in advance.
4.6.4.1 Referral process
Referring agencies (A&E and wards) will contact single point of access (SPA) who will contact the Tickhill Road Hospital switchboard in the first instance on 01302 566 999, who will then contact the on-call clinician. Child and adolescent mental health service clinicians will contact the referrer and triage the referral by phone to determine suitability and necessity to attend the ward or A&E to undertake an assessment.
Child and adolescent mental health service clinicians will assess all young people up to the age of 18 years who meet the urgent criteria (see 4.6.4.2). Assessments may be face to face or via phone. Phone assessments may be based on the referral information, presentation and risks identified and it may be in the best interest of the young person or family to reduce length of time in urgent or emergency care centre environment.
For young people aged 17 years and 6 months and above will be given the choice of child and adolescent mental health services or adult services.
4.6.4.2 Criteria for urgent referral
Clinicians will assess either in person or via the phone if the following conditions are present:
- following an episode of self-harm
- where a young person has attended A&E following an episode of self-harm where there was suicidal intent, and they are refusing to be admitted to the paediatric ward
- if a young person presents in A&E or on the ward and has expressed suicidal thoughts and has an active plan for suicide but have not currently self-harmed, for young people under 16 years old an admission to paediatric ward should be considered
- where there is evidence of major thought disturbance suggestive of a psychotic episode
To undertake a comprehensive assessment and discharge plan a parent or carer will be required to be present; in the case of children in care, this may be a social worker, foster carer or residential worker.
If the clinician conducts a phone triage and deems that it is an inappropriate referral, then the referring clinician should make a referral to the appropriate agency such as social care. It is not the responsibility of the out of hours child and adolescent mental health service clinicians to forward on inappropriate referrals.
4.6.4.3 Options for referrers
- A young person may be discharged from A&E without a child and adolescent mental health service assessment with the agreement that the child and adolescent mental health service Crisis team contact the family or young person the next working day and triage as per referral process, this may include arranging an urgent assessment, routine follow up or signposting and discharge. The referrer needs to contact the CAMHS Crisis team as per paragraph 4.6 to inform of the circumstances of presentation and to discuss immediate safety planning.
- A young person may be admitted to a paediatric ward without a child and adolescent mental health service assessment, this should always be with the support and supervision of a parent or carer unless there are safeguarding issues, or the parent or carer is increasing the risk. When considering admission, the clinician should refer to the National Institute for Health and Care Excellence guidance for self-harm NG225 (2022).
- The young person will then be assessed when they are fit for assessment the following day by the child and adolescent mental health service crisis team.
- Consent to care and treatment and discharge should be considered, see trust policy.
4.6.4.4 Outcomes from assessment
Following assessment there are a range of alternative options, dependent on the presentation and risk management plans, these may include:
- discharge home with a safety plan and follow-up contact agreed
- referral to social care, where there are safeguarding concerns or specific concerns about parent or carers ability to safely care for a young person
- where there are no mental disorders identified by the child and adolescent mental health service practitioner and this is recorded in the in-patient or A&E patient records and information passed to the named worker or department who will follow up as necessary
- admission or continued admission to an inpatient ward with agreed re-assessment or follow-up
4.6.4.4.1 Tier 4 admissions
If the outcome of a child and adolescent mental health service out of hours assessment is that a young person requires a tier 4 bed, attempts should be made to ensure the young person is kept in the least restrictive environment possible and kept safe with risks to self or others managed or agreed with whoever is responsible for their safety. Mental health wards should be used as a last resort where there is an acute onset of a severe mental illness or there is imminent risk to self or others, this is a decision made in conjunction with senior managers on call.
Tier 4 admissions are processed as per NHS England operating handbook protocol and completion of the referral form to access tier 4 (formerly referred to as “form 1”).
For South Yorkshire residents in the first instance a referral form to access tier 4 is completed, and contact made with the on call psychiatrist for the Becton centre via 0114 271 7000 to discuss and email the detail to scn-tr.becton.centre@nhs.net and copied to the local NHS England case manager.
For North Lincolnshire residents in the first instance a referral form to access tier 4 is completed and sent to Inspire child and adolescent mental health service hospital via the email hnf-tr.inspire-referrals@nhs.net.
4.6.4.5 Record keeping
Where child and adolescent mental health service Crisis team practitioners attend a ward or department, they will input assessment summary and risk management and discharge plan in the hospital, patient notes or records.
The child and adolescent mental health service on call report on SystmOne should be completed for all out of hours contacts, including those where the young person has not been assessed.
A functional analysis of care environments (FACE) risk assessment and detailed contact or session note should be completed on all assessed young people. Please see appendix I recording of referrals and activity on SystmOne for detail of how to register a patient not known to child and adolescent mental health service on SystmOne. The child and adolescent mental health service Crisis team must be informed of any assessment the following working day. Correspondence to general practitioners (GPs), patient, family or carers will be followed up by the child and adolescent mental health service crisis team or the locality team (if the person is open to them) and not by the assessing out of hours clinician.
Patients that have been open to child and adolescent mental health service prior to November 2017, their Silverlink records can be accessed via the Stalis archive facility in SystmOne.
4.6.4.6 Handing over cases or information
Following an assessment, the clinician who has completed the out of hours assessment is responsible for handing over the information to the relevant team via SystmOne task and where urgency requires, phone contact is made with the service to ensure that the case is followed up with urgency.
For those individuals who are already open to child and adolescent mental health service, the child and adolescent mental health service crisis team should hand over all details relating to the presentation and discharge plans along with any requirements for their follow-up.
Please see contact information below for all 3 child and adolescent mental health services and the community eating disorder service.
4.6.4.6.1 Rotherham
-
Phone
Duty team, Kimberworth Place. SystmOne, Rotherham administration.
4.6.4.6.2 Doncaster
-
Phone
Duty team, Doncaster Children and young people’s mental health service. SystmOne, Doncaster administration.
4.6.4.6.3 North Lincolnshire
-
Phone
St Nicholas House, child and adolescent mental health service. SystmOne, NL administration team.
4.6.4.6.4 Eating disorders
Stone Castle, Conisbrough. SystmOne, task eating disorders.
If staff believe that psychiatric medical assessment is required, make this clear within the handover of the case, further information may be required from the appropriate psychiatrist.
4.6.4.7 Out of area patients
Where a young person has presented to a local hospital out of hours, the child and adolescent mental health service Crisis team will hand over the information to the child and adolescent mental health service team where the young person resides or is registered with a GP. Young people and families need to be made aware that follow-up arrangements may be different to those expected within trust services.
4.6.4.8 Gillick competency or mental capacity
If a young person under 16 is deemed to be Gillick competent or is aged 16 or over and has mental capacity and able to consent to admission and treatment, an assessment can be completed without an adult present. If staff make the decision that a young person is Gillick competent or has mental capacity to make the decision this needs to be clearly recorded in your record keeping and how that decision has been reached. However, it is acknowledged that on discharge from A&E or the ward, there is a vital safeguarding role and responsibility for the parents or carers. This should be explained to A&E and ward staff with the suggestion that it would be advantageous to wait until the next working day when there is no responsible adult present so that the locality team can assess and liaise with family and appropriate services. If there are any concerns or suspicions that there may be safeguarding issues, then the local out of hours safeguarding team should be contacted for checks to be made and possible advice on any recommendations or interventions. If safeguarding concerns are highlighted these need to be handed over to the locality teams. Staff may consider possibly discussing in safeguarding supervision to support reflection. See consent to care and treatment policy for more detail around capacity and lack of capacity in relation to consent.
4.6.4.9 Staff capability
Child and adolescent mental health service staff undertaking out of hours assessments should be band 6 and above clinical staff.
No clinician will be put on the out of hours rota until they have completed the capability framework (appendix G).
4.6.4.10 Lone working
All assessments will be conducted within a contained, staffed environment, generally either within A&E or on the paediatric ward or general adult ward. Whilst assessments may be undertaken alone, there will be access to other health professionals and support from crisis services if necessary.
Appendix H key contact details contain the details of the three general hospitals and other useful contact details.
If a clinician is called out, they should contact the child and adolescent mental health service on call manager to inform them of the need to travel and should agree arrangements for “reporting in” arrangements to them when they have returned home following an assessment to ensure that they have returned home safely. Staff should have completed a Lone worker risk assessment that reflects their need to undertake this work.
4.6.4.11 Transport
If called out, staff claim (via on-line e-expenses) the distance being identified to and from home address, identifying that this was outside usual duty hours. If staff require access to taxi services due to medical, fatigue or ability reasons, this will or can be arranged via Tickhill Road switchboard (on 03000 213 000).
4.6.4.12 Claiming time back, rest periods, payment
When called out (either in person or phone) to complete an assessment, the time taken (from leaving to returning home, phone liaison and record keeping) can be claimed. This is done by confirming the time of the call, venue and duration. This should be shared with the clinician’s team manager for processing at the end of each month.
On call during the week may mean that staff are expected within their work environment the next day. If the clinician is unable to safely attend for work the next day, they will inform the team manager of this, with an expected time of attendance and provide feedback in relation to the case.
Whilst there is no formal requirement to provide any additional rest time when callouts have been less than 5 hours in duration during the week (11 hours of “rest”), the team managers can provide flexibility in working hours to ensure that staff have appropriate rest and are capable of returning to work safely and effectively.
Following being on call the clinician will designate time to administration or online training to avoid the potential need to cancel patients, this is supported by team managers.
Child and adolescent mental health service clinicians can claim back time or additional overtime payment for a callout, they will inform the child and adolescent mental health service (CAMHS) service manager of the following:
- date of the call
- location called to (Rotherham, Doncaster or Scunthorpe)
- duration of the call-out, time from leaving home to returning, including administrative time
On occasions, the processing of payments for interventions can be provided over the phone, this would include assessments and formulation of cases where it was not possible or relevant to attend the location. As with all other clinical interventions these will be recorded on SystmOne.
Full time child and adolescent mental health service clinicians are expected to provide a minimum of 2 slots in a month period, dependent on the number of shifts required to be covered and the availability of staff. The on-call allowance paid for staff is calculated by sessions, the maximum number required is 1 in 9. Out of hours child and adolescent mental health service managers are expected to provide 4 to 5 slots in a month (with weekend or bank holiday days being counted as 2 slots). Both clinicians and managers are responsible for providing additional cover if any clinical activity is arranged for the following day. If the rota has been amended to provide cover, then the manager of the rota needs to update the switchboard, to update their rota. If the rota manager is unavailable the clinician will need to do this. The switchboard is contactable on:
-
Phone
Managers and clinicians are required to update the switchboard when changes have been made to contact phone numbers.
4.6.4.13 Bank holidays
Clinicians on call on a bank holiday are entitled to time back to reflect the time on call (irrespective of if they are called out). The team manager will authorise the additional time owing following a bank holiday and add the time to annual leave entitlement.
4.6.4.14 On call manager
In addition to an on call clinician, there is an on-call child and adolescent mental health service manager, which is either a senior clinician, pathway lead or child and adolescent mental health service manager. The on-call manager is contacted via the Tickhill Road switchboard 03000 213 000).
If the on-call clinician has made arrangements to go out and assess a child or young person they need to contact the out of hours manager to make them aware of the arrangements, and particularly the time they intend to go out. Following the assessment, the clinician will need to contact the on-call manager to make them aware they have completed the assessment and are back home safe. Failure to contact the on-call manager following an assessment will result in the manager contacting the last known location or next of kin to ascertain the safety and whereabouts of the clinician.
The on-call clinician can also contact the on-call manager for advice and assistance surrounding the assessment process and the management of risk. The on-call manager will not be expected to attend any assessment. Any advice or instructions that are passed to the clinician from the manager will be done so on the information that they have received from the clinician.
The on-call manager can be contacted to support any professional differences with other agencies if required and they can support with the liaison between services.
The on-call manager can be contacted to discuss any case, for support in decision-making and access to tier 4 beds or any other planned admission. In the event of a young person requiring access to an adult mental health bed or further organisational advice and support, they can contact the director on call via switchboard.
In exceptional circumstances where the on-call clinician is not available and there is a scenario where a young person is at risk, the on-call manager will undertake any activities to support the welfare of a young person; this includes liaison and support to other services or escalating concerns to senior managers.
4.6.4.15 Rota for on call
The rota will be available for staff at least 4 weeks in advance of the start date. Prior to this staff will be asked for details of availability or non-availability within a set period of time for the rota to be developed.
4.7 Safe transportation of patients and staff (adult and older person’s mental health and learning disability)
4.7.1 Aim
There are times when clinical colleagues working within adult and older person’s mental health and across learning disability services are required to arrange the transportation of patients for the purpose of escort or transfer. This may be due to the patient requiring a transfer to another inpatient facility, attending legal hearings, having escorted therapeutic leave, or being supported to undertake discharge preparation or therapeutic and community activities. There may also be times when clinical colleagues are responsible for organising transport arrangements for admission to an inpatient (or other) facility.
In terms of inpatient services, it is recognised that there can be an increase in the level of risk a patient poses to either themselves or others when away from the supportive environment of the Ward and Clinical teams. It is important therefore that transportation activities are risk assessed, and where possible planned in advance, and that systems of working are implemented proportionate to the level of risk.
Likewise in terms of community services, there may be times when clinical colleagues (working within an agreed scope of duties and role), are required to organise transport or transport patients. It is acknowledged that at such times these employees are undertaking work activities on behalf of the trust and the risks associated with this must be assessed and effectively managed and documented accordingly.
The purpose of this procedure is to set out the arrangements for when it is required for a patient to be transported or escorted by colleagues, with particular attention being paid to the assessment and proportionate management of any identified risks. The procedure will also outline the arrangements for procuring a taxi to transport a colleague when deemed appropriate to do so.
The authorisation arrangements for the booking of transport will also be outlined to ensure a standardised approach and to provide a process which finance and procurement colleagues can effectively monitor both the contractual and financial obligations for the trust.
The contents of this procedure are to be read in conjunction with both the leave for inpatients policy and guidance (including section 17) and the section 19 transfer of patients detained under the Mental Health Act (1983) to another hospital or unit procedure. Where appropriate the safer driving at work policy must also be adhered to.
4.7.2 Scope
The contents of this procedure apply to clinical colleagues working within adult and older person’s mental health and learning disability services. Please note that forensic services have their own patient escorting procedure (forensic services manual).
4.7.3 Procedure
In all instances of transportation of patients, whether in community services or inpatients, the same or equivalent clinical responsibilities, multidisciplinary team (MDT) duties and patient care planning, risk assessment and risk management principles and procedures apply.
The requirements of each individual patient whilst being escorted will vary, but each escort should wherever possible be planned and undertaken following consideration of any risks and in line with the agreed risk management plan and, where applicable, the requirements of the Mental Health Act (1983).
4.7.3.1 Risk assessment
All patients should have a clinical risk assessment prior to any transportation or escorted leave being undertaken; this will be updated to take account of any additional or increased risks of the patient absconding. Consideration also needs to be given to the length of the journey and arrangements for adequate comfort breaks.
From this risk assessment the following will be determined:
- method of transportation
- number of colleagues escorts required
- medication that may be required during the journey
- arrangements for if comfort breaks are required
- arrangements for colleagues to remain in contact, and able to summon assistance if needed, for example, by carrying a mobile phone
- any physical health care needs that should be handed over to the escorting colleagues, for example, diabetes
4.7.3.1.1 Factors that need to be considered when assessing the risk of absconding
Factors that indicate a patient is low risk of absconding:
- no recent history of attempts or threats to abscond
- no immediate identified risk to self or others
- current mental state, stable
- compliant with treatment
Factors that indicate a patient is a medium risk of absconding:
- past attempts to abscond
- an expression that they wish to leave the inpatient ward
- impulsive behaviour
- behaviour that may pose a risk to themselves or others
- fluctuating mental state
- fluctuating compliance with treatment
Factors that indicate a patient is a high risk of absconding:
- recent attempts to abscond
- assessed as posing a significant and immediate threat to themselves or others
- exhibiting acute symptoms of mental illness
- exhibiting challenging behaviour
- non-compliant with treatment
4.7.3.2 Care planning
A care plan is to be in place for all patients for any period of leave from the inpatient ward, including escorted leave. The care plan will be informed by the outcome of the risk assessment and include details of the arrangements that need to be considered as set out in section 4.1 above.
It should, where relevant also include the following:
- nature of the escorted leave
- reason escort required
- duration of leave
- destination
- transport arrangements
- number and skill mix of the colleagues undertaking the escort
- action to be taken in the event of the patient absconding
- arrangements for the administration of medication
4.7.3.2.1 Potential use of restraint
Where restraint is needed to be used to keep the person safe, it should only be carried out with:
- the person’s consent
- under the Mental Health Act (1983)
- or where the person lacks capacity, in the person best interests under the Mental Capacity Act (MCA) (2005)
- under common law
Where restraint is used the following conditions must be met:
- the person taking action must reasonably believe that restraint is necessary to prevent harm to the person who lacks capacity
- the amount or type of restraint used and the amount of time it lasts must be a proportionate response to the likelihood and seriousness of harm
- the use of the least restrictive option must be always considered
4.7.3.2.2 Safe transportation of patients with disabilities or mobility difficulties
As part of the assessment there should be a discussion with the patient and Clinical team as to their limitations and requirements for safe and comfortable transportation. Having a physical disability or mobility difficulty does not preclude the use of a car, but in such cases a moving and handling risk assessment will be completed, and consideration be given to:
- what assistance the patient will need to get in and out of the car
- the amount of legroom provided in the car
- whether there is capacity in the vehicle for a wheelchair or other equipment to be carried
4.7.3.3 Medication
Where medication is required during the escort this should wherever possible be ordered in advance. Colleagues should ensure there is sufficient supply for the journey, and it is to be carried either by one of the colleagues undertaking the escort, or in a secure area of the car for example, locking glove compartment or rear boot.
Patients are not to hold their own medication during any colleague escorted leave unless this is part of the care plan and reflected in the patient risk assessment.
4.7.3.4 Transport of clinical records with the patient
Any clinical records which are to be carried during the escort must be in an appropriate, sealed package and clearly addressed for the destination, with no patient identifiable information visible. Clinical records are to be carried either by colleagues, or in a secure area of the vehicle. The patient must not be left unsupervised with their clinical records.
4.7.4 Transports options
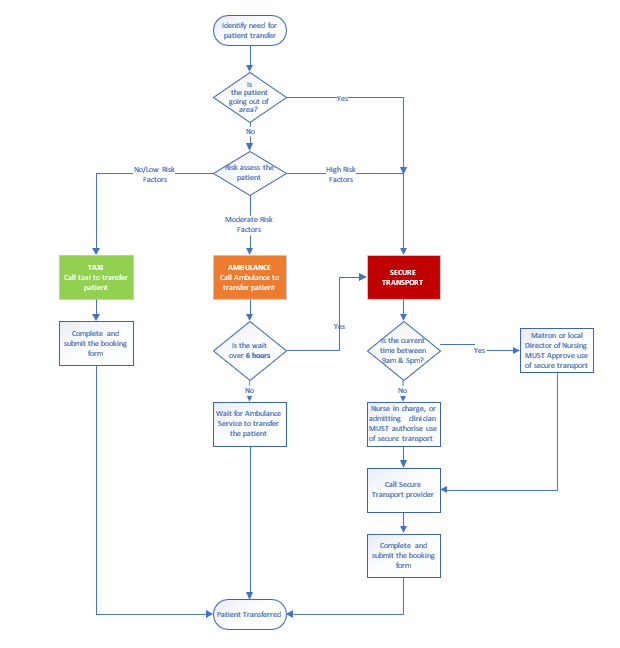
4.7.4.1 Transport options procedure
- Identify need for patient transfer.
- Is the patient going out of area?
- If yes, proceed to 4.7.4.1.3 secure transport.
- If no, proceed to 4.7.4.1.1 risk assessment.
4.7.4.1.1 Risk assessment
Assess the patient, if no or low risk factors (taxi)
- Call a taxi to the transfer patient.
- Complete and submit the booking form.
- Patient transferred.
4.7.4.1.2 If moderate risk factors (ambulance)
- Call ambulance to transfer patient
- Is the wait over 6 hours?
- If yes, proceed to 4.7.4.1.3 secure transport.
- If no, wait for ambulance service to transfer the patient.
4.7.4.1.3 If high risk factors or going out of area (secure transport)
- Is the current time between 9am and 5pm?
- If yes, matron or local director of nursing must approve use of secure transport.
- If no, nurse in charge, or admitting clinician must authorise use of secure transport.
- Call secure transport provider.
- Complete and submit the booking form.
- Patient transferred.
4.7.4.2 Use of trust owned or colleague vehicles
A small number of colleagues, who work within an agreed scope of duties and roles will be supported to transport patients (and sometimes carers) in their own vehicles (or in equivalent work provided vehicles, such as a ward, service people carrier or car). These colleagues would ordinarily be allied health professionals or relevant team members supporting patients with rehabilitation activities in the community or transporting patients in their cars for home assessments and to progress therapy goals linked to rehab or discharge from inpatient units.
The trust has a responsibility to acknowledge the risks associated with this and these must be assessed and effectively managed.
In situations where it is agreed that colleagues can transport patients (and or carers) the team manager must be satisfied that:
- there is an overall clinical rationale
- the activity fits with the role and duties of the colleague and the colleague consents to using their vehicle for this purpose
- the use of this transportation is in line with the patient’s care plan and risk assessments or procedures are in place along with any necessary controls before the journey is undertaken
- that the necessary vehicle, and driver requirements are fulfilled in line with the safer driving at work policy and the colleague has appropriate business insurance that explicitly covers them for this purpose
- arrangements are in place in the event of breakdown, colleague illness or extreme weather
- in the case of work provided vehicles, such as unit minibus or car, that any additional driver training is completed and associated procedures are followed
The team manager should also be satisfied that the colleague has competence to:
- undertake or seek completion of necessary risk assessments that consider and accommodate the needs of the patient and any hazards of the trip, the activity, any equipment to be carried
- follow the associated patient risk management plans and be able to dynamically review situations, tasks or changes in patient needs or risks to make changes or seek additional guidance or help and make use of related procedures (such as summoning help or emergency services)
- summon emergency assistance, and have the means to do this such as, a phone
- recognise situations and scenarios that may arise with patients (and or carers) during transportation where safety could be compromised and be competent to take appropriate action
If the colleague is required to assist patients in or out of vehicles or loading and unloading, the team manager must be satisfied that:
- the colleague is up-to-date with the required level of moving and handling training and able to assist in transfers in and out of their vehicle for the client group
- the colleague is up-to-date with all other relevant risk management training completed, including infection prevention and control, managing violence and aggression, clinical risk assessment and management
- any specialist equipment or protective clothing is supplied if this is required for example, spill kits and first aid kits
If it is a three colleague escort the patient is to be seated between two staff for the duration of the journey. In the event of it being a single colleague escort for safety reasons the patient is not to be seated behind the driver. All colleagues must exit the car before opening the door for the patient, to minimise the risk of absconding.
4.7.4.3 Use of local ambulance service
- Rotherham or Doncaster, Yorkshire ambulance service
- North Lincolnshire, East Midlands ambulance service
All trust inpatient wards (including the Woodlands in Rotherham) in the event of a medical emergency will call an ambulance using 222 internally.
In this situation the ward colleagues must brief the ambulance colleagues on any identified risks, and if necessary, accompany the patient in the ambulance. It is also important that the Nurse in charge contacts the local accident and emergency department to give them information as to the patient’s mental state, legal status, capacity to consent, treatment plan, and identified risks. However, if this is not possible, an accompanying letter with the information on should be sent with the ambulance or escorting colleague.
In other non-emergency situations, an ambulance may need to be arranged. Examples of these scenarios are including, but not limited to, transfer of patients between trust sites, transfer from acute providers to a trust site, if the patient has a disability or physical condition which makes it difficult or uncomfortable, or not possible for them to travel in a car. In these cases, a booking will be made through the ambulance call centre as far in advance as possible of the transport being required. When making the booking colleague should inform the ambulance service of any identified risks, and escort requirements (as this may influence the type of ambulance and pick up arrangements). This method of transport should be used as a primary option ahead of using private transport services where clinically possible. Colleagues need to be aware that non-urgent transfer requests may have an extended response time of 4 to 6 hours. If the response time is beyond this timescale, alternative transport options can be considered.
In community services a non-emergency ambulance may be requested to transport a patient to an inpatient setting. However, if this wait is several hours and there is a risk of impact to the patient’s mental health, if risk assessed and appropriate to do so alternative forms of transport may be used to transport the patient. This must be documented in the patient’s risk management plan (see section 4.1).
4.7.4.4 Use of taxis
There will be times when transportation of patients in a taxi is safe and appropriate. This must be risk assessed by the patient’s responsible team or ward and a taxi booked if safe and reasonable to do so.
Some examples of when use of a taxi may be appropriate are:
- attendance for a planned hospital appointment for informal patients and those patients on a section accessing section 17 leave and therefore assessed as low risk
- facilitating a patient’s home visit
- to facilitate contact with family members or carers when we have a patient out of area and there are no alternative forms of transport available
- if a patient requires urgent treatment or assessment at a general hospital, the wait time for an ambulance is excessive, and the patient is viewed by the Nursing or Community team as low risk and therefore conveyance by taxi will prevent further deterioration in physical healthcare
- admitting a patient to one of the crisis houses when there is no alternative transport available
- to facilitate a planned appointment with the Crisis team at one of the trust sites, this could be due to the risk associated with the patient and therefore unsuitable to have the appointment in their own home or if the patient does not have any access to other transport
- to enable a patient to access safe space or crisis cafés
- when an informal patient is being repatriated or moved to an alternative trust or NHS mental health setting
- a patient is being discharged home or utilising home leave and there is no access to appropriate public transport, or a family member is not available to transport them
- transporting perinatal patients to mother and baby units when deemed appropriate by a community team
- a patient has been assessed in accident and emergency (A&E) and does not require admission to hospital home and there is no access to appropriate public transport, or a family member is not available to transport them
- a patient is assessed in the 136 suite and does not require admission to hospital home and there is no access to appropriate public transport, or a family member is not available to transport them
Prior to transporting a physically ill patient in a taxi, a review should take place jointly by a medic and a nurse to determine the suitability of this transport option, where appropriate please refer to the guidance in the patient falls policy (prevention and management) manual. If deemed appropriate the patient must be accompanied by a colleague.
Note: there may be occasions when a taxi is required to transport a colleague. Such occasions may include:
- when additional colleagues are required at an acute general hospital to facilitate a change of observation level
- when colleagues are deployed to another hospital site, and they do not have business insurance and therefore are unable to use their own vehicle or do not have access to a vehicle
- a colleague is injured whilst on duty and requires hospital assessment or to return home and there is no alternative transport available
4.7.4.5 Use of private transport
4.7.4.5.1 Rationale for use of private transport
There may be occasions when it may be necessary to employ the services of a specialist transport and escort company.
This would ordinarily be for the transportation of any detained patient as they require a higher level of supervision or for those patients who cannot tolerate a lengthy wait (more than 2 hours) for a local ambulance.
Other examples of when private transport may be required include:
- if a patient requires urgent treatment or assessment at a general hospital and the Nursing or Community team feel there is a risk of the patient absconding, assaults on colleagues or self-harming behaviours
- regardless of detention: if the patient is not known to the Nursing team or admitting professional and therefore a full assessment of risk cannot take place (for example a non-trust patient requiring transport to re-patriate them to their local area from the 136 suite or having been on the ward less than 72 hours)
- there is concern regarding the patient’s level of aggression in their community placement and therefore conveyance by an ambulance is not deemed safe by the admitting professional
- to bring a patient from the community into a mental health hospital setting if the professional feels they are at risk and unable or unwilling to make their own way in
- to transport a patient from one seclusion facility to another
- a patient is transferring to a secure unit, locked rehab placements or another specialist placement
4.7.4.5.2 Authorisation
The decision regarding transport for an in-patient will be made by the nurse in charge in discussion with the Clinical team as and when necessary.
For community patients, the admitting professional will decide on the most appropriate form of transport and liaise with the relevant care group for authorisation.
If the admitting professional is non-trust colleague (for example external trust colleagues or local authority colleague) the request should be made to the patient flow bed manager for authorisation during working hours and the allocated care group bed manager out of hours.
4.7.4.5.3 Booking a taxi
All bookings for Doncaster taxis are to be made through the Tickhill Road Hospital main reception. The contracted taxi supplier is Drive.
All bookings for Rotherham and North Lincolnshire taxis are to be made with the contracted taxi supplier.
-
Rotherham, A1 Taxi’s
-
Scunthorpe, 121 Taxi’s
The person ringing to make the booking must have the details of the account number (where necessary), date, time, name of passenger, name of colleague making the booking, details of the journey and the department’s budget code for it to be charged against.
When booking a taxi, the nurse in charge or admitting professional must complete the taxi booking request form (appendix T) and forward this to the service manager, modern matron or Admin team (as per local agreement) for oversight and processing.
4.7.4.5.4 Contacting the private transport company
The primary contractor for the trust is exclusive secure patient transport.
-
Phone
If exclusive secure patient transport is unavailable, then the V-care Ltd may be utilised.
-
Phone
-
Online
When making the booking it must be made clear to the company the purpose of the transport request and a full and robust handover of risk and patient care plans shared.
The transport company will request the following information:
- NHS number
- patient’s home address
- patient details:
- age
- height
- weight
- build
- illness and mental health section (if applicable)
- medical conditions
- history of violence, aggression or assault
- current behaviour and trigger factors
- history of absconsion and current risk
- history of self-harm and current risk
- full details of the person authorising payment of transfer
- handcuff authorisation (if applicable)
- details of any medication administered
When requesting private transport, the nurse in charge or admitting professional must complete the private transport request form (appendix V) for oversight and processing and forward this to:
- the service manager or modern matron
- the secure transport company: for exclusive secure transport remittance@securecareservices.co.uk or for V care finance@vcare24.co.uk.
- the relevant finance manager for the care group
4.7.4.5.5 Payment of invoices
All invoices for payment will be directed in the first instance to the purchase ledger department via email rdash.purchaseledger@nhs.net so that the invoice can be registered on the system. It will then be coded to the correct budget and forwarded onto to the locality manager within the relevant care group for authorisation so it can be processing for payment or recharged to the organisation who has agreed to pay.
Colleagues should be clear as to who will be paying for the invoice, and this will depend on the named integrated care board (ICB) for the patient. Where any agreement to recharge has been made this information should be forwarded onto to the relevant finance lead for the care group.
Patients who are registered with a general practitioner (GP) in Doncaster, Rotherham or North Lincolnshire who need to be conveyed to a hospital out of area will be paid for by their responsible integrated care board. This may be covered in the block contract arrangements the trust has with each integrated care board and would be reviewed on a case-by-case basis between finance and the Contracting team, and any recharging discussed and agreed with the commissioner.
Note, in the first instance, all invoices will be paid by the trust and on some occasions, this can then be recharged to the appropriate provider or integrated care board providing authorisation has been sought in advance. It is therefore imperative that all the necessary information is provided on the transport request form (appendix V). This will enable the Finance team to be able to recharge an alternative provider or integrated care board where necessary within the allocated timeframe (as per the Who pays? guidance, which is 30 days). If this is not provided and the trust cannot recharge the other provider or integrated care board within the timeframe, then the cost of the transport will come out of the ward or service’s budget who that requested it.
Where the cost of the transport is to be met by the trust, the budget code and purchase order (where known) should be provided on the transport request form. If this information is not readily available, the nurse in charge or admitting professional should detail the name of the service or ward.
4.7.4.6 Request for police assistance
As the patient is under the care of the trust, the police have no authority under which to transport our patients, so colleagues should not routinely contact them for assistance.
The exceptions to this are:
- the transfer of a patient detained on a section 136 to another place of safety, the police have their own policy on transferring a patient on a section 136 and 135
- the return of a patient detained under the Mental Health Act who has absconded
- if a patient is arrested
4.7.4.7 Escorting a patient to court
If a detained inpatient is to be escorted to court, colleagues are to remain with them even if they are to be held in the cells.
In the case of a patient being held in the cells the accompanying colleagues will remain outside of cells in the main court waiting area ensuring that any key risk information is communicated to the Court Custody team and an agreement made in relation to the safe management of the patient whilst in the holding cells.
4.7.5 Action if a patient absconds or goes missing whilst on escorted leave or during planned transport arrangements
Whilst all practical steps should be taken when escorting, colleagues must never put either their own safety or that of others at risk in taking measures to prevent patients from absconding.
If practical to do so a search of the immediate area should be undertaken by the escort, and if the patient is not located, the ward will be contacted by the escort and notified of the absconding.
The nurse in charge of the ward will then implement the relevant actions from the trust patients missing or absent without leave (AWOL) policy. If the patient is located but the escorting colleagues have concerns about their ability to retake the patient safely, assistance should be sought from the police.
Where a patient in the community absconds or goes missing during planned transport arrangements, it is expected that the community professional responsible for the patient will also implement the relevant actions from the trust patients missing or absent without leave (AWOL) policy.
4.7.6 Transportation of infectious patients
Movement of infectious or potentially infectious patients must be kept to a minimum. When it is necessary to transport patients to other wards, departments or premises, precautions taken to minimise the risks of transmission must continue. If it is possible to delay an investigation or transfer without adversely affecting the patient’s clinical management this should be considered. However, the presence of an infectious disease should not delay urgent clinical investigations. The receiving area or Transport team must be informed prior to transfer to ensure that they have the necessary precautions in place and that appropriate facilities are available. Where patients with known or suspected infections are being transferred for appointments, they should be seen at the end of the list and not left in waiting areas. This will allow adequate cleaning of the environment and equipment following the appointment and reduce the risks of transmission to other patients. Please refer to the infection prevention and control manual for further guidance relating to specific infections and precautions required. Consult the Infection Prevention and Control team for any further advice or guidance.
4.7.7 Reporting any incidents which occur during the transportation of a patient
Any incidents which occur during an escort (including absconding) are to be reported at the earliest opportunity onto the electronic incident reporting system via the trusts safeguard electronic incident reporting system and the responsible clinician notified.
5 Training implications
There are no specific training needs in relation to this policy, but the following colleagues will need to be familiar with its contents and any other individual or group with a responsibility for implementing the contents of this policy.
As a trust policy, all colleagues need to be aware of the key points that the policy covers. Colleagues can be made aware through:
- one to one meetings or supervision
- continuous professional development sessions
- posters
- practice development days
- team meetings
- local induction
6 Equality impact assessment screening
To access the equality impact assessment for this policy, please email rdash.equalityanddiversity@nhs.net to request the document.
6.1 Privacy, dignity and respect
The NHS Constitution states that all patients should feel that their privacy and dignity are respected while they are in hospital. High Quality Care for All (2008), Lord Darzi’s review of the NHS, identifies the need to organise care around the individual, ‘not just clinically but in terms of dignity and respect’.
As a consequence, the trust is required to articulate its intent to deliver care with privacy and dignity that treats all service users with respect. Therefore, all procedural documents will be considered, if relevant, to reflect the requirement to treat everyone with privacy, dignity and respect, (when appropriate this should also include how same sex accommodation is provided).
6.1.1 How this will be met
All employees, contractors and partner organisations working on behalf of the trust must follow the requirements of this policy and other related policies, particularly those relating to information governance. All health employees must also meet their own professional codes of conduct in relation to confidentiality.
6.2 Mental Capacity Act (2005)
Central to any aspect of care delivered to adults and young people aged 16 years or over will be the consideration of the individuals’ capacity to participate in the decision-making process. Consequently, no intervention should be carried out without either the individual’s informed consent, or the powers included in a legal framework, or by order of the court.
Therefore, the trust is required to make sure that all staff working with individuals who use our service are familiar with the provisions within the Mental Capacity Act (2005). For this reason all procedural documents will be considered, if relevant to reflect the provisions of the Mental Capacity Act (2005) to ensure that the rights of individual are protected and they are supported to make their own decisions where possible and that any decisions made on their behalf when they lack capacity are made in their best interests and least restrictive of their rights and freedoms.
6.2.1 How this will be met
All individuals involved in the implementation of this policy should do so in accordance with the guiding principles of the Mental Capacity Act (2005).
7 Links to any other associated documents
- Infection prevention and control manual
- Mental Capacity Act (2005) policy
- Section 135 Mental Health Act (1983) policy
- Mental Capacity Act (2005) Deprivation of Liberty (DoL) policy
- Advance statements and advance decisions to refuse treatment policy
- Positive patient identification policy
- Safe and secure handling of medicines manual
- Resuscitation manual
- Care programme approach (CPA) policy
- Clinical risk assessment and management policy
- Section 136 Mental Health Act (1983) policy
- Care and treatment of children under the age of 18 on adult acute mental health inpatient areas policy
- Assessment and care of children and young people with mental health needs who are placed in an acute general hospital ward policy
- Syringe driver administration of drugs via the CME medical T34 syringe driver procedure
- Controlled drugs (physical health community services) procedure
- Consent to care and treatment policy
- Healthcare record keeping policy
- Incident management policy
- Non-medical prescribing policy
- Safe and secure handling of medicines manual
- Scanning of physical documentation policy
- Self harm in primary and specialist care services policy
- Transitioning from children’s to adult services
- Safeguarding children policy
- Lone working policy
- Safer driving at work policy
- Leave for inpatients policy and guidance including section 17
- Section 19 transfer of patients detained under the Mental Health Act (1983) to another hospital or unit procedure
- Patients missing or absent without leave (AWOL) policy
- Forensic manual: patient escorting procedure
- Police assistance and conveyance for the admission of patients detained under Mental Health Act (1983) to hospital
- Infection prevention and control
- Patient falls manual (prevention and management)
- Safe and secure handling of medicines manual
- Nutrition and hydration policy
8 References
- Home to the Unknown, Getting hospital discharge right (2019) British Red Cross.
- NICE Guidance Medicines optimisation: the safe and effective use of medicines to enable the best possible outcomes (NG5).
- NICE Guidance (2015): Transition between inpatient hospital settings and community or care home settings for adults with social care needs (NG27).
9 Appendices
9.1 Appendix A responsibilities, accountabilities and duties
9.1.1 Board of directors
Board of directors is responsible for ensuring that the organisation consistently follows the principles of good governance applicable to NHS organisations. This includes the development of systems and processes for admission, transfer, and discharge of patients.
9.1.2 Chief executive
The board of directors delegates to the chief executive the overall responsibility for effective risk management in the trust, meeting all statutory requirements and adhering to guidance issued.
9.1.3 Care group directors and care group nurse directors
Care group directors and care group nurse directors are the designated leads with responsibility for the implementation of this policy and national and local guidance.
- Disseminating, implementing and monitoring this policy and the local standard operating procedure within their services.
- Facilitating collaborative working between in-patient and community services in order to provide high quality patient care.
- Monitoring any trends, themes or concerns raised during the admission process and taking action as appropriate to reduce or prevent risks and to improve the patient experience.
9.1.4 Lead clinician
Depending on the inpatient area the responsible person could be a doctor, a nurse or an allied health professional. It is their responsibility to ensure:
- they are involved in the admission, discharge, or transfer of the patient in consultation with carers and the multi-disciplinary team
- that admissions, transfer and discharges are carried out in line with the relevant service’s standard operating procedure or local procedural documents
- that all required information is shared with appropriate healthcare professionals, for example, general practitioner (GP) as detailed in the local service procedure. As a minimum the following information must be shared:
- medication
- patient discharge against medical advice
- a copy of the patient’s discharge or transfer letter
- the local security management specialist (LSMS) is informed at the earliest opportunity of the admission of a formal or informal active prisoner
9.1.5 Ward managers
Ward managers or modern matrons or service managers are responsible for:
- informing the local security management specialist at the earliest opportunity of the admission of a formal or informal active prisoner
- informing all colleagues through local induction of the trust’s admission, discharge and transfer manual and relevant local procedures or standard operating procedures
- recording and monitoring standards to ensure compliance with trust policy for admission, transfer and discharge
- monitoring, recording, and reporting delays in transfer of care as per agreed trust process
- ensuring good communication between inpatient and community agencies
- ensuring national and local guidance is adhered to
9.1.6 Local security management specialist (LSMS)
Once notification by the lead clinician, ward manager or service manager or modern matron has been received the local security management specialist must attend that specific ward and liaise with the prison officers to carry out a joint risk assessment based on the prisoner’s history obtained from the police to define responsibilities of staff during the patients’ care and continued detention. This will be reviewed at regular intervals.
9.1.7 All trust colleagues
Colleagues who come into contact with patients are seen by doctors, nurses, allied health professionals, pharmacists, psychologists, bank staff and agency workers, students and volunteers. All are expected to ensure that each person coming into their care and their carers are treated with dignity and respect.
Members of the multidisciplinary team including external agencies, the patient and their family or carers should be aware of and involved in the admission, transfer, and discharge process in a timely manner.
All clinical and non-clinical colleagues involved in the admission, discharge or transfer of a patient to and from trust services, should ensure local and national guidance in relation to this are adhered to.
9.1.8 Care coordinator (mental health)
In line with the trust care programme approach (CPA) policy or equivalent, the care coordinator should stay involved throughout admission and support discharge planning. Where the care coordinator is not available, a deputy should be in place.
9.2 Appendix B monitoring arrangements
9.2.1 Admission or discharge experience
- How: review of complaints.
- Who by: Patient Safety and Investigations team.
- Reported to: care groups.
- Frequency: bi-monthly.
9.2.2 Admission or discharge experience
- How: Care Opinion forms.
- Who by: service managers.
- Reported to: care group quality meetings.
- Frequency: monthly.
9.2.3 Staff compliance with policy
- How: monitoring of admission documentation via management or clinical supervision.
- Who by: ward managers.
- Reported to: service managers escalated if required to care group nurse directors.
- Frequency: minimum bi-monthly.
9.3 Appendix C informal admission
This leaflet has been developed for those who are considering admission to hospital for assessment, care, and treatment of their mental health. As an informal patient there are certain considerations that you need to know before agreeing to admission.
As an informal patient you would be expected to actively participate with the clinical team involved in your care. This will involve doctors, nurses, and other health professionals. It is hoped that you will participate with the agreed treatment plan which could include medication, nursing and psychological interventions, occupational therapy, and specialist mental health care.
Occupational therapy and psychology sessions are also available, and you will be encouraged to attend these during your time on the ward.
With your agreement, and where appropriate, we would usually involve your family and friends in the development of your treatment plan.
9.3.1 Restrictions while in hospital
While in hospital you will be required to agree to some restrictions which may be necessary to keep you and other patients on the ward safe.
- As an informal patient you have the right to ask that you are discharged from hospital at any time. However, nursing staff will ask you to wait to see a doctor before you leave. If the care team do not believe that leaving hospital is in your best interests, or if they have concerns about your safety if you left hospital, they may arrange for you to be assessed under the Mental Health Act (1983).
- The doors to our wards are locked for security reasons and you will not be able to leave without discussion with a senior member of staff.
- Out of hours the doors to the mental health units are also locked for security reasons.
- You will usually be expected to stay on the ward for a minimum period of 72 hours to enable an assessment of your presenting mental health needs.
- The trust operates a smoke free policy in its premises and on its grounds, which you will be expected to adhere to. The use of disposable e-cigarettes is permitted by inpatients, which are available on the ward. These can only be used in designated outdoor spaces.
- The use of alcohol, any illegal substances or medication that is not prescribed for you is not permitted either on the ward or on the hospital grounds. If you are suspected to be under the influence of any illegal substance you may be breathalysed and, or requested to provide a supervised urine sample for drug screening. A positive test result could end in you being discharged from the ward. Restricted items will be removed and disposed of as per trust policy. This may potentially involve a report to the police.
- There are some items which you are not able to bring onto the ward or keep in your room. These are known as blanket restrictions, which include weapons and sharp items. You will be asked if you have any particular items with you when you arrive at the ward.
- On arrival at the ward staff will carry out a search of your belongings to ensure both your own safety and the safety of others. Searches may also be carried out when you return to the ward from leave, if staff have any concerns regarding your health and safety and others. All this will be documented.
- Staff will carry out regular observations on the ward to ensure everyone’s safety and wellbeing is monitored. This means they will check where you are on the ward at least every hour, including during the night.
- There are fixed mealtimes on the wards. You are welcome to bring snacks onto the ward but due to health and safety reasons you are unable to re-heat any food items or keep food in your bedroom. We will safely store such items for you in the kitchen area of the ward.
- Visiting times are restricted. This is to support treatment plans and protected mealtimes. We ask that visits do not coincide with mealtimes wherever possible. You need to ask ward staff if visits are needed outside visiting hours and exceptions can be made. You will need to speak to the nursing staff if you would like to arrange for children to visit.
- The trust operates a zero tolerance to aggressive, violent, or threatening behaviour and any incidents will be reported to the police and may result in you being discharged from the ward. You will be asked to consent to these restrictions.
9.4 Appendix D nursing admission checklist
Refer to appendix D: nursing admission checklist (staff access only).
9.5 Appendix E named nurse
Rotherham Doncaster and South Humber NHS Foundation Trust is committed to further improving the services it provides, whilst maintaining and re-affirming your rights in keeping with the patients’ charter.
The Patient’s charter (April 1992) states that:
“You should have a named, qualified nurse, midwife or health visitor who will be responsible for your nursing or midwifery care.” (National charter standard number 8).
This means that you will be allocated a named, qualified person who will be responsible for assessing, planning, implementing and evaluating your individualised needs and requirements, whether you are in hospital or in the community, taking into account your own and relatives’ or carers’ needs.
Rotherham Doncaster and South Humber NHS Foundation Trust staff will provide you with an information card which states:
- the name of your nurse
- the hospital or ward or department phone number
- the health centre or department phone number
- the time to contact (if in the community)
- the names of other professionals involved in your care
Your named nurse will have 24-hour responsibility for your care but obviously cannot be available for the whole of that period of time.
Therefore, when he or she goes off duty, you will be introduced to a nominated deputy who will maintain the continuity of your care.
Named nurses provide care for other patients as well as their own but will not have the overall 24-hour responsibilities.
The concept of a named nurse can and does apply in any setting. It is your right to know who is responsible for your care.
If you have any queries, do not hesitate to ask your named nurse or other health care worker involved in your care.
9.6 Appendix F evidence of legal authority to admit an informal patient checklist
Refer to appendix F: evidence of legal authority to admit an informal patient checklist (staff access only).
9.7 Appendix G recording of referrals and activity on SystmOne
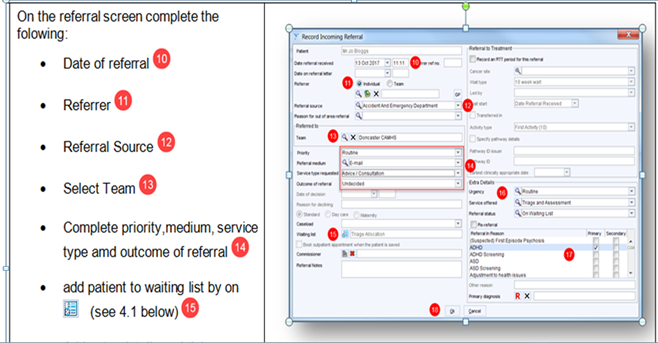
On the referral screen complete the following:
- date of referral (10)
- referrer (11)
- referral source (12)
- select team (13)
- complete priority, medium, service type and outcome of referral (14)
- add patient to waiting list on (see 4.1 below) (15)
13, team equals locality Child and adolescent mental health service (CAMHS) Crisis team the child presents at, for example, Scunthorpe Children and Young (CYP) Crisis team, Doncaster Children and Young People Crisis team or Rotherham Children and Young People Crisis team by A&E or emergency care centre locality.
14, priority equals very urgent for out of hours (or emergency if immediate threat to life).
Service type requested equals advice and consultation.
Complete outcome of referral to “accepted” if possible, if not task the relevant locality team to accept.
9.8 Appendix H adult and older persons mental health bed capacity
9.8.1 Doncaster bed capacity
9.8.1.1 Skelbrooke ward, psychiatric intensive care unit, Tickhill Road Hospital
-
Bed number
6
-
Phone
- 01302 798174
- 01302 798 175 (11176)
9.8.1.2 Brodsworth ward, acute adult assessment or treatment, Tickhill Road Hospital
-
Bed number
20
-
Phone
- 01302 798 060
- 01302 798 185 (11061)
9.8.1.3 Cusworth ward, acute adult assessment or treatment, Tickhill Road Hospital
-
Bed number
20
-
Phone
- 01302 798 170
- 01302 798 171 (11170)
9.8.1.4 Windermere Lodge, assessment or treatment for older people with an organic or functional mental illnesses, Tickhill Road Hospital
-
Bed number
20
-
Phone
01302 796 087 (14086)
9.8.2 Rotherham best capacity
9.8.2.1 Kingfisher ward, psychiatric intensive care unit, Swallownest Court
-
Bed number
5
-
Phone
01709 447 443 (15521)
9.8.2.2 Sandpiper ward, acute adult assessment or treatment, Swallownest Court
-
Bed number
18
-
Phone
01709 447 442 (15531)
9.8.2.3 Osprey ward, acute adult assessment or treatment, Swallownest Court
-
Bed number
18
-
Phone
01709 447 441 (15529)
9.8.2.4 The Willows, assessment or treatment for older people with an organic mental illness, The Woodlands
-
Bed number
15
-
Phone
01709 447 003 (15601)
9.8.2.5 Brambles ward, assessment or treatment for older people with a functional mental illness, The Woodlands
-
Bed number
15
-
Phone
01709 447 002 (15611)
9.8.3 North Lincolnshire bed capacity
9.8.3.1 Mulberry ward, acute adult assessment or treatment, Great Oaks
-
Bed number
17
-
Phone
01724 382 077 (16011)
9.8.3.2 Laurel ward, assessment or treatment for older people with organic and functional mental illnesses, Great Oaks
-
Bed number
13
-
Phone
01724 382 054 (16166)
9.9 Appendix I ward transfer checklist
Refer to appendix I: ward transfer checklist (staff access only).
9.10 Appendix J adult mental health and older persons process for arranging and authorising out of area placements
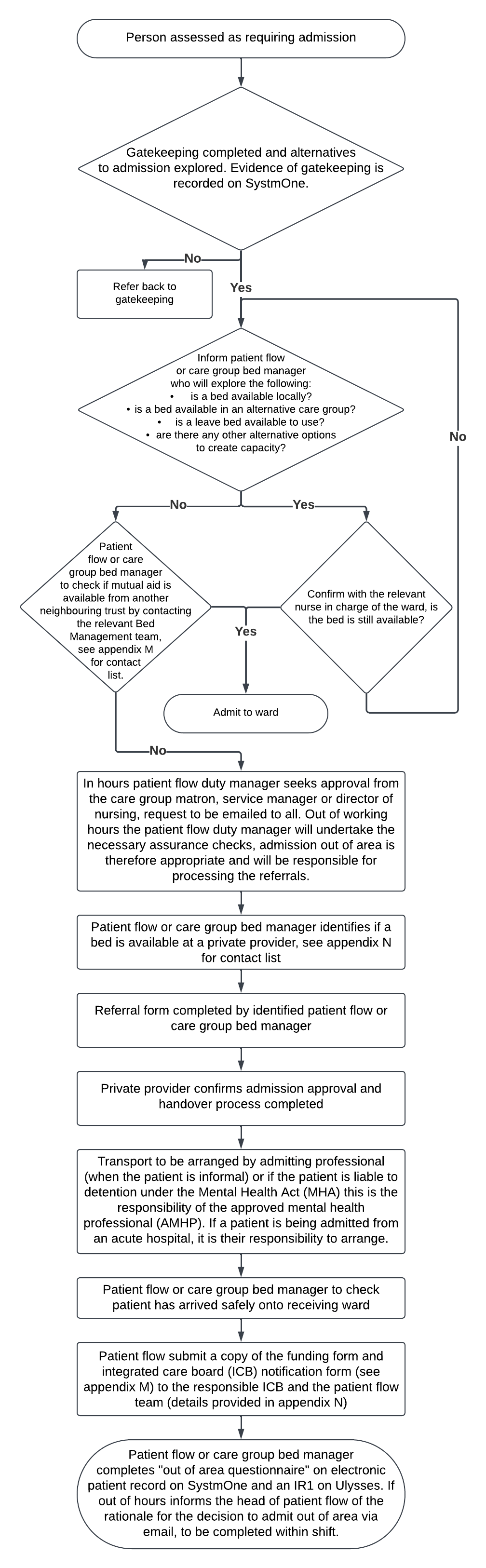
- Person assessed as requiring admission.
- Gatekeeping completed and alternatives to admission explored. Evidence of gatekeeping is recorded on SystmOne.
- no, refer to gatekeeping
- Yes, inform patient flow or care group bed manager who will explore the following:
- is a bed available locally?
- is a bed available in an alternative care group?
- is a leave bed available to use?
- are there any other alternative options to create capacity?
- Yes, confirm with the relevant nurse in charge of the ward, is the bed is still available?
- Yes, admit to ward
- Yes, confirm with the relevant nurse in charge of the ward, is the bed is still available?
- No, patient flow or care group bed manager to check if mutual aid is available from another neighbouring trust by contacting the relevant Bed Management team, see appendix M for contact list.
- Yes, admit to ward
- No, in hours patient flow duty manager seeks approval from the care group matron, service manager or director of nursing, request to be emailed to all. Out of working hours the patient flow duty manager will undertake the necessary assurance checks, admission out of area is therefore appropriate and will be responsible for processing the referrals.
- Patient flow or care group bed manager identifies if a bed is available at a private provider, see appendix N for contact list.
- Referral form completed by identified patient flow or care group bed manager.
- Private provider confirms admission approval and handover process completed.
- Transport to be arranged by admitting professional (when the patient is informal) or if the patient is liable to detention under the Mental Health Act (MHA) this is the responsibility of the approved mental health professional (AMHP). If a patient is being admitted from an acute hospital, it is their responsibility to arrange.
- Patient flow or care group bed manager to check patient has arrived safely onto receiving ward.
- Patient flow submit a copy of the funding form and integrated care board (ICB) notification form (see appendix M) to the responsible integrated care board and the patient flow team (details provided in appendix N).
- Patient flow or care group bed manager completes “out of area questionnaire” on electronic patient record on SystmOne and on the incident reporting system. If out of hours informs the head of patient flow of the rationale for the decision to admit out of area via email, to be completed within shift.
9.11 Appendix K mutual aid contact details
9.11.1 Berkshire Healthcare NHS Foundation Trust bed management
-
Phone
9.11.2 Black Country Healthcare NHS Foundation trust bed management
-
Phone
9.11.3 Cheshire and Wirral Partnership NHS Foundation Trust patient flow
-
Switchboard
9.11.4 Coventry and Warwickshire Partnership NHS Trust bed management
-
Phone
-
Switchboard
9.11.5 Cornwall Partnership NHS Foundation Trust bed coordination
-
Phone
9.11.6 Essex Partnership University NHS Foundation Trust bed management north
-
Phone
-
Email
9.11.7 Devon Partnership University NHS Trust bed capacity
-
Phone
9.11.8 Greater Manchester mental health services patient flow
-
Phone
9.11.9 Hertfordshire Partnership University NHS Foundation Trust bed management
-
Phone
9.11.10 Humber Teaching NHS Foundation Trust bed management
-
Phone
9.11.11 Lancashire and South Cumbria NHS Foundation trust hub
-
Phone
9.11.12 Lancashire and South Cumbria NHS Foundation trust administrator
-
Phone
9.11.13 Lincolnshire Partnership Foundation Trust bed management
-
Phone
9.11.14 Midlands Partnership NHS Foundation Trust Redwoods centre
-
Phone
-
Switchboard
9.11.15 Navigo (North East Lincolnshire Mental health Access team)
-
Phone
9.11.16 Norfolk and Suffolk NHS Foundation Trust bed management
-
Phone
-
Email
9.11.17 Nottinghamshire Healthcare NHS Foundation Trust bed management
-
Phone
-
Email
9.11.18 Rotherham, Doncaster and South Humber NHS Foundation Trust patient flow
-
Phone
9.11.19 Sheffield Health and Social Care Trust patient flow
-
Phone
9.11.20 Somerset NHS Foundation Trust urgent care hub
-
Phone
-
Switchboard
9.11.21 South London and Maudsley NHS Foundation Trust bed management
-
Phone
-
Email
9.11.22 South West Yorkshire Partnership NHS Foundation Trust patient flow
-
Phone
-
Out of hours
9.11.23 Tees, Esk and Wear Valleys NHS Foundation Trust Crisis team
Phone
9.11.24 West London NHS Foundation Trust
-
Phone
9.12 Appendix L private providers contact details
9.12.1 Mutual aid contact details in hours
9.12.1.1 Cygnet
-
Phone
-
Email
9.12.1.2 Elysium
-
Phone
9.12.1.3 Priory
-
Phone
-
Email
9.12.1.4 St Andrew’s
-
Phone
-
Email
Different email addresses for different hospitals.
9.12.1.5 Elizabeth house
-
Phone
9.12.1.6 Southern hill
-
Phone
9.13 Appendix M integrated care board (ICB) notification and funding form submission details
9.13.1 Trust notification contact details
Corporate, Patient Flow team, patient flow managers
9.13.2 Integrated care board notification contact details
Doncaster
9.14 Appendix N out of area patient integrated care board (ICB) notification form
Refer to appendix N: out of area patient integrated care board (ICB) notification form (staff access only).
9.15 Appendix O adult mental health and older persons out of area (OOA) placement monitoring process
The adult mental health and older persons out of area (OOA) placement monitoring process flow chart provides oversight of the monitoring requirements for all patients placed in either an inappropriate or appropriate placement external to the trust.
An inappropriate out of area placement occurs when clinical demand for an inpatient bed exceeds the trust bed stock availability and therefore patients need to be accommodated in an alternative NHS or private sector setting.
An out of area placement may on occasion be defined as appropriate if a patient requires their needs to be met in a particular environment due to risk, for example, a male only psychiatric intensive care physical environment (PICU) or if a patient is close to discharge and elects to remain out of area for continuity of care.
Specialist placements refer to care provision outside the trust services, for example, secure and locked rehab and are therefore outside the scope of this flow chart.
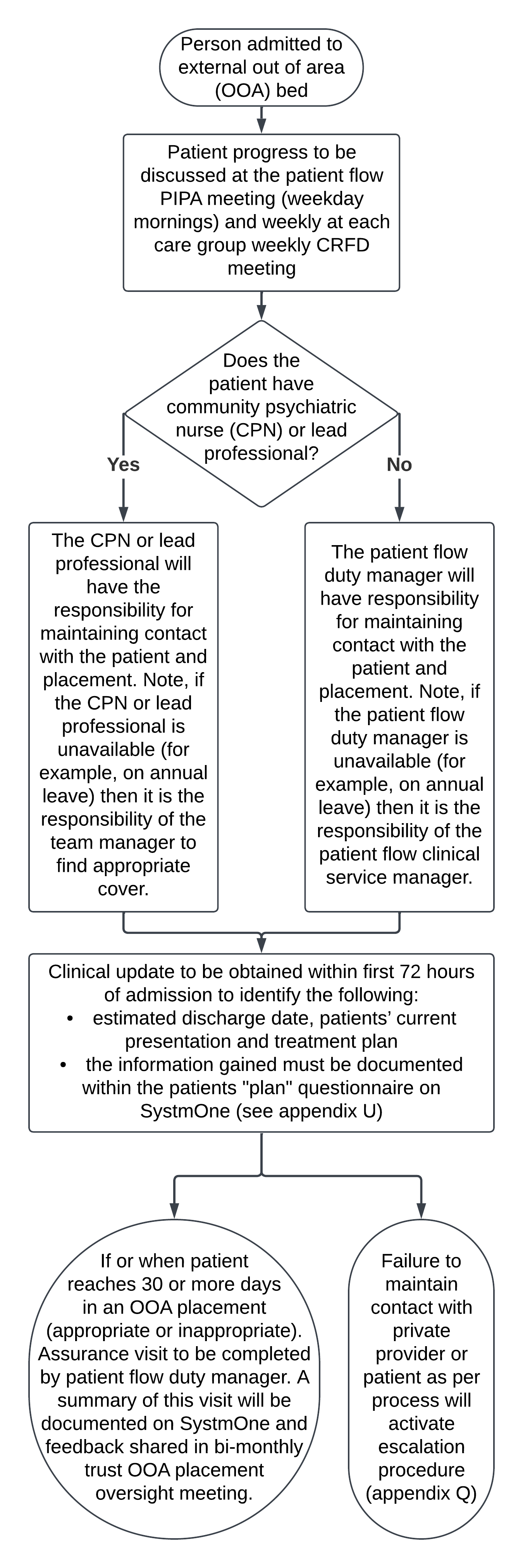
- Person admitted to external out of area (OOA) bed.
- Patient progress to be discussed at the patient flow PIPA meeting (weekday mornings) and weekly at each care group weekly CRFD meeting.
- Does the patient have community psychiatric nurse (CPN) or lead professional?
- Yes, the community psychiatric nurse or lead professional will have the responsibility for maintaining contact with the patient and placement. Note, if the community psychiatric nurse or lead professional is unavailable (for example, on annual leave) then it is the responsibility of the team manager to find appropriate cover.
- No, the patient flow duty manager will have responsibility for maintaining contact with the patient and placement. Note, if the patient flow duty manager is unavailable (for example, on annual leave) then it is the responsibility of the patient flow clinical service manager.
- Clinical update to be obtained within first 72 hours of admission to identify the following:
- estimated discharge date, patients’ current presentation and treatment plan
- the information gained must be documented within the patients’ “plan” questionnaire on SystmOne (see appendix U)
- If or when patient reaches 30 or more days in an out of area placement (appropriate or inappropriate). Assurance visit to be completed by patient flow duty manager. A summary of this visit will be documented on SystmOne and feedback shared in bi-monthly trust out of area placement oversight meeting.
- Failure to maintain contact with private provider or patient as per process will activate escalation procedure (appendix Q).
9.16 Appendix P how to document clinical updates
Data capture for out of area placement (OAP) is completed using 4 questionnaires within SystmOne, admission, transfer, discharge and plan.
9.16.1 Adult units
The questionnaires can be located on the Clinical Tree, on a node called “out of area placement”. All of the questionnaires are in one place. This node is located just under care planning or multidisciplinary team on each unit.
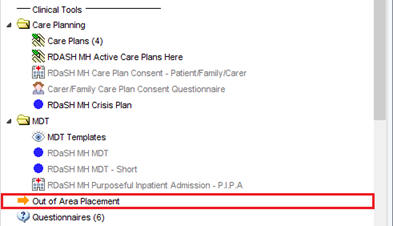
Once you click on the node, there are four buttons:
- admission
- transfer
- discharge
- plan
Upon any of the first three being completed, a task will be sent automatically to the Patient Flow team for information. All of the fields in these three questionnaires are now mandatory to aid data quality.
The fourth questionnaire (plan) is used to record discussions with out-of-area providers, or the patient, and considerations of repatriation.
Once a questionnaire has been completed, they’ll go under the corresponding section. To view these, either right click and select “View Questionnaire” or use the little triangle on the left side:
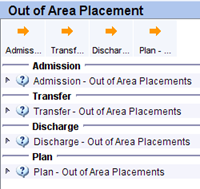 Refer to out of area placement tutorial (staff access only).
Refer to out of area placement tutorial (staff access only).
9.17 Appendix Q Escalation procedure
- Appropriate professional to obtain initial update within 72 hours of
admission - Update obtained by Patient Flow team and sent to relevant community team along with any multi-disciplinary team dates and key information
- Failure to obtain update within 72 hours of admission or since last
contact will be escalated to the service manager by the Patient Flow
team. - Failure to obtain update within 7 days of admission or since last
contact will be escalated to the director of nursing by the Patient Flow team. - The Patient Flow team to report as an incident on the incident reporting system.
9.18 Appendix R ward closure procedure adult and older adults mental health
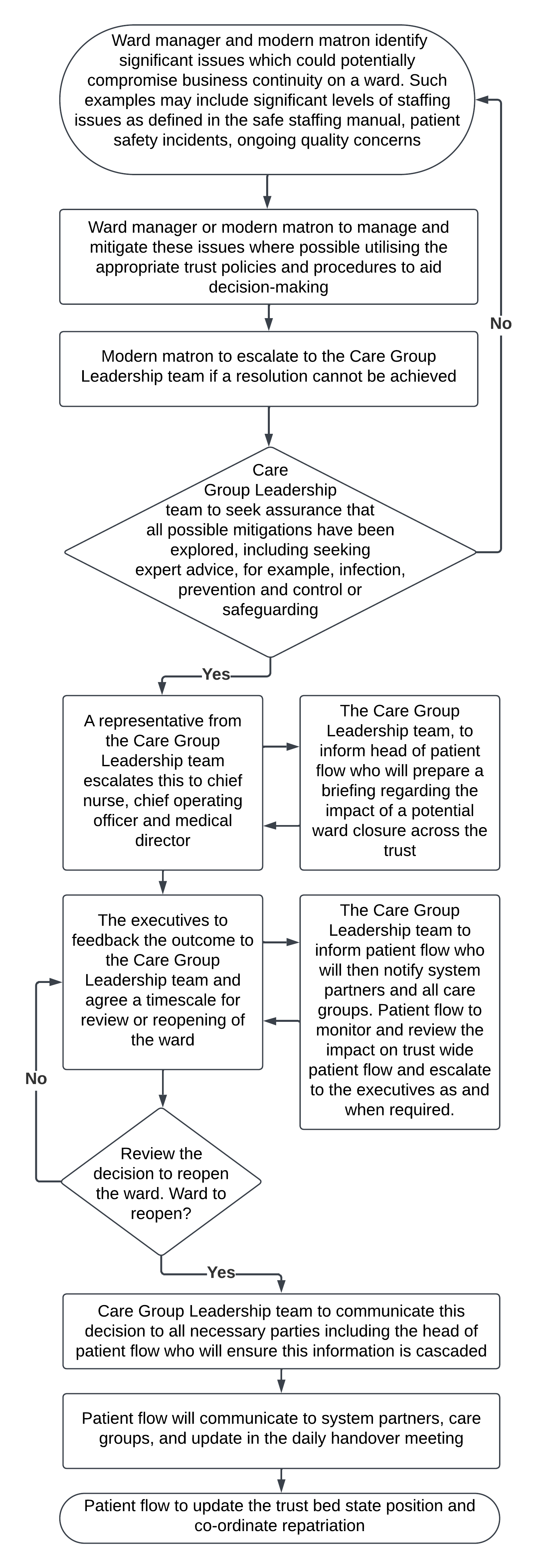
- Ward manager and modern matron identify significant issues which could potentially compromise business continuity on a ward
Such examples may include significant levels of staffing issues as defined in the safe staffing manual, patient safety incidents, ongoing quality concerns. - Ward manager or modern matron to manage and mitigate these issues where possible utilising the appropriate trust policies and procedures to aid decision-making.
- Modern matron to escalate to the Care Group Leadership team if a resolution cannot be achieved.
- Care Group Leadership team to seek assurance that all possible mitigations have been explored, including seeking
expert advice, for example, infection, prevention and control or safeguarding.- No, proceed back to step 1 and repeat process
- Yes, A representative from the Care Group Leadership team escalates this to chief nurse, chief operating officer and medical director: the Care Group Leadership team, to inform head of patient flow who will prepare a briefing regarding the impact of a potential ward closure across the trust
- The executives to feedback the outcome to the Care Group Leadership team and agree a timescale for review or reopening of the ward: the Care Group Leadership team to inform patient flow who will then notify system partners and all care groups. Patient flow to monitor and review the impact on trust wide patient flow and escalate to the executives as and when required
- Review the decision to reopen the ward. Ward to reopen?
- No, proceed back to step 6 and repeat process
- Yes, Care Group Leadership team to communicate this decision to all necessary parties including the head of patient flow who will ensure this information is cascaded.
- Patient flow will communicate to system partners, care groups, and update in the daily handover meeting.
- Patient flow to update the trust bed state position and co-ordinate repatriation.
9.19 Appendix S Rockwood frailty scale
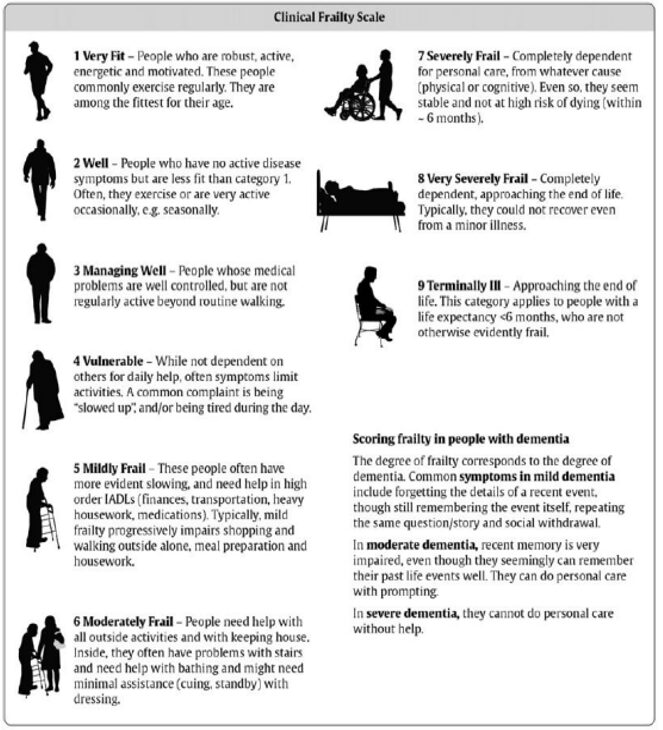
Adapted with the permission from Moorhouse P, Rockwood K. Frailty and its quantitative clinical evaluation Royal Collage Physicians Edinburgh. 2012. 42:333 to 340.
- Very fit, people who are robust, active, energetic and motivated. These people commonly exercise regularly. They are among the fittest for their age.
- Well, people who have no active disease symptoms but are less fit than category 1. Often, they exercise or are very active occasionally, for example, seasonally.
- Managing well, people whose medical problems are well controlled, but are not regularly active beyond routine walking.
- Vulnerable, while not dependent on others for daily help, often symptoms limit activities. A common complaint is being “slowed up”, and, or being tired during the day.
- Mildly frail, these people often have more evident slowing and need help in high order instrumental activity of daily livings (IADLs) (finances, transportation, heavy housework, medications). Typically, mild frailty progressively impairs shopping and walking outside alone, meal preparation and housework.
- Moderately frail, people need help with all outside activities and with keeping house. Inside, they often have problems with stairs and need help with bathing and might need minimal assistance (cuing, standby) with dressing.
- Severely frail, completely dependent for personal care, from whatever cause (physical or cognitive). Even so, they seem stable and not at high risk of dying (within 6 months).
- Very severely frail, completely dependent, approaching the end of life. Typically, they could not recover even from a minor illness.
- Terminally iII, approaching the end of life. This category applies to people with a life expectancy less than 6 months, who are not otherwise evidently frail.
9.19.1 Scoring frailty in people with dementia
The degree of frailty corresponds to the degree of dementia. Common symptoms in mild dementia include forgetting the details of a recent event, though still remembering the event itself, repeating the same question or story and social withdrawal.
In moderate dementia, recent memory is very impaired, even though they seemingly can remember their past life events well. They can do personal care with prompting.
In severe dementia, they cannot do personal care without help.
Please note as advised by the NHS specialised clinical frailty network the clinical frailty scale has not been widely validated in younger populations (below 65 years of age), or in those with learning disability. It may not perform as well in people with stable long-term disability such as cerebral palsy, whose outcomes might be very different compared to older people with progressive disability. It is therefore to be used to support decision-making in the context of this procedure as in the round it will be part of a wider and more holistic assessment of need. Further information can be found at the NHS specialised clinical frailty network.
9.20 Appendix T taxi booking form
Refer to appendix T: taxi booking form (staff access only).
9.21 Appendix U 72-hour follow-up technical guide
Refer to appendix U: 72-hour follow-up technical guide.
9.22 Appendix V private ambulance secure transport request form
Refer to appendix V: private ambulance secure transport request form.
Document control
- Version: 4.
- Unique reference number: 1006.
- Approved by: Clinical Effectiveness Group.
- Date approved: 7 October 2025.
- Name of originator or author: head of patient flow.
- Name of responsible committee or individual: chief operating officer.
- Date issued: 10 February 2026.
- Review date: 31 October 2028.
Page last reviewed: February 24, 2026
Next review due: February 24, 2027
Problem with this page?
Please tell us about any problems you have found with this web page.
Report a problem